Abstract
Background
Osteopontin (OPN) is an extracellular matrix glycoprotein that plays a role in a variety of cellular activities associated with inflammatory and fibrotic responses. Increased OPN levels in myocardium and plasma have been demonstrated in patients with dilated cardiomyopathy (DCM). However, nothing is known about OPN levels in patients with hypertrophic cardiomyopathy (HCM). Therefore, the aim of our study was to compare plasma OPN levels in patients with these two most common cardiomyopathies.
Patients and methods
We examined plasma OPN as well as creatinine, C‑reactive protein (CRP), brain-type natriuretic peptide (BNP), and troponin I levels in 64 patients with DCM, 43 patients with HCM, and 75 control subjects. Transthoracic echocardiography was also performed on all cardiomyopathy patients.
Results
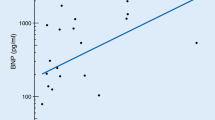
Plasma OPN levels were significantly elevated in patients with DCM compared with HCM patients (95 ± 43 vs. 57 ± 21 ng/ml; p < 0.001) and control subjects (54 ± 19 ng/ml; p < 0.001); however, there was no difference between HCM patients and control subjects. New York Heart Association (NYHA) class III or IV disease was more frequently present in DCM patients than in HCM subjects (44 % vs. 2 %, p < 0.0001). In multivariate analysis, BNP and CRP levels together with NYHA class were found to be significant predictors of plasma OPN levels in DCM patients (p = 0.002, p = 0.029, and p < 0.001 for BNP, CRP, and NYHA, respectively).
Conclusion
Plasma OPN levels were associated with overall heart failure severity rather than with specific cardiomyopathy subtype in patients suffering from DCM or HCM, respectively.
Zusammenfassung
Hintergrund
Osteopontin (OPN) ist ein Glykoprotein der extrazellulären Matrix, das bei verschiedenen zellulären Prozessen im Rahmen entzündlicher und fibrotischer Reaktionen eine Rolle spielt. Erhöhte OPN-Spiegel im Myokard und im Plasma wurden bei Patienten mit dilatativer Kardiomyopathie (DCM) nachgewiesen. Es ist jedoch nichts über die OPN-Spiegel bei Patienten mit hypertrophischer Kardiomyopathie (HCM) bekannt. Daher war es Ziel der vorliegenden Studie, die OPN-Spiegel bei Patienten mit diesen beiden häufigsten Kardiomyopathien zu vergleichen.
Patienten und Methoden
Es wurden die Werte für OPN im Plasma sowie Kreatinin, C‑reaktives Protein (CRP), BNP („brain-type natriuretic peptide“) und Troponin I bei 64 Patienten mit DCM, 43 Patienten mit HCM und 75 Kontrollen ermittelt. Auch wurde bei allen Kardiomyopathiepatienten eine transthorakale Echokardiographie durchgeführt.
Ergebnisse
Die OPN-Werte im Plasma waren bei Patienten mit DCM im Vergleich zu HCM-Patienten (95 ± 43 vs. 57 ± 21 ng/ml; p < 0,001) und Kontrollen (54 ± 19 ng/ml; p < 0,001) signifikant erhöht; jedoch bestand kein Unterschied zwischen HCM-Patienten und Kontrollen. Eine Erkrankung der Klasse III oder IV gemäß New York Heart Association (NYHA) lag häufiger bei Patienten mit DCM als bei Patienten mit HCM vor (44 % vs. 2 %, p < 0,0001). In der multivariaten Analyse erwiesen sich die BNP- und CRP-Werte zusammen mit der NYHA-Klasse als signifikante Prädiktoren der OPN-Werte im Plasma bei DCM-Patienten (p = 0,002 für BNP; p = 0,029 für CRP bzw. p < 0,001 für NYHA).
Schlussfolgerung
Die OPN-Spiegel im Plasma waren bei Patienten mit DCM oder HCM eher mit dem Gesamtschweregrad der Herzinsuffizienz als mit spezifischen Subtypen der Kardiomyopathie assoziiert.



Similar content being viewed by others
References
Gravallese EM (2003) Osteopontin: a bridge between bone and the immune system. J Clin Invest 112:147–149. https://doi.org/10.1161/01.HYP.0000148459.25908.49
Klingel K, Kandolf R (2010) Osteopontin: a biomarker to predict the outcome of inflammatory heart disease. Semin Thromb Hemost 36:195–202. https://doi.org/10.1055/s-0030-1251504
Oldberg A, Franzén A, Heinegård D (1986) Cloning and sequence analysis of rat bone sialoprotein (osteopontin) cDNA reveals an Arg-Gly-Asp cell-binding sequence. Proc Natl Acad Sci USA 83:8819–8823
Graf K, Stawowy P (2004) Osteopontin: a protective mediator of cardiac fibrosis? Hypertension 44:809–810. https://doi.org/10.1161/01.HYP.0000148459.25908.49
Inoue M, Shinohara ML (2011) Intracellular osteopontin (iOPN) and immunity. Immunol Res 49:160–172. https://doi.org/10.1007/s12026-010-8179-5
Mazzali M, Kipari T, Ophascharoensuk V et al (2002) Osteopontin – a molecule for all seasons. QJM 95:3–13
O’Regan AW, Chupp GL, Lowry JA et al (1999) Osteopontin is associated with T cells in sarcoid granulomas and has T cell adhesive and cytokine-like properties in vitro. J Immunol 162:1024–1031
Singh M, Foster CR, Dalal S, Singh K (2009) Osteopontin: role in extracellular matrix deposition and myocardial remodelling post-MI. J Mol Cell Cardiol 48:538–543. https://doi.org/10.1016/j.yjmcc.2009.06.015
Singh M, Foster CR, Dalal S, Singh K (2010) Role of osteopontin in heart failure associated with aging. Heart Fail Rev 15:487–494. https://doi.org/10.1007/s10741-010-9158-6
Singh M, Dalal S, Singh K (2014) Osteopontin: at the cross-roads of myocyte survival and myocardial function. Life Sci 118:1–6. https://doi.org/10.1016/j.lfs.2014.09.014
Singh K, Sirokman G, Communal C et al (1999) Myocardial osteopontin expression coincides with the development of heart failure. Hypertension 33:663–670
Behnes M, Brueckmann M, Lang S et al (2013) Diagnostic and prognostic value of osteopontin in patients with acute congestive heart failure. Eur J Heart Fail 15:1390–1400. https://doi.org/10.1093/eurjhf/hft112
Stawowy P, Blaschke F, Pfautsch P et al (2002) Increased myocardial expression of osteopontin in patients with advanced heart failure. Eur J Heart Fail 4:139–146
Rosenberg M, Zugck C, Nelles M et al (2008) Osteopontin, a new prognostic biomarker in patients with chronic heart failure. Circ Heart Fail 1:43–49. https://doi.org/10.1161/CIRCHEARTFAILURE.107.746172
Satoh M, Nakamura M, Akatsu T et al (2005) Myocardial osteopontin expression is associated with collagen fibrillogenesis in human dilated cardiomyopathy. Eur J Heart Fail 7:755–762. https://doi.org/10.1016/j.ejheart.2004.10.019
Elliott P, Andersson B, Arbustini E et al (2008) Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 29:270–276. https://doi.org/10.1093/eurheartj/ehm342
Elliott PM, Anastasakis A, Borger MA et al (2014) 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy. Eur Heart J 35:2733–2779. https://doi.org/10.1093/eurheartj/ehu284
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16:233–270. https://doi.org/10.1093/ehjci/jev014
Devereux RB, Alonso DR, Lutas EM et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Evaluation of left ventricular diastolic function by echocardiography: EAE/ASE Recommendations. Eur J Echocardiogr 10:165–193. https://doi.org/10.1093/ejechocard/jep007
Rudski LG, Lai WW, Afilalo J et al (2010) Echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography Endorsed by the European Association of Echocardiography and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713. https://doi.org/10.1016/j.echo.2010.05.010
Francia P, Balla C, Ricotta A et al (2011) Plasma osteopontin reveals left ventricular reverse remodelling following cardiac resynchronization therapy in heart failure. Int J Cardiol 153:306–310. https://doi.org/10.1016/j.ijcard.2010.08.048
Tang DW, Lin GS, Huang JL et al (2012) Changes of left ventricular myocardial collagen fibres and osteopontin expression in hypertrophic cardiomyopathy. Fa Yi Xue Za Zhi 28:247–251
Arnlöv J, Evans JC, Benjamin EJ et al (2006) Clinical and echocardiographic correlates of plasma osteopontin in the community: the Framingham Heart Study. Heart 92:1514–1515. https://doi.org/10.1136/hrt.2005.081406
Dick SA, Epelman S (2016) Chronic heart failure and inflammation: what do we really know? Circ Res 119:159–176. https://doi.org/10.1161/CIRCRESAHA.116.308030
Anker SD, von Haehling S (2004) Inflammatory mediators in chronic heart failure: an overview. Heart 90:464–470. https://doi.org/10.1136/hrt.2002.007005
Yndestad A, Damås JK, Oie E et al (2006) Systemic inflammation in heart failure – The whys and wherefores. Heart Fail Rev 11:83–92. https://doi.org/10.1007/s10741-006-9196-2
Anand IS, Latini R, Florea VG et al (2005) C‑reactive protein in heart failure. Prognostic value and the effect of valsartan. Circulation 112:1428–1434. https://doi.org/10.1161/CIRCULATIONAHA.104.508465
Szalay G, Sauter M, Haberland M et al (2009) Osteopontin: a fibrosis-related marker molecule in cardiac remodeling of enterovirus myocarditis in the susceptible host. Circ Res 104:851–859. https://doi.org/10.1161/CIRCRESAHA.109.193805
Renault MA, Robbesyn F, Réant P et al (2010) Osteopontin expression in cardiomyocytes induces dilated cardiomyopathy. Circ Heart Fail 3:431–439. https://doi.org/10.1161/CIRCHEARTFAILURE.109.898114
Shin T, Ahn M, Kim H et al (2006) Increased expression of osteopontin in the heart tissue of Lewis rats with experimental autoimmune myocarditis. J Vet Med Sci 68:379–382
Schoensiegel F, Bekeredjian R, Schrewe A et al (2007) Atrial natriuretic peptide and osteopontin are useful markers of cardiac disorders in mice. Comp Med 57:546–553
Bujak M, Kweon HJ, Chatila K et al (2008) Aging-related defects are associated with adverse cardiac remodeling in a mouse model of reperfused myocardial infarction. J Am Coll Cardiol 51:1384–1392. https://doi.org/10.1016/j.jacc.2008.01.011
Jugdutt BI, Palaniyappan A, Uwiera RR, Idikio H (2009) Role of healing-specific-matricellular proteins and matrix metalloproteinases in age-related enhanced early remodeling after reperfused STEMI in dogs. Mol Cell Biochem 322:25–36. https://doi.org/10.1007/s11010-008-9905-3
Acknowledgements
The authors are thankful to Ms. Hana Řeháková of the Institute of Medical Biochemistry and Laboratory Diagnostics for technical assistance.
Funding
The study was supported by MH CZ DRO 64165 and Progres Q38/LF1 projects.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Podzimkova, T. Palecek, P. Kuchynka, J. Marek, B.A. Danek, M. Jachymova, M. Kalousova, T. Zima, and A. Linhart declare that they have no competing interests.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version). Informed consent was obtained from all patients included in the study.
Rights and permissions
About this article
Cite this article
Podzimkova, J., Palecek, T., Kuchynka, P. et al. Plasma osteopontin levels in patients with dilated and hypertrophic cardiomyopathy. Herz 44, 347–353 (2019). https://doi.org/10.1007/s00059-017-4645-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-017-4645-3