Abstract
Aim
The purpose of this study was to assess the associations of polymorphisms in two metalloproteinase genes—metalloproteinase-2 (MMP-2) and angiotensin converting enzyme (ACE)—with clinical response to autologous transplantation of mononuclear bone marrow cells (MBMC) in patients with acute myocardial infarction.
Methods
The double centre study included 48 patients with a first acute myocardial infarction treated with primary coronary angioplasty, stent implantation and transplantation of MBMC. According to the changes in perfusion defect size, left ventricle ejection fraction, end-systolic volume and peak systolic velocity of the infracted wall (dSaMI) after cell therapy, the patients were retrospectively divided into group A (responders) and group B (non-responders). Genomic DNA was isolated from peripheral leukocytes by a standard technique using proteinase K. Three MMP-2 promoter (-1575G/A, -1306C/T and -790T/G) as well as I/D ACE gene polymorphisms were detected by PCR methods with restriction analyses (when necessary) according to standard protocols.
Results
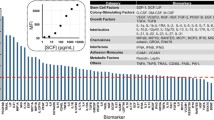
Of the 48 patients who received MBMC transplantation, 17 responded to the therapy. There were no significant differences in the prevalence of matrix metalloproteinase-2 triple genotype GGCCTT between responder/non-responder groups (71% versus 61%, p=0.375). Similarly, no differences in either genotype distribution or allelic frequencies of I/D ACE polymorphism between responders and non-responders to the cell therapy were observed (p=0.933). Compared to patients with ACE genotype ID or DD, the patients with ACE II genotype significantly improved in regional systolic LV function of the infarcted wall after implantations of MBMC (dSaMI – 0.4 versus 1.4 cm/s, p=0.037).
Conclusion
In our study, the ACE genotype II was associated with improvement of regional systolic LV function of the infarcted wall after implantations of MBMC. The detected polymorphism in matrix metalloproteinase-2 gene was not associated with clinical response to cell therapy.
Zusammenfassung
Fragestellung
Ziel der Studie war, die Verbindung zwischen zwei Zink-Metalloproteinase-Genen − Matrix-Metalloproteinase-2 (MMP-2) und Angiotensin-converting-Enzym (ACE) − und deren klinische Reaktion auf autologe Transplantation von mononukleären Knochenmarkzellen (MBMC) bei Patienten mit einem akuten Myokardinfarkt zu untersuchen.
Patienten und Methodik
In die an zwei Zentren durchgeführte Studie waren 48 Patienten eingeschlossen, die wegen eines erstmaligen Myokardinfarkts mit primärer Koronarangioplastie, Stentimplantation und MBMC-Transplantation behandelt wurden. In Abhängigkeit von der Größenänderung des Perfusionsdefekts, der linksventrikulären Ejektionsfraktion (LVEF), des endsystolischen Volumens und der systolischen Maximalgeschwindigkeit der infarzierten Wand (dSaMI) nach der Stammzelltherapie wurden die Patienten retrospektiv in Gruppe A (Responder) und Gruppe B (Nonresponder) eingeteilt. Die Genom-DNA wurde aus peripheren Leukozyten mittels standardisierter Techniken unter Verwendung von Proteinase K isoliert. Sowohl drei MMP-2-Promotoren (-1575G/A, -1306C/T und -790T/G) als auch I/D-ACE-Polymorphismen wurden mittels Polymerase-Kettenreaktion (PCR) und mit Restriktionsanalysen unter Beachtung von Standardprotokollen nachgewiesen.
Ergebnisse
Von 48 Patienten, die eine MBMC-Transplantation erhielten, waren 17 Therapieresponder. Bezüglich der Prävalenz der MMP-2-Triple-Genotypen GGCCTT konnte zwischen Respondern und Nonrespondern (71% vs. 61%; p=0,375) kein signifikanter Unterschied nachgewiesen werden. In ähnlicher Weise wurden weder Unterschiede in der Genotypverteilung noch bei den Allelfrequenzen der I/D-ACE-Polymorphismen zwischen Respondern und Nonrespondern bezüglich der Zelltherapie beobachtet (p=0,933). Im Vergleich zu Patienten mit ACE-Genotyp ID oder DD zeigten die Patienten mit dem ACE-Genotyp II eine signifikante Verbesserung in Bezug auf die regionale systolische linksventrikuläre Funktion der infarzierten Herzmuskelwand nach Implantation von MBMC (dSaMI – 0,4 vs. 1,4 cm/s; p=0,037).
Schlussfolgerung
Im Rahmen dieser Studie konnte für den ACE-Genotyp II eine Verbesserung der regionalen systolischen linksventrikulären Funktion der infarzierten Muskelwand nach MBMC-Implantation nachgewiesen werden. Der detektierte Polymorphismus der MMP-2-Gene war nicht mit einer klinischen Antwort auf die Zelltherapie assoziiert.
Similar content being viewed by others
References
Bartunek J, Vanderheyden M, Vandekerckhove B et al (2005) Intracoronary injection of CD133-positive enriched bone marrow progenitor cells promotes cardiac recovery after recent myocardial infarction: Feasibility and safety. Circulation 112(Suppl):I-178–I-183
Fernández-Avilés F, San Román JA, García-Frade J et al (2004) Experimental and clinical regenerative capability of human bone marrow cell after myocardial infarction. Circ Res 95:742–748
Fuchs S, Satler LF, Kornowski R et al (2003) Catheter-based autologous bone marrow myocardial injection in no-option patients with advanced coronary artery disease. A feasibility study. J Am Coll Cardiol 41(10):1721–1724
Galiñanes M, Loubani M, Davies J et al (2004) Autotransplantation of unmanipulated bone marrow into scarred myocardium is safe and enhances cardiac function in humans. Cell Transplant 13:7–13
Hamano K, Nishida M, Hirata K et al (2001) Local implantation of autologous bone marrow cells for therapeutic angiogenesis in patients with ischemic heart disease. Clinical trial and preliminary results. Jpn Circ J 65:845–847
Chen SL, Fang WW, Ye F et al (2004) Effect on left ventricular function of intracoronary transplantation of autologous bone marrow mesenchymal stem cell in patients with acute myocardial infarction. Am J Cardiol 94:82–95
Stamm C, Westphal B, Kleine HD et al (2003) Autologous bone-marrow stem-cell transplantation for myocardial regeneration. Lancet 361:45–46
Tse HF, Kwong YL, Chan JKF et al (2003) Angiogenesis in ischaemic myocardium by intramyocardial autologous bone marrow mononuclear cell implantation. Lancet 361:47–49
Lunde K, Solheim S, Aakhus S et al (2006) Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. N Engl J Med 355:1199–1209
Meluzin J, Mayer J, Groch L et al (2006) Autologous transplantation of mononuclear bone marrow cells in patients with acute myocardial infarction: The effect of the dose of transplanted cells on myocardial function. Am Heart J 152, 975.e9–975.e15
Kaminek M, Meluzin J, Panovsky R et al (2008) Individual differences in the effectiveness of intracoronary bone marrow cell transplantation assessed by gated sestamibi SPECT/FDG PET imaging. J Nucl Cardiol 15(3):392–399
Agostoni P, Banfi C (2007) Matrix metalloproteinase and heart failure: is it time to move from research to clinical laboratories? Eur Heart J 28(6):659–660
Ertl G, Frantz S (2005) Healing after myocardial infarction. Cardiovasc Res 66:22–32
Vanhoutte D, Schellings M, Pinto Y, Heymans S (2006) Relevance of matrix metalloproteinases and their inhibitors after myocardial infarction: a temporal and spatial window. Cardiovasc Res 69:604–613
Panovsky R, Meluzin J, Janousek S et al (2008) Cell therapy in patients with left ventricular dysfunction due to myocardial infarction. Echocardiography 25:888–897
Vasku A, Goldbergova M, Izakovicova Holla L et al (2004) A haplotype constituted of four MMP-2 promoter polymorphisms (-1575G/A, -1306C/T, -790T/G, and –735C/T) is associated with coronary triple-vessel disease. Matrix Biol 22:585–591
Fedak PW, Szmitko PE, Weisel RD et al (2005) Cell implantation preserves matrix homeostasis: a novel paracrine mechanism. J Thorac Cardiovasc Surg 130:1430–1439
Uemura R, Xu M, Ahmad N, Ashraf M (2006) Bone marrow stem cells prevent left ventricular remodeling of ischemic heart through paracrine signaling. Circ Res 98:1414–1421
Li TS, Mikamo A, Takahashi M et al (2007) Comparison of cell therapy and cytosine therapy for functional repair in ischemic and nonischemic heart failure. Cell Transplant 16:365–374
Tse HF, Siu CW, Zhu SG et al (2007) Paracrine effects of direct intramyocardial implantation of bone marrow derived cells to enhance neovascularization in chronic ischaemic myocardium. Eur J Heart Fail 9:747–753
Kinnaird T, Stabile E, Burnett MS et al (2004) Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ Res 94:678–685
Misao Y, Takemura G, Arai M et al (2006) Bone marrow-derived myocyte-like cells and regulative of repair-related cytokines after bone marrow cell transplantation. Cardiovasc Res 69:476–490
Cheng AS, Yau TM (2008) Paracrine effects of cell transplantation: strategies to augment the efficacy of cell therapies. Semin Thorac Cardiovasc Surg 20(2):94–101
Rohde LE, Ducharme A, Arroyo LH et al (1999) Matrix metalloproteinase inhibition attenuates early left ventricular enlargement after experimental myocardial infarction in mice. Circulation 99:3063–3070
Mukherjee R, Brinsa TA, Dowdy KB et al (2003) Myocardial infarct expansion and matrix metalloproteinase inhibition. Circulation 107:618–625
Creemers EEJM, Cleutjens JPM, Smits JFM, Daemen MJAP (2001) Matrix metalloproteinase inhibition after myocardial infarction: a new approach to prevent heart failure? Circ Res 89:201–210
Frangogiannis NG, Shimoni S, Chang SM et al (2002) Active interstitial remodeling: an important process in the hibernating human myocardium. J Am Coll Cardiol 39(9):468–474
Chen J, Tung CH, Allport JR et al (2005) Near infrared fluorescent imaging of matrix metalloproteinase activity after myocardial infarction. Circulation 111:1800–1805
Yasuda S, Miyazaki S, Kinoshita H et al (2007) Enhanced cardiac production of matrix metalloproteinase-2 and –9 and its attenuation associated with pravastatin treatment in patients with acute myocardial infarction. Clin Sci 112(1–2):43–49
Matsunaga T, Abe N, Kameda K et al (2005) Circulating level of gelatinase activity predicts ventricular remodeling in patients with acute myocardial infarction. Int J Cardiol 105:203–208
Kai H, Ikeda H, Yusukawa H et al (1998) Peripheral blood levels of matrix metalloproteinases-2 and-9 are elevated in patients with acute coronary syndromes. J Am Coll Cardiol 32:368–372
Hayashidani S, Tsutsui H, lkeuchi M et al (2003) Targeted deletion of MMP-2 attenuates early LV rupture and late remodeling after experimental myocardial infarction. Am J Heart Circ Physiol 285:H 1229–H 1235
Matsumura S, lwanaga S, Mochizuki S et al (2005) Targeted deletion or’ pharmacological inhibition of MMP-2 prevents cardiac rupture after myocardial infarction in mice. J Clin Invest 115(3):599–609
Wagner RD, Delagardelle C, Ernens I et al (2006) Matrix metalloproteinase-9 is a marker of heart failure after acute myocardial infarction. J Cardiac Fail 12:66–72
Orn S, Manhenke C, Squire IB et al (2007) Plasma MMP-2, MMP-9 and N-BNP in long-term survivors following complicated myocardial infarction: Relation to cardiac magnetic resonance imaging measures of left ventricular structure and function. J Cardiac Fail 13(10):843–849
Kelly D, Cockerill G, Ng LL et al (2007) Plasma matrix metalloproteinase-9 and left ventricular remodeling after acute myocardial infarction in man: a prospective cohort study. Eur Heart J 28(6):711–718
Squire lB, Evans J, Ng LL et al (2004) Plasma MMP-9 and MMP-2 following acute myocardial infarction in man: correlation with echocardiographic and neurohumoral parameters of left ventricular dysfunction. J Cardiac Fail 10:328–333
Mizon-Gérard F, Groote P de, Lamblin N et al (2004) Prognostic impact of matrix metalloproteinase gene polymorphisms in patients with heart failure according to the etiology of left ventricular systolic dysfunction. Eur Heart J 25:688–693
Lamblin N, Bauters C, Hermant et al (2002) Polymorphisms in the promoter region of MMP-2, MMP-3, MMP-9 and MMP-12 genes as determinants of aneurysmal coronary artery disease. J Am Coll Cardiol 40:43–48
Bauters C, Lamblin N, Ennezat PV et al (2007) A prospective evaluation of left ventricular remodeling after inaugural anterior myocardial infarction as a function of gene polymorphisms in the renin-angiotensin-aldosterone, adrenergic, and metalloproteinase systems. Am Heart J 153(4):641–648
Perez-Ilzarbe M, Agbulut O, Pelacho B et al (2008) Characterization of the paracrine effects of human skeletal myoblasts transplanted in infarcted myocardium. Eur J Heart Fail 10:1065–1072
Davis GK, Millner RW, Roberts DH (2000) Angiotensin converting enzyme (ACE) gene expression in the human left ventricle: effect of ACE gene insertion/deletion polymorphism and left ventricular function. Eur J Heart Fail 2(3):253–256
Yoshida M, Iwai N, Ohmichi N et al (1999) D allele of the angiotensin-converting enzyme gene is a risk factor for secondary cardiac events after myocardial infarction. Int J Cardiol 70:119–125
Pinto YM, Gilst WH van, Kingma JH, Schunkert H (1995) Deletion-type allele of the angiotensin-converting enzyme gene is associated with progressive ventricular dilation after anterior myocardial infarction. Captopril and Thrombolysis Study Investigators. J Am CoIl Cardiol 25:1622–1626
Ohmichi N, Iwai N, Maeda K et al (1996) Genetic basis of left ventricular remodeling after myocardial infarction. Int J CardioI 53:265–272
Nagashima J, Musha H, So T et al (1999) Effect of angiotensin-converting enzyme gene polymorphism on left ventricular remodeling after anteroseptal infarction. Clin Cardiol 22:587–590
Samani NJ, Thompson JR, O’Toole L et al (1996) A meta-analysis of the association of the deletion allele of the angiotensin-converting enzyme gene with myocardial infarction. Circulation 94:708–712
Keavney B, McKenzie C, Parish S et al (2000) Large-scale test of hypothesized associations between the angiotensin-converting-enzyme insertion/deletion polymorphism and myocardial infarction in about 5000 cases and 6000 controls. Lancet 355:434–442
Zee RYL, Solomon SD, Ajani UA et al (2002) A prospective evaluation of the angiotensin-converting enzyme D/I polymorphism and left ventricular remodeling in the ‚Healing and Early Afterlood Reducing Therapy’ study. Clin Genet 61:21–25
Acknowledgements
The work was supported by a grant of the Ministry of Education of the Czech Republic No. MSM 0021622402.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Panovsky, R., Vasku, A., Meluzin, J. et al. Association of polymorphisms of zinc metalloproteinases with clinical response to stem cell therapy. Herz 35, 309–316 (2010). https://doi.org/10.1007/s00059-010-3353-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-010-3353-z