Abstract
Background
Elevated levels of the extracellular matrix glycoprotein osteopontin (OPN) may be detected in both myocardium and plasma under various pathological conditions affecting the heart. Several studies demonstrated increased plasma OPN levels in patients with heart failure due to dilated cardiomyopathy (DCM), while other studies showed high OPN expression levels in the myocardium of such patients. However, very little is known about OPN levels in both plasma and myocardium of the same individual with DCM. Therefore, we aimed to compare plasma OPN levels and levels of myocardial OPN expression in patients with recent-onset DCM (Ro-DCM).
Methods
We examined plasma OPN as well as creatinine, C‑reactive protein (CRP), brain natriuretic peptide (BNP), and troponin I levels in 25 patients with Ro-DCM. Furthermore, all subjects underwent transthoracic echocardiography, selective coronary angiography, and endomyocardial biopsy (EMB) for the assessment of myocardial OPN expression.
Results
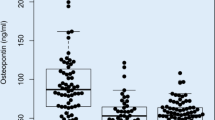
No significant correlation between myocardial OPN expression and clinical, biochemical, or echocardiographic parameters was found. In log transformation analysis, plasma OPN levels correlated significantly with BNP levels (r = 0.46, p = 0.031), with CRP levels (r = 0.52, p = 0.015), and with early diastolic mitral annular velocity (r = −0.57, p = 0.009). There was a borderline association between the plasma OPN log value and New York Heart Association class (p = 0.053).
Conclusion
Plasma OPN levels reflect heart failure severity in patients with Ro-DCM. Myocardial OPN expression is not associated with either plasma OPN levels or markers of heart failure in these individuals.
Zusammenfassung
Hintergrund
Erhöhte Spiegel des extrazellulären Matrixglykoproteins Osteopontin (OPN) sind bei verschiedenen pathologischen Veränderungen des Herzens sowohl im Myokard als auch im Plasma nachweisbar. In mehreren Studien wurden bei Patienten mit Herzinsuffizienz aufgrund dilatativer Kardiomyopathie (DCM) erhöhte OPN-Plasmaspiegel festgestellt, während sich in anderen Studien hohe OPN-Expressionswerte im Myokard solcher Patienten zeigten. Jedoch ist nur sehr wenig über die OPN-Werte sowohl im Plasma als auch im Myokard desselben Patienten mit DCM bekannt. Daher war es Ziel der Studie, die OPN-Plasmawerte und die Werte der myokardialen OPN-Expression bei Patienten mit seit Kurzem bestehender DCM („recent onset DCM“, Ro-DCM) zu vergleichen.
Methoden
Dazu wurden die Werte für OPN im Plasma, Kreatinin, C‑reaktives Protein (CRP), BNP („brain natriuretic peptide“) und Troponin I bei 25 Patienten mit Ro-DCM bestimmt. Außerdem erfolgte bei allen Teilnehmern eine transthorakale Echokardiographie, selektive Koronarangiographie und Endomyokardbiopsie (EMB) zur Bestimmung der myokardialen OPN-Expression.
Ergebnisse
Zwischen myokardialer OPN-Expression und klinischen, biochemischen oder echokardiographischen Parametern fand sich keine signifikante Korrelation. In der Log-Transformationsanalyse waren die OPN-Werte im Plasma signifikant mit den BNP-Werten (r = 0,46; p = 0,031), den CRP-Werten (r = 0,52; p = 0,015) und der frühdiastolischen Mitralringgeschwindigkeit korreliert (r = −0,57; p = 0,009). Ein grenzwertiger Zusammenhang bestand zwischen dem Plasma-OPN-Log-Wert und der Klasse nach New York Heart Association (p = 0,053).
Schlussfolgerung
Die OPN-Werte im Plasma widerspiegeln den Schweregrad der Herzinsuffizienz bei Patienten mit Ro-DCM. Dagegen ist die myokardiale OPN-Expression weder mit den OPN-Werten im Plasma noch mit Markern der Herzinsuffizienz bei diesen Patienten assoziiert.



Similar content being viewed by others
References
Lakdawala NK, Winterfield JR, Funke BH (2013) Dilated cardiomyopathy. Circ Arrhythm Electrophysiol 6:228–237
Weintraub RG, Semsarian C, Macdonald P (2017) Dilated cardiomyopathy. Lancet 390:400–414. https://doi.org/10.1016/S0140-6736(16)31713-5
Rubis P (2015) The diagnostic work up of genetic and inflammatory dilated cardiomyopathy. An article from the e‑journal of the ESC Council for Cardiology Practice. https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-13/The-diagnostic-work-up-of-genetic-and-inflammatory-dilated-cardiomyopathy. Accessed 7 Apr 2015
Bielecka-Dabrowa A, Wierzbicka M, Dabrowa M, Goch A (2008) New methods in laboratory diagnostics of dilated cardiomyopathy. Cardiol J 15:388–395
Oldberg A, Franzén A, Heinegård D (1986) Cloning and sequence analysis of rat bone sialoprotein (osteopontin) cDNA reveals an Arg-Gly-Asp cell-binding sequence. Proc Natl Acad Sci USA 83:8819–8823
Mazzali M, Kipari T, Ophascharoensuk V et al (2002) Osteopontin—a molecule for all seasons. QJM 95:3–13
>O’Regan AW, Chupp GL, Lowry JA et al (1999) Osteopontin is associated with T cell in sarcoid granulomas and has T cell adhesive and cytokine-like properties in vitro. J Immunol 162:1024–1031
Klingel K, Kandolf R (2010) Osteopontin: a biomarker to predict the outcome of inflammatory heart disease. Semin Thromb Hemost 36:195–202. https://doi.org/10.1055/s-0030-1251504
Singh M, Dalal S, Singh K (2014) Osteopontin: At the cross-roads of myocyte survival and myocardial function. Life Sci 118:1–6. https://doi.org/10.1016/j.lfs.2014.09.014
Podzimkova J, Palecek T, Kuchynka P et al (2017) Plasma osteopontin levels in patients with dilated and hypertrophic cardiomyopathy. Herz. https://doi.org/10.1007/s00059-017-4645-3
Rosenberg M, Zugck C, Nelles M et al (2008) Osteopontin, a new prognostic biomarker in patients with chronic heart failure. Circ Heart Fail 1:43–49. https://doi.org/10.1161/CIRCHEARTFAILURE.107.746172
Soeijma H, Irie A, Fukunaga T et al (2007) Osteopontin expression of circulating T cells and plasma Osteopontin levels are increased in relation to severity of heart failure. Circ J 71:1879–1884
Stawowy P, Blaschke F, Pfautsch P et al (2002) Increased myocardial expression of osteopontin in patients with advanced heart failure. Eur J Heart Fail 4:139–146
Satoh M, Nakamura M, Akatsu T et al (2005) Myocardial osteopontin expression is associated with collagen fibrillogenesis in human dilated cardiomyopathy. Eur J Heart Fail 7:755–762. https://doi.org/10.1016/j.ejheart.2004.10.019
Cabiati M, Svezia B, Matteucci M et al (2016) Myocardial expression analysis of osteopontin and its splice variants in patients affected by end-stage idiopathic or Ischemic dilated cardiomyopathy. PLoS ONE 11(8):e160110. https://doi.org/10.1371/journal.pone.0160110
Elliott P, Andersson B, Arbustini E et al (2008) Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 29:270–276. https://doi.org/10.1093/eurheartj/ehm342
Caforio AL, Pankuweit S, Arbustini E et al (2013) European society of cardiology working group on myocardial and pericardial diseases. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on myocardial and pericardial diseases. Eur Heart J 34:2636–2648. https://doi.org/10.1093/eurheartj/eht210
Ponikowski P, Voors AA, Anker DS et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular imaging. Eur Heart J Cardiovasc Imaging 16:233–270. https://doi.org/10.1093/ehjci/jev014
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Evaluation of left ventricular diastolic function by echocardiography: EAE/ASE Recommendations. Eur J Echocardiogr 10:165–193. https://doi.org/10.1093/ejechocard/jep007
Rudski LG, Lai WW, Afilalo J et al (2010) Echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713. https://doi.org/10.1016/j.echo.2010.05.010
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Livac KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2− ∆∆CT method. Methods 4:402–408
Schipper ME, Scheenstra MR, van Kuik J et al (2011) Osteopontin: a potential biomarker for heart failure and reverse remodeling after left ventricular assist device support. J Heart Lung Transpl 30:805–810. https://doi.org/10.1016/j.healun.2011.03.015
López B, González A, Lindner D et al (2013) Osteopontin-mediated myocardial fibrosis in heart failure: a role for lysyl oxidase? Cardiovasc Res 99:111–120. https://doi.org/10.1093/cvr/cvt100
Tamura A, Shingai M, Aso N et al (2003) Osteopontin is released from the heart into the coronary circulation in patients with a previous anterior wall myocardial infarction. Circ J 67:742–744
Trueblood NA, Xie Z, Communal C et al (2001) Exaggerated left ventricular dilatation and reduced collagen deposition after myocardial infarction in mice lacking osteopontin. Circ Res 88:1080–1087
Dick SA, Epelman S (2016) Chronic heart failure and inflammation: what do we really know? Circ Res 119:159–176. https://doi.org/10.1161/CIRCRESAHA.116.308030
Anker SD, von Haehling S (2004) Inflammatory mediators in chronic heart failure: an overview. Heart 90:464–470. https://doi.org/10.1136/hrt.2002.007005
Anand IS, Latini R, Florea VG et al (2005) C‑reactive protein in heart failure. Prognostic value and the effect of valsartan. Circulation 112:1428–1434. https://doi.org/10.1161/CIRCULATIONAHA.104.508465
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Waggoner AD recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17:1321–1360
Acknowledgements
The authors are thankful to Ms. Hana Rehakova form the Institute of Medical Biochemistry and Laboratory Diagnostics for technical assistance
Funding
The study was supported by MH CZ DRO 64165, Progres Q25 and Q38/LF1 projects.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Podzimkova, T. Palecek, P. Kuchynka, J. Marek, B.A. Danek, M. Jachymova, M. Safarikova, M. Kalousova, T. Zima, and A. Linhart declare that they have no competing interests.
All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Podzimkova, J., Palecek, T., Kuchynka, P. et al. Plasma osteopontin levels, but not its myocardial expression, reflect heart failure severity in recently diagnosed dilated cardiomyopathy. Herz 45 (Suppl 1), 105–110 (2020). https://doi.org/10.1007/s00059-019-4829-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-4829-0