Abstract
Background
This study aimed to evaluate the effect of different blood pressure (BP) parameters on the collateral circulation in a retrospective cohort of patients with acute ischemic stroke and ipsilateral internal carotid artery (ICA) occlusion.
Methods
The degree of intracranial collaterals was graded according to the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) Collateral Flow Grading System. At 12–72 h after stroke onset, six BP measurements were obtained in 124 patients with ICA occlusion. Baseline clinical and imaging characteristics were collected. Group comparisons were performed, and the collateral score (CS) was assessed and entered into a logistic regression analysis.
Results
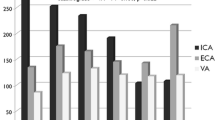
In all, 80 (64.5%) patients displayed good collateral filling (CS ≥ 2). Good intracranial collaterals were more frequently associated with the development of collaterals in the anterior communicating artery, posterior communicating artery, and leptomeningeal artery. The systolic blood pressure (SBP; p = 0.018), diastolic blood pressure (DBP; p = 0.013), and mean arterial pressure (MAP; p = 0.016) were significantly associated with good CS. Median CS was highest when SBP was 120–130 mm Hg (p = 0.034). Logistic regression analysis showed that hypertension (p = 0.026, OR: 0.380, 95% CI: 0.163–0.890) was a significant predictor of poor CS.
Conclusion
The development of collateral circulation in patients with acute ischemic stroke with ICA occlusion may be influenced by BP. A moderately decreased SBP is associated with good integrity of the collateral circulation in patients with acute ischemic stroke with occlusion of the ICA.
Zusammenfassung
Hintergrund
Die vorliegende Studie zielte darauf ab, die Wirkung verschiedener Parameter des Blutdrucks („blood pressure“, BP) auf den Umgehungskreislauf in einer retrospektiven Kohorte von Patienten mit akutem ischämischem Schlaganfall und ipsilateralem Verschluss der A. carotis interna („internal carotid artery“, ICA) zu untersuchen.
Methoden
Das Ausmaß intrakranieller Kollateralen wurde gemäß dem Klassifikationssystem für den Kollateralfluss, dem Collateral Flow Grading System der American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR), eingestuft. Zum Zeitpunkt 12–72 h nach Beginn des Schlaganfalls erfolgten 6 Blutdruckmessungen bei 124 Patienten mit ICA-Verschluss. Die klinischen und bildgebenden Ausgangsmerkmale wurden dokumentiert. Es wurde ein Gruppenvergleich durchgeführt, darüber hinaus wurde der Kollateralscore („collateral score“, CS) ermittelt und in die logistische Regressionsanalyse aufgenommen.
Ergebnisse
Insgesamt zeigte sich bei 80 (64,5%) Patienten eine gute Kollateralenfüllung (CS ≥ 2). Gute intrakranielle Kollateralen waren häufiger mit der Entwicklung von Kollateralen in der A. communicans anterior, der A. communicans posterior und der A. leptomeningealis assoziiert. Der systolische Blutdruck (SBP; p = 0,018), diastolische Blutdruck (DBP; p = 0,013) und der mittlere arterielle Druck („mean arterial pressure“, MAP; p = 0,016) waren signifikant mit einem guten CS korreliert. Der mediane CS war am höchsten, wenn der SBP 120–130 mm Hg (p = 0,034) betrug. Die logistische Regressionsanalyse zeigte, dass Hypertonie (p = 0,026; Odds Ratio, OR: 0,380; 95%-Konfidenzintervall, 95%-KI: 0,163–0,890) ein signifikanter Prädiktor eines schlechten CS war.
Schlussfolgerung
Die Entwicklung eines Umgehungskreislaufs bei Patienten mit akutem ischämischem Schlaganfall mit ICA-Verschluss wird möglicherweise durch den Blutdruck beeinflusst. Ein mäßig erniedrigter SBP ist mit einer guten Ausprägung des Kollateralkreislaufs bei Patienten mit akutem ischämischem Schlaganfall und Verschluss der ICA assoziiert.

Similar content being viewed by others
References
Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, Ovbiagele B et al (2011) Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke 42:693–699
Sung SM, Lee TH, Cho HJ, Kang TH, Jung DS, Park KP et al (2015) Functional outcome after recanalization for acute pure M1 occlusion of the middle cerebral artery as assessed by collateral CTA flow. Clin Neurol Neurosurg 131:72–76
Leng X, Lan L, Liu L, Leung TW, Wong KS (2016) Good collateral circulation predicts favorable outcomes in intravenous thrombolysis:a systematic review and mate-analysis. Eur J Neurol 23(12):1738–1749
Britton M, Carlsson A, de Faire U (1986) Blood pressure course in patients with acute stroke and matched controls. Stroke 17:861–864
Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, Lees KR, Toni D, SITS Investigators (2009) Relationship of blood pressure, antihypertensive therapy, and outcome in ischemic stroke treated with intravenous thrombolysis: retrospective analysis from Safe Implementation of Thrombolysis in Stroke-International Stroke Thrombolysis Register (SITS-ISTR). Stroke 40:2442–2449
Rusanen H, Saarinen JT, Sillanp N (2015) The association of blood pressure and collateral circulation in hyperacute Ischemic stroke patients treated with intravenous thrombolysis. Cerebrovasc Dis 39:130–137
Adams HP Jr, Bendixen BH, Kappelle JJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions of use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Higashida RT, Furlan AJ, Roberts H et al (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34:e109–e137
Calleja AI, Cortijo E, Garcia-Bermejo P, Gomez RD, Perez-Fernandez S, Del Monte JM, Munoz MF, Fernandez-Herranz R, Arenillas JF (2013) Collateral circulation on perfusion-computed tomography-source images predicts the response to stroke intravenous thrombolysis. Eur J Neurol 20:795–802
Lima FO, Furie KL, Silva GS, Lev MH, Camargo EC, Singhal AB, Harris GJ, Halpern EF, Koroshetz WJ, Smith WS, Yoo AJ, Nogueira RG (2010) The pattern of leptomeningeal collaterals on CT angiography is a strong predictor of long-term functional outcome in stroke patients with large vessel intracranial occlusion. Stroke 41:2316–2322
Liebeskind DS, Tomsick TA, Foster LD, Yeatts SD, Carrozzella J, Demchuk AM, Jovin TG, Khatri P, von Kummer R, Sugg RM, Zaidat OO, Hussain SI, Goyal M, Menon BK, Al Ali F, Yan B, Palesch YY, Broderick JP, IMS III Investigators (2014) Collaterals at angiography and outcomes in the Interventional Management of Stroke (IMS) III trial. Stroke 45:759–764
Maas MB, Lev MH, Ay H, Singhal AB, Greer DM, Smith WS, Harris GJ, Halpern E, Kemmling A, Koroshetz WJ, Furie KL (2009) Collateral vessels on CT angiography predict outcome in acute ischemic stroke. Stroke 40:3001–3005
Refiker Ege M, Zorlu A, Birhan Yilmaz M, Acıkgoz S, Tandogan I, Cinar Z (2013) Central diastolic blood pressure is associated with the degree of coronary collateral development. Angiology 64(7):546–552
Heil M, Eitenmüller I, Schmitz-Rixen T, Schaper W (2006) Arteriogenesis versus angiogenesis: similarities and differences. J Cell Mol Med 10(1):45–55
Ko Y, Park JH, Yang MH, Ko SB, Han MK, Oh CW et al (2010) The significance of blood pressure variability for the development of hemorrhagic transformation in acute ischemic stroke. Stroke 41:2512–2518
Mattle HP, Kappeler L, Arnold M, Fischer U, Nedeltchev K, Remonda L et al (2005) Blood pressure and vessel recanalization in the first hours after ischemic stroke. Stroke 36:264–268
Buratti L, Cagnetti C, Balucani C, Viticchi G, Falsetti L, Luzzi S et al (2014) Blood pressure variability and stroke outcome in patients with internal carotid artery occlusion. J Neurol Sci 339(1–2):164–168
Kang J, Ko Y, Park JH, Kim WJ, Jang MS, Yang MH et al (2012) Effect of blood pressure on 3-month functional outcome in the subacute stage of ischemic stroke. Neurology 79:2018–2024
Rothwell PM, Howard SC, Spence JD, Carotid Endarterectomy Trialists’ Collaboration. (2003) Relationship between blood pressure and stroke risk in patients with symptomatic carotid occlusive disease. Stroke 34:2583–2592
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Wufuer, P. Mijiti, R. Abudusalamu, H. Dengfeng, C. Jian, M. Jianhua, and Z. Xiaoning declare that they have no competing interests.
This contribution depicts a retrospective study which does not interfere with therapy. The protocol was approved by the Xinjiang Medical University Ethics Committee and conducted in accordance with the Declaration of Helsinki. All patients gave written informed consent.
Additional information
Author contributions. Conceptualization: Z. Xiaoning; data acquisition: A. Wufuer, P. Mijiti; formal analysis: A. Wufuer, ZJ; methodology: P. Mijiti, C. Jian; resources: A. Wufuer, C. Jian, TS; software: P. Mijiti, M. Jianhua; validation: TS, M. Jianhua; writing of original draft: A. Wufuer, PW, Z. Xiaoning; review and editing: A. Wufuer, Z. Xiaoning; A. Wufuer and P. Mijiti share first authorship.
Rights and permissions
About this article
Cite this article
Wufuer, A., Mijiti, P., Abudusalamu, R. et al. Blood pressure and collateral circulation in acute ischemic stroke. Herz 44, 455–459 (2019). https://doi.org/10.1007/s00059-018-4691-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-018-4691-5
Keywords
- Collateral blood circulation
- Cerebrovascular stroke
- Hypertension
- Cerebral arteries
- Carotid artery, internal