Abstract
Background
This study summarizes the clinical features of stroke in patients with prosthetic valve endocarditis (PVE) in China.
Methods
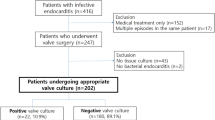
The clinical data of PVE patients admitted to Beijing Anzhen Hospital from January 1997 to August 2018 were retrospectively analyzed.
Results
In total, 62 patients with PVE were enrolled (45 males, 17 females). The patients’ age ranged from 23 to 79 years (51.69 ± 15.01). Rheumatic heart disease (RHD) was the most common reason for valve replacement. Of the patients, 58 were found to have vegetations by echocardiography. Blood cultures revealed the most common pathogens to be Staphylococcus (12 cases) and fungal infections (n = 7); 18 (29.03%) patients had strokes. There were 12 cases of ischemic stroke, three cases of cerebral hemorrhage, one case of subarachnoid hemorrhage, and two cases of unclear etiology. The most commonly found clinical symptoms of stroke patients were hemiplegia (n = 10) and coma (n = 5). The five patients in coma died during hospitalization. The incidence of RHD, double valve replacement, atrial fibrillation, and mitral valve vegetation was significantly higher in the stroke group than in the non-stroke group (p = 0.045, 0.000, 0.033, and 0.045, respectively). Logistic regression analysis showed that the odds ratios (ORs) for RHD, double valve replacement, and fungal infection as risk factors of stroke were 7.26 (95% CI: 1.23–42.68), 25.60 (95%CI: 4.33–126.16), and 20.58 (95% CI: 2.13–198.82), respectively, and were statistically significant. Eight patients died during hospitalization and the in-hospital mortality was 12.90%. The OR for in-hospital mortality with concurrent stroke was 5.13 (95% CI: 1.08–24.46, p = 0.028).
Conclusion
Stroke is a common complication in PVE that increases patient mortality. Rheumatic heart disease, double valve replacement, and fungal infection may be risk factors for patients with PVE complicated by stroke.
Zusammenfassung
Hintergrund
Der vorliegende Beitrag stellt klinische Merkmale des Schlaganfalls bei Patienten in China mit Klappenprothesenendokarditis (KPE) dar.
Methoden
Retrospektiv wurden von Januar 1997 bis August 2018 die klinischen Daten von KPE-Patienten, die ins Beijing Anzhen Hospital aufgenommen wurden, analysiert.
Ergebnisse
Insgesamt wurden 62 Patienten mit KPE in die Analyse einbezogen (45 m., 17 w.). Das Alter der Patienten betrug 23–79 Jahre (51,69 ± 15,01). Häufigster Grund für den Klappenersatz war eine rheumatische Herzerkrankung („rheumatic heart disease“, RHD). Bei 58 der Patienten wurden echokardiographisch Vegetationen festgestellt. Blutkulturen ergaben als häufigste Pathogene Staphylococcus (12 Fälle) und Pilzinfektionen (n = 7); 18 (29,03%) Patienten hatten einen Schlaganfall. Es gab 12 Fälle mit ischämischem Schlaganfall, 3 Fälle mit Zerebralblutung, einen Fall mit Subarachnoidalblutung und 2 Fälle unklarer Ätiologie. Häufigste klinische Symptome der Schlaganfallpatienten waren Hemiplegie (n = 10) und Koma (n = 5). Die 5 Patienten im Koma starben während der stationären Behandlung. Die Inzidenz von RHD, doppeltem Klappenersatz, Vorhofflimmern und Mitralklappenvegetationen war in der Schlaganfallgruppe signifikant höher als in der Gruppe ohne Schlaganfall (p =0,045; 0,000; 0,033 bzw. 0,045). Die logistische Regressionsanalyse ergab, dass die Odds Ratio (OR) für RHD, doppelten Klappenersatz und Pilzinfektion als Risikofaktoren des Schlaganfalls 7,26 (95%-KI: 1,23–42,68); 25,60 (95%-KI: 4,33–126,16) bzw. 20,58 (95%-KI: 2,13–198,82) betrug und statistisch signifikant war. Während der stationären Behandlung starben 8 Patienten, die Krankenhausmortalität lag bei 12,90%. Die OR für die Krankenhausmortalität bei gleichzeitigem Schlaganfall betrug 5,13 (95%-KI: 1,08–24,46; p = 0,028).
Schlussfolgerung
Ein Schlaganfall ist eine häufige Komplikation bei KPE und erhöht die Mortalität. Risikofaktoren für Patienten mit KPE und der Komplikation eines Schlaganfalls sind möglicherweise RHD, doppelter Klappenersatz und Pilzinfektionen.
Similar content being viewed by others
Change history
28 May 2019
<Emphasis Type="Bold">Erratum to:</Emphasis>
<Emphasis Type="Bold">Herz 2019</Emphasis>
<ExternalRef><RefSource>https://doi.org/10.1007/s00059-019-4809-4</RefSource><RefTarget Address="10.1007/s00059-019-4809-4" TargetType="DOI"/></ExternalRef>
The original article has been corrected. The data given in Table 4 for patient No. 13 were wrong. Please find here the corrected Table.
The authors and publisher apologize for this …
References
Wang A, Athan E, Pappas PA et al (2007) Contemporary clinical profile and outcome of prosthetic valve endocarditis. JAMA 297(12):1354–1361
Xie H, Hu B, Zhou C, Zhou Q, Gao X (2014) An analysis of clinical characteristics, etiologies and prognosis of 218 patients with infective endocarditis. Zhonghua Nei Ke Za Zhi 53(5):363–367
Lou XF, Yang DY, Liu ZY, Wang HL, Li TS (2009) Clinical analysis of 120 cases of infective endocarditis. Zhonghua Nei Ke Za Zhi 48(1):35–38
Baddour LM, Wilson WR, Bayer AS et al (2015) Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 132(15):1435–1486
Nonaka M, Kusuhara T, An K et al (2013) Comparison between early and late prosthetic valve endocarditis: clinical characteristics and outcomes. J Heart Valve Dis 22(4):567–574
Davenport J, Hart RG (1990) Prosthetic valve endocarditis 1976–1987. Antibiotics, anticoagulation, and stroke. Stroke 21(7):993–999
Wang HL, Fan HW, Fang LG et al (2010) A clinical analysis of 25 cases of prosthetic valve endocarditis. Zhonghua Nei Ke Za Zhi 49(9):758–761
Hannachi N, Béard T, Ben Ismail M (1991) Neurologic manifestations of infectious endocarditis. Arch Mal Coeur Vaiss 84(1):81–86
Wang D, Liu M, Lin S et al (2013) Stroke and rheumatic heart disease: a systematic review of observational studies. Clin Neurol Neurosurg 115(9):1575–1582
Kuwaki K, Tsukamoto M, Komatsu K, Morishita K, Sakata J, Abe T (2003) Simultaneous aortic and mitral valve replacement: predictors of adverse outcome. J Heart Valve Dis 12(2):169–176
Walls G, McBride S, Raymond N et al (2014) Infective endocarditis in New Zealand: data from the International Collaboration on Endocarditis Prospective Cohort Study. N Z Med J 127(1391):38–51
Melgar GR, Nasser RM, Gordon SM, Lytle BW, Keys TF, Longworth DL (1997) Fungal prosthetic valve endocarditis in 16 patients. An 11-year experience in a tertiary care hospital. Medicine (Baltimore) 76(2):94–103
Keyser DL, Biller J, Coffman TT, Adams HP Jr. (1990) Neurologic complications of late prosthetic valve endocarditis. Stroke 21(3):472–475
García-Cabrera E, Fernández-Hidalgo N, Almirante B et al (2013) Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation 127(23):2272–2284
Asaithambi G, Adil MM, Qureshi AI (2013) Thrombolysis for ischemic stroke associated with infective endocarditis: results from the nationwide inpatient sample. Stroke 44(10):2917–2919
Ambrosioni J, Urra X, Hernández-Meneses M et al (2018) Mechanical thrombectomy for acute ischemic stroke secondary to infective endocarditis. Clin Infect Dis 66(8):1286–1289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G.-F. Cao, W Liu, L. Cao, and Y. Wang declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case. This retrospective study was performed after consultation with the institutional ethics committee and in accordance with national legal requirements.
Additional information
The original version of this article was revised. The data given in Table 4 for patient No. 13 were published wrong.
Rights and permissions
About this article
Cite this article
Cao, GF., Liu, W., Cao, L. et al. Stroke in patients with prosthetic valve endocarditis. Herz 45 (Suppl 1), 72–77 (2020). https://doi.org/10.1007/s00059-019-4809-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-4809-4