Abstract
Purpose
To compare failure rates and maximum load capacity (Fmax) of six different computer-aided design/computer-aided manufacturing (CAD/CAM) retainers with those of the hand-bent five-stranded stainless steel twistflex retainer.
Materials and methods
Six groups (n = 8 per group) of commercially available CAD/CAM retainers (cobalt–chromium [CoCr], titanium grade 5 [Ti5], nickel–titanium [NiTi], zirconia [ZrO2], polyetheretherketone [PEEK], and gold) and twistflex retainers were tested for long-term sufficiency and for Fmax using a self-developed in vitro model. All retainer models underwent a simulated ageing process of about 15 years (1,200,000 chewing cycles with a force magnitude of 65 N at 45° followed by storage in water at 37 °C for 30 days). If retainers did not debond or break during ageing, their Fmax was determined in a universal testing machine. Data were statistically analysed using Kruskal–Wallis and Mann–Whitney U‑tests.
Results
Twistflex retainers did not fail (0/8) during ageing and had the highest Fmax (445 N ± 51 N). Ti5 retainers were the only CAD/CAM retainers that also did not fail (0/8) and had similar Fmax values (374 N ± 62 N). All other CAD/CAM retainers had higher failure rates during ageing and significantly lower Fmax values (p < 0.01; ZrO2: 1/8, 168 N ± 52 N; gold: 3/8, 130 N ± 52 N; NiTi: 5/8, 162 N ± 132 N; CoCr: 6/8, 122 N ± 100 N; PEEK: 8/8, 65 ± 0 N). Failure was due to breakage in the NiTi retainers and debonding in all other retainers.
Conclusion
Twistflex retainers remain the gold standard regarding biomechanical properties and long-term sufficiency. Of the CAD/CAM retainers tested, Ti5 retainers seem to be the most suitable alternative. In contrast, all other CAD/CAM retainers investigated in this study showed high failure rates and had significantly lower Fmax values.
Zusammenfassung
Zielsetzung
Vergleich der Versagensraten und der maximalen Belastbarkeit (Fmax) von 6 unterschiedlichen CAD/CAM(„computer-aided design/computer-aided manufacturing“)-Retainern mit denen eines handgebogenen 5‑strängigen Twistflex-Retainers aus Edelstahl.
Material und Methoden
Sechs Gruppen (n = 8 pro Gruppe) kommerziell verfügbarer CAD/CAM-Retainer (Kobalt-Chrom [CoCr], Titan Grade 5 [Ti5], Nickel-Titan [NiTi], Zirkoniumdioxid [ZrO2], Polyetheretherketon [PEEK] und Gold) und Twistflex-Retainer wurden anhand eines selbst entwickelten In-vitro-Modells auf ihre Langzeitstabilität und auf Fmax getestet. Alle Retainermodelle wurden einem simulierten Alterungsprozess von etwa 15 Jahren unterzogen (1.200.000 Kauzyklen mit einer Kraft von 65 N bei 45 °, gefolgt von einer 30-tägigen Lagerung in Wasser bei 37 °C). Wenn sich die Retainer während der Alterung nicht ablösten oder brachen, wurde ihre Fmax in einer Universalprüfmaschine bestimmt. Die Daten wurden mit Kruskal-Wallis- und Mann-Whitney-U-Tests statistisch ausgewertet.
Ergebnisse
Twistflex-Retainer versagten während der Alterung nicht (0/8) und hatten die höchste Fmax (445 N ± 51 N). Ti5-Retainer waren die einzigen CAD/CAM-Retainer, die ebenfalls nicht versagten (0/8) und ähnliche Fmax-Werte aufwiesen (374 N ± 62 N). Alle anderen CAD/CAM-Retainer hatten höhere Versagensquoten während der Alterung und signifikant niedrigere Fmax-Werte (p < 0,01; ZrO2: 1/8, 168 N ± 52 N; Gold: 3/8, 130 N ± 52 N; NiTi: 5/8, 162 N ± 132 N; CoCr: 6/8, 122 N ± 100 N; PEEK: 8/8, 65 ± 0 N). Das Versagen war bei den NiTi-Retainern auf Brechen, bei allen anderen Retainern auf Debonding zurückzuführen.
Schlussfolgerung
Twistflex-Retainer sind nach wie vor der Goldstandard im Hinblick auf biomechanische Eigenschaften und Langzeitstabilität. Von den getesteten CAD/CAM-Retainern scheinen Ti5-Retainer die am besten geeignete Alternative. Im Gegensatz dazu wiesen alle anderen untersuchten CAD/CAM-Retainer hohe Versagensquoten und deutlich niedrigere Fmax-Werte auf.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Digital techniques are being increasingly integrated into diagnostics and treatment in orthodontics. For example, fully automated digital cephalometric analysis [1] or digital model analysis [2] has been used in diagnostics, and computer-aided design and manufacturing (CAD/CAM) technology has been used to design and fabricate treatment devices. CAD/CAM technology has many applications in orthodontics, including anchoring appliances [3], customised archwires [4] and brackets [5,6,7], which can be placed intraorally by CAD/CAM-produced bonding trays [8,9,10]. We recently introduced a CAD/CAM-fabricated functional regulator 3 (CAD-FR3), which extended CAD/CAM application to the production of removable functional appliances [11]. Aligners can also be produced by CAD/CAM, since the different therapy steps and respective models are planned digitally and manufactured using a three-dimensional (3D) printer [12, 13].
Fixed orthodontic CAD/CAM retainers, which are made from various materials including polyetheretherketone (PEEK) [14, 15], nickel–titanium (NiTi) [16,17,18,19], and zirconia (ZrO2) [20], have emerged as potential alternatives to hand-bent retainers in the last few years. These CAD/CAM retainers have been considered advantageous because of their high-precision fit in demanding situations [21] and because they can be produced automatically by the technician without bending. However, it is important to consider long-term survival rates because retainers can only provide long-term retention if they restrain physiological mastication forces over a long time.
It remains unclear whether CAD/CAM retainers have better long-term survival than hand-bent retainers because studies have only evaluated CAD/CAM retainers for up to one year [17, 19, 22, 23]. This is not sufficient because a retainer may fail years after the orthodontic treatment is finished [24]. Thereby retainer failure can cause complications such as orthodontic relapse [24] or enamel damage caused by the removal of retainers [25]. It is moreover important to note here that complications might not be detected by the orthodontist, since the orthodontic therapy was usually finished years before, and therefore the anterior alignment may relapse. To avoid these complications, it is important to evaluate the long-term survival of different retainers to recommend future treatment.
The aim of the present study was to compare the long-term stability of six novel CAD/CAM retainers with that of the conventional five-stranded twistflex retainer in an in vitro approach. For each tested retainer, the failure rate was recorded during a simulated ageing process and maximal load capacity values (Fmax) were determined. The null hypothesis was that conventional twistflex retainers show inferior performance regarding failure rate and Fmax compared to CAD/CAM retainers.
Materials and methods
Test model for the investigation
For the investigation, a CAD/CAM in vitro model was developed to test the retainers. The model consisted of six artificial teeth (canine to canine) of a lower jaw embedded in a model base (Fig. 1). The model base and the artificial teeth were digitally planned (Geomagic Design X; 3D Systems, Rock Hill, SC, USA) and manufactured separately. The teeth provided planar loading sites on the vestibular surface and were milled from fibre-reinforced composite discs (FRCs; Trinia, Bicon, Boston, MA, USA). The FRCs were tested in advance with the recommended primer (Ceraresin Bond 1&2, Shofu, Tokyo, Japan) and a dental composite (Transbond XT) according to DIN 13990‑1 and had a similar shear bond strength (18.0 ± 2.4 MPa) to that of the clinical situation [26, 27].
In vitro tooth model. The model base and the teeth were planned and manufactured using computer-aided design/computer-aided manufacturing (CAD/CAM) technology. The model base contained flexible bars that simulated physiological tooth mobility (a). All teeth provided planar loading sites on the vestibular surface and were embedded in the model base (b). Retainers were bonded on the models (c)
In-vitro-Zahnmodell. Der Modellsockel und die Zähne wurden mit Hilfe der CAD/CAM(„computer-aided design/computer-aided manufacturing“)-Technologie geplant und hergestellt. Die Modelbasis war mit nachgiebigen Stegen konstruiert, um die physiologische Zahnbeweglichkeit zu simulieren (a). Alle Zähne wurden vestibulär und inzisal mit planen Belastungsflächen konstruiert und waren in den Modellsockel eingebettet (b). Die Retainer wurden auf die Modelle geklebt (c)
The model base was made of resin (Biomed Clear Resin, Formlabs, Somerville, MA, USA) and was manufactured using a stereolithography printer (Form 3B, Formlabs, Somerville, MA, USA). Each tooth was placed and bonded into a socket, which was held by flexible horizontal bars. The bar dimensions (width: 3 mm; height: 1.7 mm) and the vertical distance between the bars (2.6 mm) were adjusted to allow physiological tooth mobility. Tooth mobility was tested in all models (three teeth per model) before the main experiments began and all models had comparable tooth mobility to that of the clinical situation [28]: horizontal tooth mobility: 0.36 ± 0.06 mm/100 N; axial tooth mobility: 0.11 ± 0.01 mm/100 N. We also tested whether the models could withstand cyclic mastication forces (1,200,000 cycles, 60 N) and maximum mastication forces above 500 N, which exceeds the physiological mastication forces in the incisal area of about 230 N [29]. For every retainer, eight in vitro tooth models (56 models in total) were produced and tested.
Building the sample
The twistflex retainers were bent by hand onto each in vitro model. For the CAD/CAM retainers, all in vitro tooth models were scanned with an intraoral scanner (Trios 4, 3Shape, Copenhagen, Hovedstaden, Denmark) and a separate standard tessellation language (STL) file was generated for each model. The STL files were sent to the manufacturers. Eight CAD/CAM retainers were made from each of the six materials. These materials were cobalt–chromium (CoCr), gold, titanium grade 5 (Ti5), nickel–titanium (NiTi), polyetheretherketone (PEEK) and zirconia (ZrO2) (Table 1, Fig. 2).
Tested retainers—conventional twistflex retainers (a) and six commercially available computer-aided design/computer-aided manufacturing (CAD/CAM) retainers (b–f) were tested. The CAD/CAM retainers were made from cobalt–chromium (b), gold (c), titanium grade 5 (d), nickel–titanium (e), polyetheretherketone (f) and zirconia (g)
Die getesteten Retainer – herkömmliche Twistflex-Retainer (a) und 6 kommerziell erhältliche CAD/CAM(„computer-aided design/computer-aided manufacturing“)-Retainer (b–f). Die CAD/CAM-Retainer waren aus Kobalt-Chrom (b), Gold (c), Titan Grad 5 (d), Nickel-Titan (e), Polyetheretherketon (f) und Zirkoniumdioxid (g) gefertigt
Before the retainers were bonded to the models, all model teeth were sandblasted (50 μm alumina particles, 1 bar) and conditioned with a primer (Ceraresin Bond 1&2, Shofu, Tokyo, Japan) as previously described [26]. NiTi, Ti5, gold, PEEK, and twistflex retainers were bonded with composite (Transbond XT, 3M, Saint Paul, MN, USA) and light cured with a dental light curing device (460 nm; Smartlite focus; Dentsply Sirona, Charlotte, NC, USA) for 40 s on every tooth according to previous studies [26, 30]. ZrO2 retainers were prepared with tribochemical silica coating using Rocatec (RC; 3M ESPE; Seefeld, Germany) on the bonding site: RC Pre (lot 467012, 0.28 MPa, distance: 10 mm, duration: 10 s, angle: 45°) and RC Plus (lot 432661, 0.28 MPa, distance: 10 mm, duration: 13 s, angle: 45°). Afterwards, the primer (Clearfil Ceramic Primer Plus, Kuraray Noritake, Tokyo, Japan) and the composite cement (Panavia V5, Kuraray Noritake, Tokyo, Japan) were successively applied onto the ZrO2 retainers. ZrO2 retainers were placed onto the corresponding model and light cured for 40 s (Smartlite focus, Dentsply Sirona, Charlotte, NC, USA) from four directions on every tooth as previously described [31] and excess cement was removed. The whole bonding procedure was performed by the same dentist in accordance with the manufacturers’ instructions.
Ageing and load capacity testing
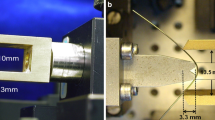
After bonding, all retainer models underwent the following standardised ageing process (Fig. 3a,b):
-
1,200,000 chewing cycles (force magnitude 65 N, loading direction tilted by 45° to the vertical axis; CS‑4, SD Mechatronik, Feldkirchen-Westerham, Germany) were exerted on tooth 31. During chewing simulation, the model was immersed in water at room temperature (23 ± 1 °C).
-
Water storage for 30 days at body temperature (37 ± 1 °C).
Testing protocol: to simulate 15 years of wearing time, all retainer models were loaded 1,200,000 times in a chewing simulator in water (for better visibility photo in a was taken without water in chambers) (a, b). Retainers that were not damaged by the ageing process were further loaded in a universal testing device until retainer debonding or breakage was detected (c)
Prüfprotokoll: Um eine Tragezeit von 15 Jahren zu simulieren, wurden alle Retainermodelle 1.200.000-mal in einem Kausimulator in Wasser belastet (zur besseren Sichtbarkeit wurde das Foto in a ohne Wasser in den Kammern aufgenommen) (a, b). Retainer, die durch den Alterungsprozess nicht beschädigt wurden, wurden daraufhin in einem Universalprüfgerät weiter belastet, bis ein Klebeversagen oder ein Bruch festgestellt wurde (c)
After the ageing process, the models were checked for failures, i.e. retainer fracture or debonding. In retainer models that did not fracture or debond during ageing, the fracture resistance Fmax of tooth 31 was tested in a universal testing machine (Zwick, Roell, Ulm, Germany; Fig. 3c). High loads generally correspond to axial forces, so the load was applied on tooth 31 with a steel piston in a vertical direction. The crosshead was lowered with a speed of 2 mm/min until a drop-in test force ≥ 20% of the maximum test force occurred.
Statistical evaluation
Statistical analysis was performed using SPSS statistics 27 (IBM, Armonk, NY, USA). Fmax values were compared between the different groups of retainers. In line with previous studies and because of statistical reasons [32, 33], retainers that failed during the ageing process were associated with a load capacity of Fmax = 65 N. Data were analysed using Kruskal–Wallis tests first in order to find general effects. Afterwards pairwise Mann–Whitney U‑tests were used to compare twistflex retainers to the individual CAD/CAM retainers. Multiple testing was excluded by using Bonferroni correction. The significance level was set to p = 0.05.
Results
Twistflex retainers did not fail during the ageing process and had the highest Fmax values (445.8 ± 51.2 N; Figs. 4 and 5). Ti5 retainers were the only CAD/CAM retainers that also did not fail during ageing and had similar Fmax values to twistflex retainers (374.0 ± 62.4 N). All other CAD/CAM retainers failed to varying extents during ageing and had significantly lower Fmax values than twistflex retainers did (p < 0.01). Of these failed retainers, ZrO2 retainers had the lowest failure rates (1/8; Fmax = 168.8 ± 52.4 N) followed by gold retainers (3/8; Fmax = 130.2 ± 51.8 N), NiTi retainers (5/8; Fmax = 162.2 ± 132.6 N), CoCr retainers (6/8; Fmax = 122.27 ± 100.5 N) and PEEK retainers (8/8; Fmax = 65 ± 0 N).
Number of retainer failures during ageing—Twistflex retainers and computer-aided design/computer-aided manufacturing (CAD/CAM) titanium grade 5 retainers were the only retainers which did not fail during the ageing process. Of the CAD/CAM retainers that failed, ZrO2 retainers had the lowest failure rate and polyetheretherketone (PEEK) retainers had the highest failure rate
Anzahl der Retainerausfälle während der Alterung – Twistflex-Retainer und CAD/CAM(„computer-aided design/computer-aided manufacturing“)-Retainer aus Titan Grad 5 waren die einzigen Retainer, die während des Alterungsprozesses nicht versagten. Unter den anderen CAD/CAM-Retainern zeigten ZrO2-CAD/CAM-Retainer die geringsten und PEEK(Polyetheretherketon)-Retainer die höchsten Versagensraten
Load capacity (Fmax) testing—Twistflex retainers had the highest Fmax values. Titanium grade 5 retainers were the only computer-aided design/computer-aided manufacturing (CAD/CAM) retainers with a comparable Fmax to twistflex retainers. All other CAD/CAM retainers had significantly lower Fmax values (*). Retainers that failed during the ageing process were associated with a load capacity of Fmax = 65 N.
Prüfung der Maximalbelastung (Fmax) – Twistflex-Retainer zeigten die größten Fmax-Werte. Retainer aus Titan Grad 5 zeigten als einzige CAD/CAM(„computer-aided design/computer-aided manufacturing“)-Retainer vergleichbare Fmax-Werte zu Twistflex-Retainern. Alle anderen CAD/CAM-Retainer zeigten signifikant geringere Fmax-Werte (*). Retainer, die während des Alterungsprozesses versagten, wurde eine Fmax von 65 N zugewiesen
The CAD/CAM retainers failed because of debonding during ageing and Fmax testing, except for the NiTi retainers, which failed because of breakage or debonding (5/8 broke during ageing, 1/8 broke during Fmax testing and 2/8 debonded during Fmax testing). The moment of failure is illustrated in Fig. 6.
Event of failure during load capacity (Fmax) testing—Twistflex (a), cobalt–chromium (b), gold (c), titanium grade 5 (d), and zirconia (f) computer-aided design/computer-aided manufacturing (CAD/CAM) retainers failed because of debonding. NiTi retainers (e) were the only CAD/CAM retainers which failed because of breakage or debonding. Polyetheretherketone (PEEK) CAD/CAM retainers were not tested for Fmax, since all failed during ageing
Moment des Versagens unter Maximalbelastung (Fmax) – Twistflex (a), Kobalt-Chrom (b), Gold (c), Titan Grad 5 (d) und Zirkoniumdioxid (f) CAD/CAM(„computer-aided design/computer-aided manufacturing”)-Retainer versagten alle aufgrund von Debonding. NiTi-Retainer (e) waren die einzigen CAD/CAM-Retainer, die neben einem Debonding auch Brüche zeigten. PEEK(Polyetheretherketon)-CAD/CAM-Retainer wurden nicht auf Fmax getestet, da sie alle bereits während des Alterungsprozesses durch Debonding versagten
Discussion
The null hypothesis had to be rejected because conventional five-stranded stainless steel twistflex retainers showed the highest Fmax values and demonstrated no failure during simulated ageing. Therefore, conventional five-stranded stainless steel twistflex retainers can still be considered as the gold standard, which is in line with the recommendation by Zachrisson et al., which was based on their 20 years of experience with multistranded retainer wires [34]. We showed that most CAD/CAM retainers (except for Ti5 retainers) presented higher failure rates during ageing and significantly lower Fmax values (p < 0.01) than twistflex retainers. Based on these findings, only Ti5 CAD/CAM retainers can be considered a valid alternative to conventional hand-bent twistflex retainers.
There are several methodological strengths to this study. First, to the best of our knowledge, this is the first study to investigate the survival of multiple CAD/CAM retainers and compare these survival rates with those of the conventional twistflex retainer. Previous studies have only investigated NiTi [17, 19, 22, 23] or PEEK CAD/CAM retainers [15] and other studies were individual case reports presenting single CAD/CAM retainers made from PEEK [14], NiTi [16] or ZrO2 [20]. In contrast, we tested a representative sample of six different CAD/CAM retainers with standardised experimental procedures and reliable in vitro comparisons. Because of the reliability of our experimental setup, we decided not to compare these six CAD/CAM retainers in a clinical trial. Long-term clinical trials often suffer from limited standardisation, including factors like differences in chewing behaviour/forces or differences in treatment prior to retention. In addition, informative results from clinical trials are only possible after a long observation time.
Another strength of our methodology is that in vitro tooth models were specifically developed for this study and tooth mobility was tested in every model before the main investigation started. These tests confirmed the physiological mobility of the model teeth, showing that the model was valid for clinical simulation. The model could also test the retainers in their whole geometry, like in the patient. Previous studies have not taken into account physiological tooth mobility [35,36,37,38,39] and have not tested the whole geometry of the retainers but rather just on one [25], two [35,36,37] or three teeth [39]. However, not considering the whole geometry of the retainer and the physiological mobility of the teeth can affect the biomechanical behaviour of the retainer and produce misleading results. These earlier studies may have been limited by the availability of extracted human teeth. We avoided this limitation by investigating alternatives to human teeth in a previous study [26] and found FRC an ideal material for the production of teeth for in vitro testing because its bonding strength (18.0 ± 2.4 MPa) was comparable to that of the clinical situation [27]. Using CAD/CAM teeth also allowed us to use the same geometries for all models, ensuring standardised experimental conditions.
To the best of our knowledge, this is the first study to use a chewing simulator to investigate orthodontic devices. Therefore, we were able to simulate 15 years of wearing time, which tells us far more about the long-term survival of retainers than previous studies have, with follow-up times limited to 1 year [17] or 6 months [19, 22, 23]. This longer observation time might also explain why previous studies did not detect differences in the survival rates between twistflex and CAD/CAM NiTi retainers. Using our highly standardised in vitro model, we showed that, except for Ti5 retainers, CAD/CAM retainers result in higher long-term failure rates than twistflex retainers, which within our study, showed no failure at all.
Our study revealed that NiTi CAD/CAM retainers are more prone to breakage than other CAD/CAM retainers. This has important implications in the clinical situation because NiTi CAD/CAM retainers may need to be removed instead of just rebonded after breakage resulting in increasing costs and burden for the patient and time and effort for the practitioner. Also, the low Fmax values of CAD/CAM retainers might have clinical consequences. This is because the Fmax values in all tested CAD/CAM retainers (except for Ti5 retainers) were lower than the maximal incisor bite force of about 200 N [40,41,42]. In ZrO2 retainers, these low Fmax values seem to make them less suitable for long-term retention, although they were largely resistant to ageing.
Of note, debonding and breakage were not visually detectable during the initial chewing simulation but rather later on during the Fmax testing. For the detachment of ZrO2, CoCr, PEEK and gold retainers, this might have been caused by the stiffness and bulkiness of these retainers, which prevented visual inspection of the bonding area. In NiTi retainers, breaking during ageing was undetected because of their high springback properties, which returned the retainer to its original form as soon as the load was released. Undetected debonding and breakage in CAD/CAM retainers may be problematic because the patient may not notice the failure until the teeth begin to move. The orthodontist will also not notice the failure if the orthodontic therapy was finalised years ago and regular control visits have already been discontinued.
Finally, when interpreting the results of the present study, it has to be considered that although our model aimed to simulate the clinical situation as closely as possible, this was still an in vitro study, so drawing specific clinical conclusions is limited. Although the CAD/CAM teeth used in the present study were validated for having similar bonding strength values as compared to human and bovine teeth [26], there were still slight differences with respect to the adhesive remnant index. Second, we tested CAD/CAM retainers that are commercially available to give our readers the information they need to protect their patients from unnecessary burdens. This is why we refrained including own design preferences to the respective manufacturers. However, modifying the design or using other materials for the production might affect the biomechanical behaviour and therefore the survival of CAD/CAM retainers, which should be investigated in future studies.
Conclusions
The results of the present in vitro study have shown that
-
Twistflex retainers showed no failure during the ageing process and demonstrated the highest maximum load capacity of all retainers tested. Therefore, twistflex retainers should remain the gold standard for long-term sufficiency.
-
Ti5 retainers were the only computer-aided design/computer-aided manufacturing (CAD/CAM) retainers that did not fail during the ageing process and had similar load capacity values to the twistflex retainer. Therefore, Ti5 CAD/CAM retainers may represent a suitable alternative.
-
NiTi, ZrO2, gold, CoCr and polyetheretherketone (PEEK) CAD/CAM retainers all failed during ageing and had significantly lower Fmax values than twistflex retainers; therefore, the long-term sufficiency of these retainers may be limited.
References
Kunz F, Stellzig-Eisenhauer A, Zeman F, Boldt J (2020) Artificial intelligence in orthodontics: Evaluation of a fully automated cephalometric analysis using a customized convolutional neural network. J Orofac Orthop 81(1):52–68. https://doi.org/10.1007/s00056-019-00203-8
Meyer S (2010) Retrospektive methodische Studie zum Vergleich von digitaler und manueller Modellanalyse in der Kieferorthopädie
Graf S, Vasudavan S, Wilmes B (2018) CAD-CAM design and 3‑dimensional printing of mini-implant retained orthodontic appliances. Am J Orthod Dentofacial Orthop 154(6):877–882. https://doi.org/10.1016/j.ajodo.2018.07.013
Muller-Hartwich R, Jost-Brinkmann PG, Schubert K (2016) Precision of implementing virtual setups for orthodontic treatment using CAD/CAM-fabricated custom archwires. J Orofac Orthop 77(1):1–8. https://doi.org/10.1007/s00056-015-0001-5
Sha HN, Choi SH, Yu HS, Hwang CJ, Cha JY, Kim KM (2018) Debonding force and shear bond strength of an array of CAD/CAM-based customized orthodontic brackets, placed by indirect bonding—An In Vitro study. PLoS ONE 13(9):e202952. https://doi.org/10.1371/journal.pone.0202952
Sha HN, Lim SY, Kwon SM, Cha JY (2019) Camouflage treatment for skeletal Class III patient with facial asymmetry using customized bracket based on CAD/CAM virtual orthodontic system: A case report. Angle Orthod. https://doi.org/10.2319/102318-768.1
Brown MW, Koroluk L, Ko CC, Zhang K, Chen M, Nguyen T (2015) Effectiveness and efficiency of a CAD/CAM orthodontic bracket system. Am J Orthod Dentofacial Orthop 148(6):1067–1074. https://doi.org/10.1016/j.ajodo.2015.07.029
Bozelli JV, Bigliazzi R, Barbosa HA, Ortolani CL, Bertoz FA, Faltin Junior K (2013) Comparative study on direct and indirect bracket bonding techniques regarding time length and bracket detachment. Dental Press J Orthod 18(6):51–57. https://doi.org/10.1590/s2176-94512013000600009
Deahl ST, Salome N, Hatch JP, Rugh JD (2007) Practice-based comparison of direct and indirect bonding. Am J Orthod Dentofacial Orthop 132(6):738–742. https://doi.org/10.1016/j.ajodo.2006.01.037
Li Y, Mei L, Wei J, Yan X, Zhang X, Zheng W, Li Y (2019) Effectiveness, efficiency and adverse effects of using direct or indirect bonding technique in orthodontic patients: a systematic review and meta-analysis. BMC Oral Health 19(1):137. https://doi.org/10.1186/s12903-019-0831-4
Roser C, Hodecker LD, Koebel C, Lux CJ, Ruckes D, Rues S, Zenthofer A (2021) Mechanical properties of CAD/CAM-fabricated in comparison to conventionally fabricated functional regulator 3 appliances. Sci Rep 11(1):14719. https://doi.org/10.1038/s41598-021-94237-x
Ercoli F, Tepedino M, Parziale V, Luzi C (2014) A comparative study of two different clear aligner systems. Prog Orthod 15(1):31. https://doi.org/10.1186/s40510-014-0031-3
Robertson L, Kaur H, Fagundes NCF, Romanyk D, Major P, Flores Mir C (2020) Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod Craniofac Res 23(2):133–142. https://doi.org/10.1111/ocr.12353
Aboulazm K, von See C, Othman A (2021) Fixed lingual orthodontic retainer with bilateral missing lateral incisors produced in PEEK material using CAD/CAM technology. J Clin Exp Dent 13(6):e549–e551. https://doi.org/10.4317/jced.58035
Kadhum AS, Alhuwaizi AF (2021) The efficacy of polyether-ether-ketone wire as a retainer following orthodontic treatment. Clin Exp Dent Res 7(3):302–312. https://doi.org/10.1002/cre2.377
Kravitz ND, Grauer D, Schumacher P, Jo YM (2017) Memotain: A CAD/CAM nickel-titanium lingual retainer. Am J Orthod Dentofacial Orthop 151(4):812–815. https://doi.org/10.1016/j.ajodo.2016.11.021
Gelin E, Seidel L, Bruwier A, Albert A, Charavet C (2020) Innovative customized CAD/CAM nickel-titanium lingual retainer versus standard stainless-steel lingual retainer: A randomized controlled trial. Korean J Orthod 50(6):373–382. https://doi.org/10.4041/kjod.2020.50.6.373
Kartal Y, Kaya B (2019) Fixed orthodontic retainers: a review. Turk J Orthod 32(2):110–114. https://doi.org/10.5152/TurkJOrthod.2019.18080
Knaup I, Wagner Y, Wego J, Fritz U, Jager A, Wolf M (2019) Potential impact of lingual retainers on oral health: comparison between conventional twistflex retainers and CAD/CAM fabricated nitinol retainers: A clinical in vitro and in vivo investigation. J Orofac Orthop 80(2):88–96. https://doi.org/10.1007/s00056-019-00169-7
Zreaqat M, Hassan R, Hanoun AF (2017) A CAD/CAM zirconium bar as a bonded mandibular fixed retainer: a novel approach with two-year follow-up. Case Rep Dent 2017:1583403. https://doi.org/10.1155/2017/1583403
Wolf M, Schumacher P, Jager F, Wego J, Fritz U, Korbmacher-Steiner H, Jager A, Schauseil M (2015) Novel lingual retainer created using CAD/CAM technology: evaluation of its positioning accuracy. J Orofac Orthop 76(2):164–174. https://doi.org/10.1007/s00056-014-0279-8
Kartal Y, Kaya B, Polat-Ozsoy O (2021) Comparative evaluation of periodontal effects and survival rates of Memotain and five-stranded bonded retainers: A prospective short-term study. J Orofac Orthop 82(1):32–41. https://doi.org/10.1007/s00056-020-00243-5
Alrawas MB, Kashoura Y, Tosun O, Oz U (2020) Comparing the effects of CAD/CAM nickel-titanium lingual retainers on teeth stability and periodontal health with conventional fixed and removable retainers: A randomized clinical trial. Orthod Craniofac Res. https://doi.org/10.1111/ocr.12425
Booth FA, Edelman JM, Proffit WR (2008) Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop 133(1):70–76. https://doi.org/10.1016/j.ajodo.2006.10.023
Chinvipas N, Hasegawa Y, Terada K (2014) Repeated bonding of fixed retainer increases the risk of enamel fracture. Odontology 102(1):89–97. https://doi.org/10.1007/s10266-012-0095-9
Roser CJ, Rückschloß T, Zenthöfer A, Rammelsberg P, Lux CJ, Rues S (2022) Orthodontic shear bond strength and ultimate load tests of CAD/CAM produced artificial teeth. Clin Oral Invest. https://doi.org/10.1007/s00784-022-04676-7
Paradella TC, Fava M (2007) Bond strength of adhesive systems to human tooth enamel. Braz Oral Res 21(1):4–9. https://doi.org/10.1590/s1806-83242007000100001
Boldt J, Knapp W, Proff P, Rottner K, Richter EJ (2012) Measurement of tooth and implant mobility under physiological loading conditions. Ann Anat 194(2):185–189. https://doi.org/10.1016/j.aanat.2011.09.007
Kiliaridis S, Johansson A, Haraldson T, Omar R, Carlsson GE (1995) Craniofacial morphology occlusal traits, and bite force in persons with advanced occlusal tooth wear. Am J Orthod Dentofacial Orthop 107(3):286–292. https://doi.org/10.1016/S0889-5406(95)70144-3
Reicheneder C, Hofrichter B, Faltermeier A, Proff P, Lippold C, Kirschneck C (2014) Shear bond strength of different retainer wires and bonding adhesives in consideration of the pretreatment process. Head Face Med 10:51. https://doi.org/10.1186/1746-160X-10-51
Bomicke W, Schurz A, Krisam J, Rammelsberg P, Rues S (2016) Durability of resin-zirconia bonds produced using methods available in dental practice. J Adhes Dent 18(1):17–27. https://doi.org/10.3290/j.jad.a35517
Kohal RJ, Finke HC, Klaus G (2009) Stability of prototype two-piece zirconia and titanium implants after artificial aging: an in vitro pilot study. Clin Implant Dent Relat Res 11(4):323–329. https://doi.org/10.1111/j.1708-8208.2008.00116.x
Schwindling FS, Rues S, Schmitter M (2017) Fracture resistance of glazed, full-contour ZLS incisor crowns. J Prosthodont Res 61(3):344–349. https://doi.org/10.1016/j.jpor.2016.12.008
Zachrisson BU (2015) Multistranded wire bonded retainers: from start to success. Am J Orthod Dentofacial Orthop 148(5):724–727. https://doi.org/10.1016/j.ajodo.2015.07.015
Aldrees AM, Al-Mutairi TK, Hakami ZW, Al-Malki MM (2010) Bonded orthodontic retainers: a comparison of initial bond strength of different wire-and-composite combinations. J Orofac Orthop 71(4):290–299. https://doi.org/10.1007/s00056-010-9947-5
Baysal A, Uysal T, Gul N, Alan MB, Ramoglu SI (2012) Comparison of three different orthodontic wires for bonded lingual retainer fabrication. Korean J Orthod 42(1):39–46. https://doi.org/10.4041/kjod.2012.42.1.39
Cooke ME, Sherriff M (2010) Debonding force and deformation of two multi-stranded lingual retainer wires bonded to incisor enamel: an in vitro study. Eur J Orthod 32(6):741–746. https://doi.org/10.1093/ejo/cjq017
Mohlhenrich SC, Jager F, Jager A, Schumacher P, Wolf M, Fritz U, Bourauel C (2018) Biomechanical properties of CAD/CAM-individualized nickel-titanium lingual retainers: an in vitro study. J Orofac Orthop 79(5):309–319. https://doi.org/10.1007/s00056-018-0144-2
Milheiro A, de Jager N, Feilzer AJ, Kleverlaan CJ (2015) In vitro debonding of orthodontic retainers analyzed with finite element analysis. Eur J Orthod 37(5):491–496. https://doi.org/10.1093/ejo/cju074
Helkimo E, Carlsson GE, Helkimo M (1977) Bite force and state of dentition. Acta Odontol Scand 35(6):297–303. https://doi.org/10.3109/00016357709064128
Kiliaridis S, Kjellberg H, Wenneberg B, Engstrom C (1993) The relationship between maximal bite force, bite force endurance, and facial morphology during growth—A cross-sectional study. Acta Odontol Scand 51(5):323–331. https://doi.org/10.3109/00016359309040583
Regalo SC, Santos CM, Vitti M, Regalo CA, de Vasconcelos PB, Mestriner W Jr., Semprini M, Dias FJ, Hallak JE, Siessere S (2008) Evaluation of molar and incisor bite force in indigenous compared with white population in Brazil. Arch Oral Biol 53(3):282–286. https://doi.org/10.1016/j.archoralbio.2007.10.003
Acknowledgements
We thank the Wissenschaftsfonds of the DGKFO e. V. for their support, which made this investigation possible.
Funding
This study was funded by the Wissenschaftsfonds of the Deutsche Gesellschaft für Kieferorthopädie e. V.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.J. Roser, C. Bauer, L. Hodecker, A. Zenthöfer, C.J. Lux and S. Rues declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roser, C.J., Bauer, C., Hodecker, L. et al. Comparison of six different CAD/CAM retainers vs. the stainless steel twistflex retainer: an in vitro investigation of survival rate and stability. J Orofac Orthop (2023). https://doi.org/10.1007/s00056-023-00486-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00056-023-00486-y
Keywords
- Computer-aided design/computer-aided manufacturing
- Orthodontic treatment
- Bonded retainer
- Breakage
- Fixed orthodontic appliances