Abstract
Background
Distal embolization during primary percutaneous coronary intervention (p-PCI) in the treatment of ST-segment elevation myocardial infarction (STEMI) is associated with a poor prognosis. In this situation, thrombectomy is performed to prevent distal embolization and to restore myocardial reperfusion. The aim of our study was to determine angiographic predictors of angiographically visible distal embolization (AVDE) in patients with STEMI treated by p‑PCI with thrombectomy.
Patients and methods
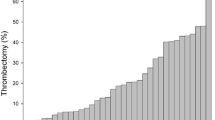
This prospective study included all consecutive patients who underwent p‑PCI with thrombectomy for STEMI at our institution between October 2011 and December 2014 AVDE was defined as a distal filling defect with an abrupt cut-off in one of the peripheral coronary branches of the infarct-related artery, distal to the angioplasty site. Thrombectomy was considered positive when it removed thrombi, and successful when it improved coronary flow.
Results
Among the 346 patients included, 59 (17%) developed AVDE during p‑PCI. In multivariate analysis, the infarct-related right coronary artery (OR: 2.48, 95% CI: 1.36–4.52; p = 0.003) and a culprit lesion diameter of >3 mm (OR : 1.90, 95% CI: 1.01–3.56; p = 0.048) were identified as independent factors associated with AVDE during p‑PCI with thrombectomy for STEMI. The success of thrombectomy and the Syntax score were not associated with AVDE.
Conclusion
AVDE complicating p‑PCI with thrombectomy in STEMI is frequent (17%) and a successful thrombectomy does not rule out AVDE.
Zusammenfassung
Hintergrund
Die distale Embolie während einer primären perkutanen Koronarintervention (p-PCI) zur Therapie des ST-Strecken-Hebungs-Infarkts (STEMI) geht mit einer schlechten Prognose einher. In dieser Situation wird eine Thrombektomie durchgeführt, um einer distalen Embolie vorzubeugen und die Myokardperfusion wiederherzustellen. Ziel der vorliegenden Studie war es, angiographische Prädiktoren einer angiographisch sichtbaren distalen Embolie („angiographically visible distal embolization“, AVDE) bei Patienten mit STEMI und Behandlung durch p‑PCI mit Thrombektomie zu ermitteln.
Patienten und Methoden
In die vorliegende prospektive Studie wurden alle aufeinanderfolgenden Patienten eingeschlossen, bei denen zwischen Oktober 2011 und Dezember 2014 eine p‑PCI mit Thrombektomie zur Therapie eines STEMI an der Klinik der Autoren erfolgte. Eine AVDE wurde als distaler Füllungsdefekt mit abruptem Abbruch in einem der peripheren Äste der infarktbeteiligten Koronararterie definiert, und zwar distal der Stelle der Angioplastie. Eine Thrombektomie galt als positiv, wenn damit Thromben entfernt wurden, und als erfolgreich, wenn sie zu einer Verbesserung des Koronarflusses führte.
Ergebnisse
Von den 346 in die Studie eingeschlossenen Patienten trat bei 59 (17 %) eine AVDE während der p‑PCI auf. In der multivariaten Analyse stellten sich die infarktbeteiligte rechte Koronararterie (Odds Ratio, OR: 2,48; 95 %-Konfidenzintervall, 95 %-KI: 1,36–4,52; p = 0,003) und ein Durchmesser der verursachenden Läsion von >3 mm (OR: 1,90; 95 %-KI: 1,01–3,56; p = 0,048) als unabhängige Faktoren heraus, die mit einer AVDE während der p‑PCI mit Thrombektomie wegen eines STEMI assoziiert waren. Die Erfolgsrate der Thrombektomie und der Syntax-Score waren nicht mit einer AVDE vergesellschaftet.
Schlussfolgerung
Eine AVDE als Komplikation einer p‑PCI mit Thrombektomie bei STEMI ist häufig (17 %), und eine erfolgreiche Thrombektomie schließt eine AVDE nicht aus.
Similar content being viewed by others
Abbreviations
- AVDE:
-
Angiographically visible distal embolization
- IRA:
-
Infarct-related coronary artery
- LDA:
-
Left descending artery
- p-PCI:
-
Primary percutaneous coronary intervention
- RCA:
-
Right coronary artery
- STEMI:
-
ST-segment elevation myocardial infarction
- TIMI:
-
Thrombolysis in Myocardial Infarction
References
Mukherjee D, Moliterno DJ (2000) Achieving tissue-level perfusion in the setting of acute myocardial infarction. Am J Cardiol 85(8):39C–46C
Henriques JP, Zijlstra F, Ottervanger JP, de Boer MJ, van ’t Hof AW, Hoorntje JC, Suryapranata H (2002) Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J 23(14):1112–1117. https://doi.org/10.1053/euhj.2001.3035
Kirtane AJ, Sandhu P, Mehran R, McEntegart M, Cristea E, Brener SJ, Xu K, Fahy M, Genereux P, Wessler JD, Stone GW (2014) Association between intraprocedural thrombotic events and adverse outcomes after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (a Harmonizing Outcomes With RevasculariZatiON and Stents in Acute Myocardial Infarction [HORIZONS-AMI] Substudy). Am J Cardiol 113 (1):36–43. https://doi.org/10.1016/j.amjcard.2013.08.034
Wessler JD, Genereux P, Mehran R, Ayele GM, Brener SJ, McEntegart M, Ben-Yehuda O, Stone GW, Kirtane AJ (2016) Which intraprocedural thrombotic events impact clinical outcomes after percutaneous coronary intervention in acute coronary syndromes?: a pooled analysis of the HORIZONS-AMI and ACUITY trials. JACC Cardiovasc Interv 9(4):331–337. https://doi.org/10.1016/j.jcin.2015.10.049
Takahashi A, Sakamoto S, Taniguchi N (2012) Thrombus aspiration with microcatheter for distal embolization during primary angioplasty for acute myocardial infarction: technical notes. J Invasive Cardiol 24(11):618–621
Weipert KF, Bauer T, Nef HM, Mollmann H, Hochadel M, Marco J, Weidinger F, Zeymer U, Gitt AK, Hamm CW (2015) Use and outcome of thrombus aspiration in patients with primary PCI for acute ST-elevation myocardial infarction: results from the multinational Euro Heart Survey PCI Registry. Heart Vessels. https://doi.org/10.1007/s00380-015-0754-1
Gibson CM, de Lemos JA, Murphy SA, Marble SJ, McCabe CH, Cannon CP, Antman EM, Braunwald E, Group TS (2001) Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy. Circulation 103(21):2550–2554
Guenancia C, Stamboul K, Hachet O, Yameogo V, Garnier F, Gudjoncik A, Cottin Y, Lorgis L (2016) Clinical effectiveness of the systematic use of the GRACE scoring system (in addition to clinical assessment) for ischaemic outcomes and bleeding complications in the management of NSTEMI compared with clinical assessment alone: a prospective study. Heart Vessels 31(6):897–906. https://doi.org/10.1007/s00380-015-0695-8
Napodano M, Peluso D, Marra MP, Frigo AC, Tarantini G, Buja P, Gasparetto V, Fraccaro C, Isabella G, Razzolini R, Iliceto S (2012) Time-dependent detrimental effects of distal embolization on myocardium and microvasculature during primary percutaneous coronary intervention. Jacc Cardiovasc Interv 5(11):1170–1177. https://doi.org/10.1016/j.jcin.2012.06.022
Napodano M, Al Mamary AH, Zilio F, Dariol G, Frigo AC, Tarantini G, Carrer A, Fraccaro C, D’Amico G, Iliceto S (2015) Development and validation of a distal embolization risk score during primary angioplasty in ST-elevation myocardial infarction. Am J Cardiol 116(8):1172–1178. https://doi.org/10.1016/j.amjcard.2015.07.027
Balevski I, Sajko MC, Kanic V, Noc M (2011) Catheter aspiration in ST-elevation myocardial infarction and different extent of coronary thrombus. Am J Cardiol 107(5):681–684. https://doi.org/10.1016/j.amjcard.2010.10.042
Mizote I, Ueda Y, Ohtani T, Shimizu M, Takeda Y, Oka T, Tsujimoto M, Hirayama A, Hori M, Kodama K (2005) Distal protection improved reperfusion and reduced left ventricular dysfunction in patients with acute myocardial infarction who had angioscopically defined ruptured plaque. Circulation 112(7):1001–1007. https://doi.org/10.1161/CIRCULATIONAHA.104.532820
Mehran R, Dangas G, Mintz GS, Lansky AJ, Pichard AD, Satler LF, Kent KM, Stone GW, Leon MB (2000) Atherosclerotic plaque burden and CK-MB enzyme elevation after coronary interventions : intravascular ultrasound study of 2256 patients. Circulation 101(6):604–610
Napodano M, Ramondo A, Tarantini G, Peluso D, Compagno S, Fraccaro C, Frigo AC, Razzolini R, Iliceto S (2009) Predictors and time-related impact of distal embolization during primary angioplasty. Eur Heart J 30(3):305–313. https://doi.org/10.1093/eurheartj/ehn594
De Carlo M, Aquaro GD, Palmieri C, Guerra E, Misuraca L, Giannini C, Lombardi M, Berti S, Petronio AS (2012) A prospective randomized trial of thrombectomy versus no thrombectomy in patients with ST-segment elevation myocardial infarction and thrombus-rich lesions: MUSTELA (MUltidevice Thrombectomy in Acute ST-Segment ELevation Acute Myocardial Infarction) trial. JACC Cardiovasc Interv 5(12):1223–1230. https://doi.org/10.1016/j.jcin.2012.08.013
Messas N, Hess S, El Adraa A, Ristorto J, Goiorani F, Brocchi J, Radulsecu B, Jesel L, Zupan M, Ohlmann P, Morel O (2014) Impact of manual thrombectomy on myocardial reperfusion as assessed by ST-segment resolution in STEMI patients treated by primary PCI. Arch Cardiovasc Dis 107(12):672–680. https://doi.org/10.1016/j.acvd.2014.07.044
Funding
This work was supported by the University Hospital of Dijon, the Faculty of Medicine of Dijon, the Association de Cardiologie de Bourgogne, and by grants from the Union Régionale des Caisses d’Assurance Maladie de Bourgogne (URCAM), the Agence Regionale de Santé (ARS) de Bourgogne, the Conseil Régional de Bourgogne and the Fédération Française de Cardiologie (FFC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V.N. Yaméogo, C. Guenancia, G. Porot, K. Stamboul, C. Richard, A. Gudjoncik, J. Hamblin, P. Buffet, L. Lorgis, and Y. Cottin declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yaméogo, N.V., Guenancia, C., Porot, G. et al. Predictors of angiographically visible distal embolization in STEMI. Herz 45, 288–292 (2020). https://doi.org/10.1007/s00059-018-4723-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-018-4723-1
Keywords
- Acute myocardial infarction
- ST-segment elevation myocardial infarction
- Distal embolization
- Thrombectomy
- Angiography