Abstract
Background
The possible treatment strategies for defects of the pace-sense (P/S) part of a defibrillation lead are either implantation of a new high-voltage (HV)-P/S lead, with or without extraction of the malfunctioning lead, or implantation of a P/S lead.
Methods
We conducted a Web-based survey across cardiac implantable electronic device (CIED) centers to investigate their procedural practice and decision-making process in cases of failure of the P/S portion of defibrillation leads. In particular, we focused on the question of whether the integrity of the HV circuit is confirmed by a test shock before decision-making. The questionnaire included 14 questions and was sent to 951 German, 341 Austrian, and 120 Swiss centers.
Results
The survey was completed by 183 of the 1412 centers surveyed (12.7% response rate). Most centers (90.2%) do not conduct a test shock to confirm the integrity of the HV circuit before decision-making. Procedural practice in lead management varies depending on the presentation of lead failure and whether the center applies a test shock. In centers that do not conduct a test shock, the majority (69.9%) implant a new HV-P/S lead. Most centers (61.7%) that test the integrity of the HV system implant a P/S lead. The majority of centers favor DF-4 connectors (74.1%) over DF-1 connectors (25.9%) at first CIED implantation.
Conclusion
Either implanting a new HV-P/S lead or placing an additional P/S lead are selected strategies if the implantable cardioverter-defibrillator lead failure is localized to the P/S portion. However, conducting a test shock to confirm the integrity of the HV component is rarely performed.
Zusammenfassung
Hintergrund
Als Behandlungsstrategie bei Defekten des Pace-Sense(P/S)-Anteils einer Defibrillationselektrode sind entweder die Implantation einer neuen High-Voltage(HV)-P/S-Elektrode – mit oder ohne Extraktion der defekten Elektrode – oder die Implantation einer P/S-Elektrode möglich.
Methoden
Die Autoren führten eine webbasierte Erhebung in Zentren durch, in denen eine Therapie mit kardialen implantierbaren elektronischen Systemen („cardiac implantable electronic device“, CIED) erfolgt, um deren praktische Abläufe und Entscheidungsprozesse in Fällen mit einer Dysfunktion des P/S-Anteils von Defibrillationselektroden zu untersuchen. Insbesondere lag der Schwerpunkt auf der Frage, ob die Integrität des HV-Stromkreislaufs vor dem Treffen einer Entscheidung durch einen Testschock bestätigt würde. Der Fragebogen beinhaltete 14 Fragen und wurde 951 deutschen, 341 österreichischen und 120 Schweizer Zentren zugeschickt.
Ergebnisse
Die Umfrage wurde von 183 der 1412 angeschriebenen Zentren beantwortet (12,7 % Antwortrate). Die meisten Zentren (90,2 %) führen keinen Testschock zur Bestätigung der Integrität des HV-Stromkreislaufs vor dem Treffen einer Entscheidung durch. Die praktischen Abläufe im Hinblick auf die medizinische Versorgung variieren je nach entsprechender Ausprägung der Elektrodendysfunktion und abhängig davon, ob das jeweilige Zentrum mit einem Testschock arbeitet. In Zentren, die keinen Testschock geben, implantiert die Mehrheit (69,9 %) eine neue HV-P/S-Elektrode. Die meisten Zentren (61,7 %), welche die Integrität des HV-Systems prüfen, implantieren eine P/S-Elektrode. Die Mehrheit der Zentren bevorzugt DF-4-Konnektoren (74,1 %) vor DF-1-Konnektoren (25,9 %) bei der ersten CIED-Implantation.
Schlussfolgerung
Die Implantation einer neuen HV-P/S-Elektrode oder die Platzierung einer zusätzlichen P/S-Elektrode stellen die ausgewählten Strategien dar, wenn das Versagen der ICD-Elektroden im P/S-Anteil lokalisiert ist. Jedoch wird nur selten ein Testschock zur Bestätigung der Integrität der HV-Komponente gegeben.





Similar content being viewed by others
References
Padeletti L, Mascioli G, Perini AP, Grifoni G, Perrotta L, Marchese P, Bontempi L, Curnis A (2011) Critical appraisal of cardiac implantable electronic devices: complications and management. Med Devices (Auckl) 4:157–167
Kawada S, Nishii N, Morimoto Y, Miyoshi A, Tachibana M, Sugiyama H, Nakagawa K, Watanabe A, Morita H, Ito H (2017) Comparison of longevity and clinical outcomes of implantable cardioverter-defibrillator leads among manufacturers. Heart Rhythm 14(10):1496–1503
Kleemann T, Becker T, Doenges K, Vater M, Senges J, Schneider S, Saggau W, Weisse U, Seidl K (2007) Annual rate of transvenous defibrillation lead defects in implantable cardioverter-defibrillators over a period of > 10 years. Circulation 115(19):2474–2480
Swerdlow CD, Kalahasty G, Ellenbogen KA (2016) Implantable cardiac defibrillator lead failure and management. J Am Coll Cardiol 67(11):1358–1368
Eckstein J, Koller MT, Zabel M, Kalusche D, Schaer BA, Osswald S, Sticherling C (2008) Necessity for surgical revision of defibrillator leads implanted long-term: causes and management. Circulation 117(21):2727–2733
van Rees JB, van Welsenes GH, Borleffs CJ, Thijssen J, van der Velde ET, van der Wall EE, van Erven L, Schalij MJ (2012) Update on small-diameter implantable cardioverter-defibrillator leads performance. Pacing Clin Electrophysiol 35(6):652–658
Providencia R, Kramer DB, Pimenta D, Babu GG, Hatfield LA, Ioannou A, Novak J, Hauser RG, Lambiase PD (2015) Transvenous Implantable Cardioverter-Defibrillator (ICD) lead performance: a meta-analysis of observational studies. J Am Heart Assoc 4(11):e2418
Dorwarth U, Frey B, Dugas M, Matis T, Fiek M, Schmoeckel M, Remp T, Durchlaub I, Gerth A, Steinbeck G, Hoffmann E (2003) Transvenous defibrillation leads: high incidence of failure during long-term follow-up. J Cardiovasc Electrophysiol 14(1):38–43
Holubec T, Ursprung G, Schonrath F, Caliskan E, Steffel J, Falk V, Benussi S, Maisano F, Starck CT (2015) Does implantation technique influence lead failure? Acta Cardiol 70(5):581–586
Krahn AD, Champagne J, Healey JS, Cameron D, Simpson CS, Thibault B, Mangat I, Tung S, Sterns L, Birnie DH, Exner DV, Parkash R, Sivakumaran S, Davies T, Coutu B, Crystal E, Wolfe K, Verma A, Stephenson EA, Sanatani S, Gow R, Connors S, Paredes FA, Essebag V, Canadian Heart Rhythm Society Device Advisory C (2008) Outcome of the Fidelis implantable cardioverter-defibrillator lead advisory: a report from the Canadian Heart Rhythm Society Device Advisory Committee. Heart Rhythm 5(5):639–642
Parkash R, Tung S, Champagne J, Healey JS, Thibault B, Cameron D, Tang A, Connors S, Beardsall M, Mangat I, Ayala-Paredes F, Toal S, Exner D, Yee R, Krahn AD (2015) Insight into the mechanism of failure of the Riata lead under advisory. Heart Rhythm 12(3):574–579
Lin G, Nishimura RA, Connolly HM, Dearani JA, Sundt TM 3rd, Hayes DL (2005) Severe symptomatic tricuspid valve regurgitation due to permanent pacemaker or implantable cardioverter-defibrillator leads. J Am Coll Cardiol 45(10):1672–1675
Polewczyk A, Kutarski A, Tomaszewski A, Brzozowski W, Czajkowski M, Polewczyk M, Janion M (2013) Lead dependent tricuspid dysfunction: analysis of the mechanism and management in patients referred for transvenous lead extraction. Cardiol J 20(4):402–410
Buiten MS, van der Heijden AC, Schalij MJ, van Erven L (2015) How adequate are the current methods of lead extraction? A review of the efficiency and safety of transvenous lead extraction methods. Europace 17(5):689–700
Wollmann CG, Bocker D, Loher A, Kobe J, Scheld HH, Breithardt GE, Gradaus R (2005) Incidence of complications in patients with implantable cardioverter/defibrillator who receive additional transvenous pace/sense leads. Pacing Clin Electrophysiol 28(8):795–800
Scott PA, Chungh A, Zeb M, Yue AM, Roberts PR, Morgan JM (2010) Is the use of an additional pace/sense lead the optimal strategy for the avoidance of lead extraction in defibrillation lead failure? A single-centre experience. Europace 12(4):522–526
Swerdlow CD, Ellenbogen KA (2013) Implantable cardioverter-defibrillator leads: design, diagnostics, and management. Circulation 128(18):2062–2071
Kusumoto FM, Schoenfeld MH, Wilkoff BL, Berul CI, Birgersdotter-Green UM, Carrillo R, Cha YM, Clancy J, Deharo JC, Ellenbogen KA, Exner D, Hussein AA, Kennergren C, Krahn A, Lee R, Love CJ, Madden RA, Mazzetti HA, Moore JC, Parsonnet J, Patton KK, Rozner MA, Selzman KA, Shoda M, Srivathsan K, Strathmore NF, Swerdlow CD, Tompkins C, Wazni O (2017) 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 14(12):e503–e551
Koneru JN, Gunderson BD, Sachanandani H, Wohl BN, Kendall KT, Swerdlow CD, Ellenbogen KA (2013) Diagnosis of high-voltage conductor fractures in Sprint Fidelis leads. Heart Rhythm 10(6):813–818
Hauser RG, McGriff D, Retel LK (2012) Riata implantable cardioverter-defibrillator lead failure: analysis of explanted leads with a unique insulation defect. Heart Rhythm 9(5):742–749
Leong DP, van Erven L (2012) Unrecognized failure of a narrow caliber defibrillation lead: the role of defibrillation threshold testing in identifying an unprotected individual. Pacing Clin Electrophysiol 35(6):e154–e155
Wutzler A, Attanasio P, Haverkamp W, Blaschke F (2016) Near-fatal ICD lead dysfunction with implications for ICD testing. Pacing Clin Electrophysiol 39(1):105–106
Hauser RG, Abdelhadi R, McGriff D, Retel LK (2012) Deaths caused by the failure of Riata and Riata ST implantable cardioverter-defibrillator leads. Heart Rhythm 9(8):1227–1235
Shah P, Singh G, Chandra S, Schuger CD (2013) Failure to deliver therapy by a Riata Lead with internal wire externalization and normal electrical parameters during routine interrogation. J Cardiovasc Electrophysiol 24(1):94–96
Wilkoff BL, Love CJ, Byrd CL, Bongiorni MG, Carrillo RG, Crossley GH 3rd, Epstein LM, Friedman RA, Kennergren CE, Mitkowski P, Schaerf RH, Wazni OM, Heart Rhythm S, American Heart A (2009) Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management: this document was endorsed by the American Heart Association (AHA). Heart Rhythm 6(7):1085–1104
Higgins JV, Gard JJ, Sheldon SH, Espinosa RE, Wood CP, Felmlee JP, Cha YM, Asirvatham SJ, Dalzell C, Acker N, Watson RE Jr., Friedman PA (2014) Safety and outcomes of magnetic resonance imaging in patients with abandoned pacemaker and defibrillator leads. Pacing Clin Electrophysiol 37(10):1284–1290
Austin CO, Landolfo K, Parikh PP, Patel PC, Venkatachalam KL, Kusumoto FM (2017) Retained cardiac implantable electronic device fragments are not associated with magnetic resonance imaging safety issues, morbidity, or mortality after orthotopic heart transplant. Am Heart J 190:46–53
Padmanabhan D, Mehta R, Kapa S, Abhishek D, Mulpuru S, Jaffe AS, Felmlee JP, Jondal ML, Dalzell CM, Asirvatham SJ, Cha YM, Watson RE Jr., Friedman PA (2017) Safety of magnetic resonance imaging in patients with legacy pacemakers and defibrillators and abandoned leads. Heart Rhythm. https://doi.org/10.1016/j.hrthm.2017.10.022
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Lacour, A. Parwani, M. Huemer, P. Attanasio, P.L. Dang, J. Luebcke, L. Schleussner, D. Blaschke, L.-H. Boldt, B. Pieske, W. Haverkamp, and F. Blaschke declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
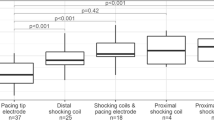
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Lacour, P., Parwani, A., Huemer, M. et al. What physicians do in case of a failure of the pace-sense part of a defibrillation lead. Herz 45, 362–368 (2020). https://doi.org/10.1007/s00059-018-4736-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-018-4736-9
Keywords
- Cardiac implantable electronic device
- High-voltage lead
- Implantable cardioverter-defibrillator
- Medical device failure
- Cardiac resynchronization therapy