Abstract
Background
Heart failure with preserved ejection fraction (HFpEF) is a syndrome in which patients have symptoms and signs of heart failure but preserved ejection fraction. Left atrial (LA) volume and function are known to be impaired in these patients. Two-dimensional speckle-tracking echocardiography (2D-STE) has recently enabled the quantification of LA deformation dynamics. In this study, we evaluated the use of 2D-STE for the diagnosis of HFpEF.
Patients and methods
The study included 83 patients with suspected HFpEF. Patients were divided into two groups after HFpEF had been diagnosed according to current guidelines. Parameters of diastolic dysfunction were evaluated, including left ventricular mass index (LVMI), LA volume index (LAVI), E/A ratio, deceleration time (DT), E/E’, and STE parameters such as global longitudinal LA strain during ventricular systole (GLAs-res) and strain during late diastole (GLAs-pump).
Results
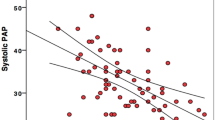
The values of BNP, LVMI, DT, LAVI, and GLAs-res were significantly different between the two groups. In univariate analysis, a strong negative correlation was seen between GLAs-res and BNP (r = −0.567, p < 0.001) as well as between GLAs-res and DT (r = −0.665, p < 0.001), while a moderate negative correlation was found between GLAs-res and LVMI (r = −0.458, p < 0.001) and GLAs-res and LAVI (r = −0.316, p = 0.004). In logistic regression analysis, GLAs-res (p = 0.049, OR = 0.71, 95 % CI = 0.451–0.99), BNP (p = 0.025, OR = 1.08, 95 % CI = 1.01–1.14), and LAVI (p = 0.042, OR = 1.59, 95 % CI = 1.02–2.48) were found to be independent predictors of HFpEF.
Conclusion
LA function as assessed by 2D-STE is impaired in patients with HFpEF. A GLAs-res value of < 17.5 % can be useful for the diagnosis of HFpEF.
Zusammenfassung
Hintergrund
Die Herzinsuffizienz mit erhaltener Ejektionsfraktion (HFpEF) stellt ein Syndrom dar, bei dem die Patienten Symptome einer Herzinsuffizienz aufweisen, aber die Ejektionsfraktion erhalten ist. Volumen und Funktion des linken Vorhofs (LA) sind bekanntermaßen bei diesen Patienten eingeschränkt. Mit der zweidimensionalen Speckle-Tracking-Echokardiographie (2D-STE) wurde vor Kurzem die Quantifizierung der LA-Deformationsdynamik ermöglicht. In der vorliegenden Studie wurde der Einsatz der 2D-STE für die Diagnosestellung einer HFpEF untersucht.
Patienten und Methoden
An der Studie nahmen 83 Patienten mit Verdacht auf HFpEF teil. Dabei wurden die Patienten in 2 Gruppen eingeteilt, nachdem die Diagnose HFpEF gemäß aktuellen Leitlinien gestellt worden war. Es wurden Parameter einer diastolischen Funktionsstörung bestimmt, dazu gehörten linksventrikulärer Massenindex (LVMI), LA-Massenindex (LAVI), E/A-Ratio (Verhältnis der frühen zur späten Mitralklappenflussgeschwindikgeit), Dezelerationszeit (DT), E/E’, und STE-Parameter, wie die globale longitudinale LA-Deformation während der Ventrikelsystole (GLAs-res) und die Deformation während der Spätdiastole (GLAs-pump).
Ergebnisse
Die Werte für BNP („brain natriuretic peptide“), LVMI, DT, LAVI und GLAs-res unterschieden sich signifikant zwischen den beiden Gruppen. In der univariaten Analyse zeigte sich eine starke negative Korrelation zwischen GLAs-res und BNP (r = −0,567; p < 0,001) sowie zwischen GLAs-res und DT (r = −0,665; p < 0,001), während eine nur mäßig ausgeprägte negative Korrelation zwischen GLAs-res und LAVI (r = −0,458; p < 0,001) sowie GLAs-res und LVMI festgestellt wurde (r = −0,316; p = 0,004). In der logistischen Regressionsanalyse stellten sich GLAs-res (p = 0,049; Odds Ratio, OR = 0,71; 95 %-Konfidenzintervall, 95 %-KI = 0,451–0,99), BNP (p = 0,025; OR = 1,08; 95 %-KI = 1,01–1,14) und LAVI (p = 0,042; OR = 1,59; 95 %-KI = 1,02–2,48) als unabhängige Prädiktoren einer HFpEF heraus.
Schlussfolgerung
Die mit der 2D-STE bestimmte LA-Funktion bei Patienten mit HFpEF erwies sich als eingeschränkt. Ein GLAs-res-Wert von < 17,5 % kann für die Diagnose einer HFpEF hilfreich sein.


Similar content being viewed by others
References
Zile MR, Brutsaert DL (2002) New concepts in diastolic dysfunction and HFpEF: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 105:1387
Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351:1097
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J 28:2539
Owan TE, Hodge DO, Herges RM et al (2006) Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355:251–259
Abhayaratna WP, Marwick TH, Smith WT et al (2006) Characteristics of left ventricular diastolic dysfunction in the community: an echocardiographic survey. Heart 92:1259–1264
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J 28(20):2539–2550
Lang RM, Bierig M, Devereux RB et al (2006) American society of echocardiography’s nomenclature and standards committee; task force on chamber quantification; american college of cardiology echocardiography committee; american heart association; european association of echocardiography, european society of cardiology. recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Kircher B, Abbott JA, Pau S et al (1991) Left atrial volume determination by biplane two-dimensional echocardiography: validation by cine computed tomography. Am Heart J 121(3 Pt 1):864–871
Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351(11):1097–1105
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J 28:2539
Topol EJ, Traill TA, Fortuin NJ (1985) Hypertensive hypertrophic cardiomyopathy of the elderly. N Engl J Med 312(5):277–283
Gottdiener JS, McClelland RL, Marshall R et al (2002) Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The cardiovascular health study. Ann Intern Med 137(8):631
Masoudi FA, Havranek EP, Smith G et al (2003) Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol 41:217
Kitzman DW, Gardin JM, Gottdiener JS et al (2001) Importance of heart failure with preserved systolic function in patients > or = 65 years of age. CHS research group. Cardiovascular health study. Am J Cardiol 87:413
Devereux RB, Roman MJ, Liu JE et al (2000) Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the strong heart study. Am J Cardiol 86:1090
Smith GL, Masoudi FA, Vaccarino V et al (2003) Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol 41:1510
Packer M (1990) Abnormalities of diastolic function as potential cause of exercise intolerance in chronic heart failure. Circulation 81(86):III–78
Morris DA, Gailani M, Vaz PA et al (2011) Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr 24(6):651–662
Kurt M, Wang J, Torre-Amione G et al (2009) Left atrial function in diastolic heart failure. Circ Cardiovasc Imaging 2(1):10–15
Santos AB, Kraigher-Krainer E, Gupta DK et al (2014) Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail 16(10):1096–1103
Nascimento CA, Gomes VA, Silva SK et al (2013) Left atrial and left ventricular diastolic function in chagas disease. J Am Soc Echocardiogr 26(12):1424–1433
Sahebjam M, Zoroufian A, Sadeghian H et al (2013) Relationship between left atrial function and size and level of left ventricular dyssynchrony in heart failure patients. Echocardiography 30(7):772–777
Mondillo S, Cameli M, Caputo ML et al (2011) Early detection of left atrial strain abnormalities by speckle tracking inhypertensive and diabetes patients with normal left atrial size. J Am Soc Echocardiogr 24(8):898–908
Guler A, Tigen KM, Dundar C et al (2014) Left atrial deformation and nonischemic dilated cardiomyopathy. A 2D speckle-tracking imaging study. Herz 39(2):251–257
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.M. Aung, A. Güler, Y. Güler, A. Huraibat, C.Y. Karabay, and I. Akdemir state that there are no conflicts of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Aung, S.M., Güler, A., Güler, Y. et al. Left atrial strain in heart failure with preserved ejection fraction. Herz 42, 194–199 (2017). https://doi.org/10.1007/s00059-016-4456-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4456-y