Abstract
Background
In patients recovering from an ST-segment elevation myocardial infarction (STEMI), it is not clear whether the negative impact of stent thrombosis (ST) is different from a non-stent-related recurrent myocardial infarction (NSRMI). This study sought to assess the long-term incidence and prognostic impact of recurrent myocardial infarction (MI) after percutaneous coronary intervention (PCI) for STEMI by comparing outcomes of ST versus NSRMI.
Patients and methods
From 2001 to 2007, 1025 patients undergoing PCI for STEMI were prospectively followed up. Patients with ST, with NSRMI, and those free from recurrent MI were compared regarding mortality and major adverse cardiac and cerebrovascular events (MACCE).
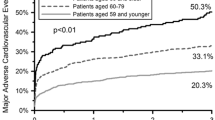
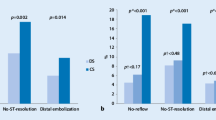
Results
Recurrent MI decreased from 37 events per 1000 person/months in the first month to 3.3 events per 1000 person/months after the first year. The cumulative 5‑year incidence of ST and NSRMI was 5.27 % and 13.2 %, respectively. MACCE at 60 months after recurrence were not significantly different for patients with reinfarction but were significantly higher than for patients free from any recurrent MI (both log-rank p < 0.001). However, the cumulative all-cause death rate did not differ between the three groups (27.8 vs. 26.7 vs. 23.0 %). Compared with ST occurring in the first 30 days after PCI for STEMI, early NSRMI was associated with a significantly reduced risk for all-cause death (HR, 0.21; 95 % CI, 0.33–3.30) but this association did not persist for recurrent MIs occurring in the late (HR, 1.05; 95 % CI, 0.33–3.30) or very late follow-up periods.
Conclusion
Although ST was associated with a significant increase in adverse events in the early recovery period, in the long term, MACCE and all-cause mortality rates were comparable to those for NSRMI.
Zusammenfassung
Hintergrund
Bei Patienten, die sich von einem ST-Streckenerhebungsinfarkt (STEMI) erholen, ist es nicht klar, ob sich die negativen Auswirkungen der Stentthrombose (ST) von einem nicht stentbedingten rekurrierenden Myokardinfarkt (NSRMI) unterscheiden. Diese Studie untersuchte die Langzeitinzidenz und die prognostischen Auswirkungen eines rekurrierenden Myokardinfarkts (MI) nach perkutaner koronarer Intervention (PCI) wegen STEMI, indem die ST- mit den NSRMI-Outcomes verglichen wurden.
Patienten und Methoden
Von 2001 bis 2007 wurden 1025 Patienten, die sich einer PCI wegen STEMI unterzogen, prospektiv untersucht. Patienten mit ST oder NSRMI sowie Patienten ohne rekurrierenden MI wurden bezüglich Mortalität und schweren unerwünschten kardialen Ereignissen („major adverse cardiac and cerebrovascular events“, MACCE) verglichen.
Ergebnisse
Rekurrierende MI verringerten sich nach einem Jahr von 37 Ereignissen pro 1000 Personen/Monat im ersten Monat auf 3,3 Ereignisse pro 1000 Personen/Monat. Die kumulative 5‑Jahres-Inzidenz von ST und NSRMI lag bei 5,27 % bzw. 13,2 %. Die MACE unterschieden sich 60 Monate nach dem Wiederauftreten nicht signifikant von Patienten mit einem Reinfarkt, sie waren jedoch signifikant höher als bei Patienten ohne rekurrierenden MI (beide Log-Rank p < 0,001). Jedoch gab es bei der kumulativen Gesamtmortalitätsrate keinen Unterschied zwischen den drei Gruppen (27,8 vs. 26,7 vs. 23,0 %). Verglichen mit einer ST, die in den ersten 30 Tagen nach PCI wegen STEMI auftrat, waren NSRMI mit einem signifikant geringeren Risiko für die Gesamtmortalität assoziiert (HR 0,21; 95 % KI 0,33–3,30). Diese Assoziation hielt allerdings bei rekurrierenden MIs im späteren (HR 1,05; 95 % KI 0,33–3,30) oder sehr späten Follow-up-Zeitraum nicht an.
Schlussfolgerung
Obwohl ST in der frühen Erholungsphase mit einem signifikanten Anstieg unerwünschter Ereignisse assoziiert waren, waren die Langzeit-MACE und Gesamtmortalitätsraten mit denen für NSRMI vergleichbar.



Similar content being viewed by others
References
Buch P, Rasmussen S, Gislason GH et al (2007) Temporal decline in the prognostic impact of a recurrent acute myocardial infarction 1985 to 2002. Heart 93:210–215
Fox KA, Steg PG, Eagle KA et al (2007) Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA 297:1892–1900
Steg PG, James SK, Atar D et al (2012) ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force on the management of ST-segment elevation acute myocardial infarction of the european society of cardiology (ESC). Eur Heart J 33:2569–2619
De Luca G, Suryapranata H, Stone GW et al (2008) Coronary stenting versus balloon angioplasty for acute myocardial infarction: a meta-regression analysis of randomized trials. Int J Cardiol 126:37–44
Kikkert W, Hoebers L, Damman P et al (2014) Recurrent myocardial infarction after primary Percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol 113:229–235
Miyamoto T, Ishikawa T, Nakano Y, Mutoh M (2016) Very long-term clinical and angiographic outcomes after sirolimus- and paclitaxel-eluting stent placement for ST-elevation myocardial infarction: a propensity score-matched comparison. Cardiovasc Interv Ther. doi:10.1007/s12928-016-0390-4
Aoki J, Lansky AJ, Mehran R, Moses J, Bertrand ME, McLaurin BT (2009) Early stent thrombosis in patients with acute coronary syndromes treated with drug-eluting and bare metal stents: The acute Catheterization and urgent intervention triage strategy trial. Circulation 119:687–698
Chechi T, Vecchio S, Vittori G et al (2008) ST-segment elevation myocardial infarction due to early and late Stent thrombosis A new group of high-risk patients. JACC 51:2396–2402
Kubo S, Kadota K, Ichinohe T et al (2013) Comparison of long-term outcome after Percutaneous coronary intervention for Stent thrombosis between early, late, and very late Stent thrombosis. Circ J 78:101–109
Kimura T, Morimoto T, Kozuma K, Honda Y, Kume T, Aizawa T (2010) Comparisons of baseline demographics, clinical presentation, and long-term outcome among patients with early, late, and very late stent thrombosis of sirolimus-eluting stents: Observations from the Registry of Stent Thrombosis for Review and Reevaluation (RESTART). Circulation 122:52–61
Hochman JS, Sleeper LA, Godfrey E, McKinlay SM, Sanborn T, Col J, LeJemtel T (1999) Should we emergently revascularize occluded coronaries for cardiogenic shocK: an international randomized trial of emergency PTCA/CABG-trial design. the SHOCK trial study group. Am Heart J 137:313–321
Thygesen K, Alpert JS, Jaffe AS et al (2012) Third universal definition of myocardial infarction. Eur Heart J 33:2551–2567
Cutlip DE, Windecker S, Mehran R et al (2007) Clinical endpoints in coronary stent trials: a case for standardized definitions. Circulation 115:2344–2351
Yan BP, Duffy SJ, Clark DJ et al (2008) Rates of Stent thrombosis in bare-metal versus drug-Eluting Stents (from a large australian Multicenter registry). Am J Cardiol 101:1716–1722
Thune JJ, Signorovitch JE, Kober L et al (2011) Predictors and prognostic impact of recurrent myocardial infarction in patients with left ventricular dysfunction, heart failure, or both following a first myocardial infarction. Eur J Heart Fail 13:148–153
De la Torre-Hernandez JM, Alfonso F, Hernandez F, Elizaga J, Sanmartin M, Pinar E (2008) Drug-eluting stent thrombosis: Results from the multicenter Spanish registry ESTROFA (Estudio ESpanol sobre TROmbosis de stents FArmacoactivos). J Am Coll Cardiol 51:986–990
Wenaweser P, Daemen J, Zwahlen M, Van Domburg R, Juni P, Vaina S (2008) Incidence and correlates of drug-eluting stent thrombosis in routine clinical practice. 4‑year results from a large 2‑institutional cohort study. J Am Coll Cardiol 52:1134–1140
Kubo S, Kadota K, Ozaki M, Ichinohe T, Eguchi H, Miyake K (2013) Difference in clinical and angiographic characteristics of very late stent thrombosis between drug-eluting and bare-metal stent implantations. Circ J 77:1453–1460
Stone GW, Witzenbichler B, Guagliumi G et al (2011) Heparin plus a glycoprotein IIb/IIIa inhibitor versus bivalirudin monotherapy and paclitaxel-eluting stents versus bare-metal stents in acute myocardial infarction (HORIZONS-AMI): final 3‑year results from a multicentre, randomised controlled trial. Lancet 377:2193–2204
Vink MA, Dirksen MT, Suttorp MJ et al (2011) A follow-up study of the PASSION (Paclitaxel-Eluting versus conventional Stent in myocardial infarction with ST-segment elevation) trial. J Am Coll Cardiol Intv 4:24–29
Spaulding C, Teiger E, Commeau P et al (2011) Four-year follow-up of TYPHOON (trial to assess the use of the CYPher Sirolimus-Eluting coronary Stent in acute myocardial infarction treated with ballOON Angioplasty). J Am Coll Cardiol Intv 4:14–23
Boden H, Van der Hoeven BL, Liem S et al (2012) Five-year clinical follow-up from the MISSION! Intervention Study: sirolimus-eluting stent versus bare metal stent implantation in patients with ST-segment elevation myocardial infarction, a randomised controlled trial. EuroIntervention 7:1021–1029
Valgimigli M, Campo G, Gambetti S et al (2013) Three-year follow-up of the MULTIcentre evaluation of single high-dose bolus tiRofiban versus Abciximab with Sirolimus-eluting STEnt or bare-metal Stent in acute myocardial infarction studY (MULTISTRATEGY). Int J Cardiol 165:134–141
Holmvang L, Kelbæk H, Kaltoft A et al (2013) Long-term outcome after drug-eluting versus bare-metal stent implantation in patients with ST segment elevationmyocardial infarction: 5 years follow-up from the randomized DEDICATION trial (Drug Elution and Distal Protection in Acute Myocardial Infarction). JACC Cardiovasc Interv 6:548–553
Park KW, Kang SH, Chung WY et al (2010) “Real world” comparison of drug-eluting stents vs bare metal stents in the treatment of unselected patients with acute ST-segment elevation myocardial infarction. Circ J 74:1111–1120
Brodie B, Pokharel Y, Fleishman N et al (2011) Very late Stent thrombosis after primary Percutaneous coronary intervention with bare-metal and drug-Eluting Stents for ST-segment elevation myocardial infarction A 15-year single-center experience. J Am Coll Cardiol Intv 4:30–38
Sattur S, Orshaw P, Boura J, Harjai KJ (2012) Long-term safety and effectiveness of drug-eluting stents compared to bare metal stents in ST elevationmyocardial infarction: findings from the Guthrie Health Off-label Stent (GHOST) Registry. J Interv Cardiol 25:118–125
Simsek C, Magro M, Boersma E et al (2011) Comparison of six-year clinical outcome of Sirolimus- and Paclitaxel-Eluting Stents to bare-metal Stents in patients with ST-segment elevation myocardial infarction: an analysis of the RESEARCH and T‑SEARCH registries. J Invasive Cardiol 23:336–341
Polonski L, Gasior M, Gierlotka M et al (2011) A comparison of ST elevation versus non-ST elevation myocardial infarction outcomes in a large registry database: are non-ST myocardial infarctions associated with worse long-term prognoses? Int J Cardiol 152:70–77
Velders MA, Boden H, Hoeven B et al (2013) Long-term outcome of second-generation everolimus-eluting stents and Endeavor zotarolimus-eluting stents in a prospective registry of ST-elevation myocardial infarction patients. EuroIntervention 8:1199–1206
Pedersen F, Butrymovich V, Kelbæk H (2014) Short- and long-term cause of death in patients treated with primary PCI for STEMI. J Am Coll Cardiol 64:2101–2108
Mega J, Braunwald E, Murphy SA et al (2013) Rivaroxaban in patients stabilized after a ST-segment elevation myocardial infarction: results from the ATLAS ACS-2-TIMI-51 trial (anti-Xa therapy to lower cardiovascular events in addition to standard therapy in subjects with acute coronary syndrome-Thrombolysis in myocardial infarction-51). J Am Coll Cardiol 61:1853–1859
Nidorf MS, Eikelboom J, Budgeon C, Thompson PL (2013) Low-dose Colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol 61:404–410
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Viveiros Monteiro, R. Ramos, A. Fiarresga, L. de Sousa, D. Cacela, L. Patricio, L. Bernardes, C. Soares, and R. Cruz Rerreira state that there are no conflicts of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
A. Viveiros Monteiro and R. Ramos contributed equally to this work.
Rights and permissions
About this article
Cite this article
Viveiros Monteiro, A., Ramos, R., Fiarresga, A. et al. Timing and long-term prognosis of recurrent MI after primary angioplasty. Herz 42, 186–193 (2017). https://doi.org/10.1007/s00059-016-4446-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4446-0