Abstract
Background
Thrombocytopenia is a frequently encountered phenomenon during intra-aortic balloon pumping (IABP), which may limit its prolonged utilization. The aim of the study was to explore the risk factors and clinical implications of IABP-associated thrombocytopenia in patients with acute coronary syndrome (ACS).
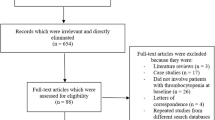
Methods
We retrospectively analyzed the data of 222 patients with ACS undergoing invasive treatment strategy supported by IABP. The incidence and risk factors of IABP-associated thrombocytopenia, and the association between thrombocytopenia and relevant clinical endpoints (in-hospital death, bleeding according to the TIMI scale, and thromboembolic events), were analyzed.
Results
IABP-associated thrombocytopenia was observed in 54.5% (121/222) of the patients. The incidence of thrombocytopenia was higher and the magnitude of reduction in platelet count was greater in the Arrow balloon group (n = 89) compared with the Datascope balloon group (n = 133; 68.5% vs. 45.1%, p = 0.001; 48.7% vs. 33.2%, p < 0.001; respectively). Independent predictors of thrombocytopenia included older age and Arrow balloon utilization (odds ratio [OR]: 1.054; 95% confidence interval [CI]: 1.028–1.080; p<0.001; OR: 2.468; 95%CI: 1.375–4.431; p = 0.002; respectively). The incidence of in-hospital death was higher in patients who developed thrombocytopenia than those who did not (9.1% vs. 2.0%, p = 0.041), and thrombocytopenia was correlated with in-hospital death (OR: 5.932; 95%CI: 1.221–28.822; p = 0.027). However, the rates of TIMI bleeding and thromboembolic events were similar between the two groups (5.8% vs. 5.0%, p = 1.000; 3.2% vs. 6.0%, p = 0.518; respectively), and thrombocytopenia was not associated with TIMI bleeding or thromboembolic events (OR: 0.940; 95%CI: 0.267–3.307; p = 0.923; OR: 0.541, 95%CI: 0.148–1.974, p = 0.352; respectively).
Conclusion
IABP-associated thrombocytopenia occurred in 54.5% of patients with ACS undergoing an invasive strategy and it was correlated with increased in-hospital mortality. Older age and use of the Arrow balloon may predict IABP-associated thrombocytopenia.
Zusammenfassung
Hintergrund
Die Thrombozytopenie gilt als eine häufige Komplikation beim Einsatz der intraaortalen Ballongegenpulsation (IABP), was deren Langzeitanwendung beschränken könnte. Ziel der vorliegenden Studie war es, die Risikofaktoren und klinischen Auswirkungen der IABP-assoziierten Thrombozytopenie bei Patienten mit akutem Koronarsyndrom (ACS) zu untersuchen.
Methode
Retrospektiv wurden die Daten von 222 IABP-Patienten mit ACS und invasiver Behandlungsstrategie ausgewertet. Dabei wurden die Inzidenz und Risikofaktoren der IABP-assoziierten Thrombozytopenie analysiert und der Zusammenhang zwischen Thrombozytopenie und relevanten klinischen Endpunkten (Krankenhausmortalität, TIMI-Blutung laut Kriterien gemäß „thrombolysis in myocardial infarction“ und Thromboembolien) untersucht.
Ergebnisse
Eine IABP-assoziierte Thrombozytopenie trat bei 54,5 % (121/222) der Patienten auf. Im Vergleich zu der Datascope-Ballon-Gruppe (n = 133) wurde eine höhere Inzidenz der Thrombozytopenie und eine größere Reduktion der Thrombozytenzahl in der Arrow-Ballon-Gruppe (n = 89) beobachtet (68,5 % vs. 45,1 %; p = 0,001 bzw. 48,7 % vs. 33,2 %; p < 0,001). Zu den unabhängigen Prädiktoren der Thrombozytopenie zählten höheres Alter und die Anwendung des Arrow-Ballons (Odds Ratio, OR: 1,054; 95%-Konfidenzintervall, 95%-KI: 1,028–1,080; p < 0,001 bzw. OR: 2,468; 95%-KI: 1,375–4,431; p = 0,002). Die Krankenhausmortalität war bei Thrombozytopeniepatienten höher als bei Patienten ohne Thrombozytopenie (9,1 % vs. 2,0 %; p = 0,041), dabei war die Thrombozytopenie mit der Krankenhausmortalität korreliert (OR: 5,932; 95%-KI: 1,221–28,822; p = 0,027). Die Rate an TIMI-Blutungen und Thromboembolien war jedoch zwischen beiden Gruppen vergleichbar (5,8% vs. 5,0%; p = 1,000 bzw. 3,2% vs. 6,0%; p = 0,518), und die Thrombozytopenie war weder mit einer TIMI-Blutung noch mit Thromboembolien assoziiert (OR: 0,940; 95%-KI: 0,267–3,307; p = 0,923 bzw. OR: 0,541, 95%-KI: 0,148–1,974; p = 0,352).
Schlussfolgerung
Eine IABP-assoziierte Thrombozytopenie trat bei 54,5% der ACS-Patienten unter invasiver Behandlungsstrategie auf und war mit einer erhöhten Krankenhausmortalität korreliert. Höheres Alter und die Anwendung des Arrow-Ballons können Prädiktoren einer IABP-assoziierten Thrombozytopenie sein.

Similar content being viewed by others
References
Parissis H, Graham V, Lampridis S, Lau M et al (2016) IABP: history-evolution-pathophysiology-indications: what we need to know. J Cardiothorac Surg 11:122. doi:10.1186/s13019-016-0513-0
Kapelios CJ, Terrovitis JV, Nanas JN (2014) Current and future applications of the intra-aortic balloon pump. Curr Opin Cardiol 29:258–265. doi:10.1097/HCO.0000000000000059
Parissis H, Soo A, Al-Alao B (2011) Intra-aortic balloon pump: literature review of risk factors related to complications of the intraaortic balloon pump. J Cardiothorac Surg 6:147. doi:10.1186/1749-8090-6-147
Vales L, Kanei Y, Ephrem G, Misra D (2011) Intra-aortic balloon pump use and outcomes with current therapies. J Invasive Cardiol 23:116–119
Chesebro JH, Knatterud G, Roberts R, Borer J et al (1987) Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation 76:142–154
Ma YC, Zuo L, Chen JH, Luo Q et al (2006) Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol 17:2937–2944. doi:10.1681/ASN.2006040368
Warkentin TE (2004) Heparin-induced thrombocytopenia: diagnosis and management. Circulation 110:e454–e458. doi:10.1161/01.CIR.0000147537.72829.1B
McCabe JC, Abel RM, Subramanian VA, Guy WA Jr (1978) Complications of intra-aortic balloon insertion and counterpulsation. Circulation 57:769–773
Leinbach RC, Nyilas E, Caulfield JB, Buckley MJ et al (1972) Evaluation of hematologic effects of intra-aortic balloon assistance in man. Trans Am Soc Artif Intern Organs 18:493–500 (S 512)
Vonderheide RH, Thadhani R, Kuter DJ (1998) Association of thrombocytopenia with the use of intra-aortic balloon pumps. Am J Med 105:27–32
Roy SK, Howard EW, Panza JA, Cooper HA (2010) Clinical implications of thrombocytopenia among patients undergoing intra-aortic balloon pump counterpulsation in the coronary care unit. Clin Cardiol 33:30–35. doi:10.1002/clc.20694
Bream-Rouwenhorst HR, Hobbs RA, Horwitz PA (2008) Thrombocytopenia in patients treated with heparin, combination antiplatelet therapy, and intra-aortic balloon pump counterpulsation. J Interv Cardiol 21:350–356. doi:10.1111/j.1540-8183.2008.00363.x
Linkins LA (2015) Heparin induced thrombocytopenia. BMJ 350:g7566
Battistelli S, Genovese A, Gori T (2010) Heparin-induced thrombocytopenia in surgical patients. Am J Surg 199:43–51. doi:10.1016/j.amjsurg.2009.01.029
Merlini PA, Rossi M, Menozzi A, Buratti S et al (2004) Thrombocytopenia caused by abciximab or tirofiban and its association with clinical outcome in patients undergoing coronary stenting. Circulation 109:2203–2206. doi:10.1161/01.CIR.0000127867.41621.85
Trost JC, Hillis LD (2006) Intra-aortic balloon counterpulsation. Am J Cardiol 97:1391–1398. doi:10.1016/j.amjcard.2005.11.070
Lubenow N, Kempf R, Eichner A, Eichler P et al (2002) Heparin-induced thrombocytopenia: temporal pattern of thrombocytopenia in relation to initial use or reexposure to heparin. Chest 122:37–42
Warkentin TE, Kelton JG (2001) Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med 344:1286–1292. doi:10.1056/NEJM200104263441704
Huxtable LM, Tafreshi MJ, Rakkar AN (2006) Frequency and management of thrombocytopenia with the glycoprotein IIb/IIIa receptor antagonists. Am J Cardiol 97:426–429. doi:10.1016/j.amjcard.2005.08.066
Briganti E, Losi P, Raffi A, Scoccianti M et al (2006) Silicone based polyurethane materials: a promising biocompatible elastomeric formulation for cardiovascular applications. J Mater Sci Mater Med 17:259–266. doi:10.1007/s10856-006-7312-4
Hui P, Cook DJ, Lim W, Fraser GA et al (2011) The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest 139:271–278. doi:10.1378/chest.10-2243
Crowther MA, Cook DJ, Meade MO, Griffith LE et al (2005) Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care 20:348–353. doi:10.1016/j.jcrc.2005.09.008
Ben HC, Lauzet JY, Rezaiguia-Delclaux S, Duvoux C et al (2003) Effect of severe thrombocytopenia on patient outcome after liver transplantation. Intensive Care Med 29:756–762. doi:10.1007/s00134-003-1727-x
Hanes SD, Quarles DA, Boucher BA (1997) Incidence and risk factors of thrombocytopenia in critically ill trauma patients. Ann Pharmacother 31:285–289
Baughman RP, Lower EE, Flessa HC, Tollerud DJ (1993) Thrombocytopenia in the intensive care unit. Chest 104:1243–1247
Fountain EM, Arepally GM (2017) Etiology and complications of thrombocytopenia in hospitalized medical patients. J Thromb Thrombolysis 43:429–436. doi:10.1007/s11239-016-1467-8
Erickson YO, Samia NI, Bedell B, Friedman KD et al (2009) Elevated procalcitonin and C‑Reactive protein as potential biomarkers of sepsis in a subpopulation of thrombotic microangiopathy patients. J Clin Apher 24:150–154. doi:10.1002/jca.20205
Gore JM, Spencer FA, Gurfinkel EP et al (2009) Thrombocytopenia in patients with an acute coronary syndrome (from the Global Registry of Acute Coronary Events [GRACE]). Am J Cardiol 103:175–180. doi:10.1016/j.amjcard.2008.08.055
Acknowledgements
This study was supported by the National Natural Science Foundation of China (30872524) and CAMS Innovation Fund for Medical Sciences (CIFMS 2016-I2M-1-009).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Z. Sheng, H. Zhao, H. Yan, S. Jiang, Y. Guan, Y. Zhang, L. Song, C. Liu, P. Zhou, K. Liu, J. Liu, and Y. Tan declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sheng, Z., Zhao, H., Yan, H. et al. Intra-aortic balloon pumping and thrombocytopenia in patients with acute coronary syndrome. Herz 43, 555–564 (2018). https://doi.org/10.1007/s00059-017-4599-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-017-4599-5