Abstract
Aim and background
Galectin-3 (Gal-3) is used to determine the prognosis of heart failure. Some studies revealed that Gal-3 promoted cardiac hypertrophy but there is no study in which the relationship between Gal-3 and left ventricular hypertrophy (LVH) geometry in patients without diastolic and systolic function impairment has been explored. The aim of the study was to analyze associations between plasma Gal-3 levels, LVH, and LV geometry in maintenance hemodialysis (HD) patients without systolic and diastolic dysfunction.
Patients and methods
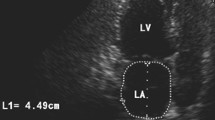
The study group included 105 patients (53 women and 52 men)—with an average age of 58.2 ± 12.6 years, treated with HD for an average of 45 ± 32 months—and 60 healthy controls. The Gal-3 and other biochemical parameters were measured and color Doppler echocardiography was performed. For this study LVH was considered present when the LV mass index (LVMI) exceeded 95 g/m2 in women and 115 g/m2 in men. Left ventricular geometry was classified into the four groups on the basis of left ventricular mass and relative wall thickness (RWT).
Results
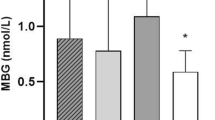
Concentric hypertrophy (CH, 40.9 %, n = 43) was the commonest geometric pattern in our study. The Gal-3 levels in CH patients were not different from the patients with eccentric hypertrophy (EH). Plasma levels of Gal-3 correlated with LVMI (r = 0.617, p < 0.001), parathyroid hormone (PTH, r = 0.408, p < 0.001), uric acid (r = 0.281, p = 0.004), C-reactive protein (CRP, r = 0.412, p < 0.001), and RWT (r = 0.281, p = 0.004) but were inversely correlated with albumin (r = − 0.466, P < 0.001) in the whole group. Plasma levels of Gal-3 were associated with LVMI (r = 0.812, P < 0.001), RWT (r = 0.318, p = 0.001), and CRP(r = 0.381, p < 0.001) in maintenance hemodialysis patients.
Conclusion
The Gal-3 level is related to left ventricular hypertrophy and it is independent of left ventricle geometry. The relationship between LVH and Gal-3 might be direct or it may also be inflammation-related.
Zusammenfassung
Ziel und Hintergrund
Galectin-3 (Gal-3) wird zur Ermittlung der Prognose bei Herzinsuffizienz eingesetzt. Einige Studien haben gezeigt, dass Gal-3 eine kardiale Hypertrophie begünstigt, aber es gibt bisher keine Studie, in der die Beziehung zwischen Gal-3 und geometrischen Parametern einer linksventrikulären Hypertrophie (LVH) bei Patienten ohne diastolische und systolische Funktionseinschränkung untersucht wurde. Ziel dieser Studie war es, Zusammenhänge zwischen dem Gal-3-Spiegel im Plasma, LVH und LV-Geometrie bei Patienten mit Erhaltungsdialyse (Hämodialyse, HD) ohne systolische und diastolische Funktionsstörung zu untersuchen.
Methoden
Die Gruppe der Studienteilnehmer umfasste 105 Patienten (53 w, 52 m) mit einem Durchschnittsalter von 58,2 ± 12,6 Jahren, die durchschnittlich seit 45 ± 32 Monaten unter HD-Behandlung standen, und 60 gesunde Kontrollen. Es wurden Gal-3 und einige Laborparameter bestimmt sowie eine Farbdopplerechokardiographie durchgeführt. Für diese Studie wurde vom Vorliegen einer LVH ausgegangen, wenn der LV-Massenindex (LVMI) 95 g/m2 bei Frauen und 115 g/m2 bei Männern überstieg. Die LV-Geometrie wurde in 4 Gruppen eingeteilt, je nach LV-Masse und relativer Wanddicke (RWT, „relative wall thickness“).
Ergebnisse
Die konzentrische Hypertrophie (CH, 40,9 %, n = 43) war das häufigste geometrische Muster in der vorliegenden Studie. Der Gal-3-Spiegel bei CH-Patienten unterschied sich nicht von dem der Patienten mit ekzentrischer Hypertrophie (EH). Die Plasmaspiegel von Gal-3 waren mit dem LVMI (r = 0,617; p < 0,001), Parathormon (PTH, r = 0,408; p < 0,001), Harnsäure (r = 0,281; p= 0,004), C-reaktivem Protein (CRP, r = 0,412; p < 0,001) und der RWT (r = 0,281; p= 0,004) korreliert, aber es bestand eine inverse Korrelation mit Albumin (r = − 0,466; p < 0,001) in der ganzen Gruppe. Bei Patienten mit Erhaltungsdialyse standen die Plasmaspiegel von Gal-3 mit dem LVMI (r = 0,812; p < 0,001), der RWT (r = 0,318; p= 0,001) und CRP (r = 0,381; p < 0,001) in Zusammenhang.
Schlussfolgerung
Den Ergebnissen zufolge steht Gal-3 in einem Zusammenhang mit einer LV-Hypertrophie, ist aber unabhängig von der LV-Geometrie. Es könnte eine unmittelbare oder auch eine entzündungsbedingte Beziehung zwischen LVH und Gal-3 bestehen.




Similar content being viewed by others
References
Nardi E, Palermo A, Mulè G et al (2009) Left ventricular hypertrophy and geometry in hypertensive patients with chronic kidney disease. J Hypertens 27:633–641
Nardi E, Cottone S, Mulè G et al (2007) Influence of chronic renal insufficiency on left ventricular diastolic function in hypertensives without left ventricular hypertrophy. J Nephrol 20:320–328
McMurray JJ, Adamopoulos S, Anker SD et al (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 14:803–869
McGill RL, Biederman RW, Getts RT et al (2009) Cardiac magnetic resonance imaging in haemodialysis patients. J Nephrol 22:367–372
Foley RN, Parfrey PS, Harnett JD et al (1995) Clinical and echocardiographic disease in patients starting end stage renal disease therapy. Kidney Int 47:186–192
Levin A, Thompson C, Ethier J et al (1999) Left ventricular mass index increase in early renal disease: impact in decline in haemoglobin. Am J Kidney Dis 34:125–134
Zoccali C, Benedetto FA, Mallamaci F et al (2004) Left ventricular mass monitoring in the follow-up of dialysis patients: prognostic value of left ventricular hypertrophy progression. Kidney Int 65:1492–1498
London GM, Pannier B, Guerin AP et al (2001) Alterations of left ventricular hypertrophy in and survival of patients receiving haemodialysis: follow-up of an interventional study. J Am Soc Nephrol 12:2759–2767
Muiesan ML, Salvetti M, Monteduro C et al (2004) Left ventricular concentric geometry during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension 43:731–738
Mancia G, De Backer G, Dominiczak A et al (2007) 2007 ESC and ESH Guidelines for the management of arterial hypertension. Eur Heart J 28:1462–1536
Mimura I, Nishi H, Mise N et al (2010) Left ventricular geometry and cardiovascular mortality based on haemodialysis patient autopsy analyses. Nephrology (Carlton) 15:549–554
Radosavljevic G, Volarevic V, Jovanovic I et al (2012) The roles of galectin-3 in autoimmunity and tumor progression. Immunol Res 52:100–110
Gruson D, Ko G (2012) Galectins testing: new promises for the diagnosis and risk stratification of chronic diseases? Clin Biochem 45:719–726
Newlaczyl AU, Yu LG (2011) Galectin-3–a jack-of-all-trades in cancer. Cancer Lett 313:123–128
Boer RA de, Voors AA, Muntendam P et al (2009) Galectin-3: a novel mediator of heart failure development and progression. Eur J Heart Fail 11:811–817
Sherwi N, Merali S, Wong K (2012) Personalizing biomarker strategies in heart failure with galectin-3. Future Cardiol 8:885–894
Sharma UC, Pokharel S, Brakel TJ van et al (2004) Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 110:3121–3128
Liu YH, D’Ambrosio M, Liao TD et al (2009) N-acetyl-seryl-aspartyl-lysyl-proline prevents cardiac remodeling and dysfunction induced by galectin-3, a mammalian adhesion/growth-regulatory lectin. Am J Physiol Heart Circ Physiol 296:H404–H412
Verma A, Meris A, Skali H et al (2008) Prognostic implications of left ventricular mass and geometry following myocardial infarction: the VALIANT (VALsartan In Acute myocardial iNfarcTion Echocardiographic Study. JACC Cardiovasc Imaging 1:582–591
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations of chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Devereux RB, Alonso D, Lutas EM et al (1986) Echocardiographic assessment of left ventricular hypertrophy, comparison to necropsy findings. Am J Cardiol 57:450–455
Appleton CP, Jensen JL, Hatle LK, Oh JK (1997) Doppler evaluation of left and right ventricular diastolic function: a technical guide for obtaining optimal flow velocity recordings. J Am Soc Echocardiogr 10:271–292
Ommen SR, Nishimura RA, Appleton CP et al (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Carabello BA, Paulus WJ (2009) Aortic stenosis. Lancet 373:956–966
Frohlich ED, González A, Díez J (2011) Hypertensive left ventricular hypertrophy risk: beyond adaptive cardiomyocytic hypertrophy. J Hypertens 29:17–26
Yu L, Ruifrok WP, Meissner M et al (2013) Genetic and pharmacological inhibition of galectin-3 prevents cardiac remodeling by interfering with myocardial fibrogenesis. Circ Heart Fail 6:107–117
Nakahara T, Takata Y, Hirayama Y et al (2007) Left ventricular hypertrophy and geometry in untreated essential hypertension is associated with blood levels of aldosterone and procollagen type III amino-terminal peptide. Circ J 71:716–721
Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA (2006) Controversies in ventricular remodelling. Lancet 367:356–367
Gross ML, Ritz E (2008) Hypertrophy and fibrosis in the cardiomyopathy of uremia—beyond coronary heart disease. Semin Dial 21:308–318
Jofré R, Rodriguez-Benitez P, López-Gómez JM et al (2006) Inflammatory syndrome in patients on haemodialysis. J Am Soc Nephrol 17(12 Suppl 3):S274–S280
Henderson NC, Sethi T (2009) The regulation of inflammation by galectin-3. Immunol Rev 230:160–171
Xu Y, Chen Y, Li D et al (2013) Hypertension, fluid overload and micro inflammation are associated with left ventricular hypertrophy in maintenance haemodialysis patients. Ren Fail 35:1204–1209
Moriguchi Y, Yogo K, Aizawa K et al (2011) Left ventricular hypertrophy is associated with inflammation in sodium loaded subtotal nephrectomized rats. Biomed Res 32:83–90
Glassock RJ, Pecoits-Filho R, Barberato SH (2009) Left ventricular mass in chronic kidney disease and ESRD. Clin J Am Soc Nephrol 4(Suppl 1):S79–S91
Compliance with ethical guidelines
Conflict of interest. H. Yilmaz, O. M. Gurel, H.T. Celik, A. Bozkurt, M.E. Yildirim, I. Bilgic, M.A. Bilgic, N. Bavbek, and A. Akcay state that they have no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yilmaz, H., Gurel, O., Celik, H. et al. Relationship of galectin-3 to left ventricular geometry and hypertrophy in chronic hemodialysis patients. Herz 40, 702–708 (2015). https://doi.org/10.1007/s00059-014-4111-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-014-4111-4