Abstract
Objective
To test the null hypothesis that children with Class I, II, and III malocclusions who have not undergone orthodontic therapy present with displaced discs.
Materials and methods
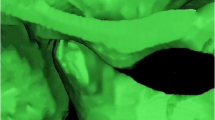
This study relied on retrospective material consisting of 76 unilateral left sagittal–oblique temporomandibular joint (TMJ) magnetic resonance imaging (MRIs) and lateral cephalometric radiographs taken in maximum intercuspal position in patients with clinically symptom-free and orthodontically untreated Class I (n = 30; 19 girls and 11 boys), Class II (n = 26; 10 girls and 16 boys), and Class III malocclusion (n = 20; 5 girls and 15 boys). The mean ages of patients with Class I, II, and III malocclusions were 10.55 ± 0.81, 11.71 ± 0.31, and 8.98 ± 1.80 years, respectively. Study groups were compared with one-way ANOVA analysis or Welch ANOVA test. Differences were evaluated via the Tukey HSD or Games–Howell test.
Results
Disc–condyle positions were almost within normal limits in Class I malocclusion. The disc was positioned anteriorly relative to the condyle (p < 0.05) and the condyle positioned posteriorly in the glenoid fossa in Class II malocclusion (p < 0.05). The disc was positioned slightly anteriorly relative to the condyle (p < 0.05) and the condyle was positioned posteriorly in the glenoid fossa in Class III malocclusion. Disc–condyle positions were observed to be almost identical in all three malocclusion classes.
Conclusion
Disc–condyle position was nearly normal in patients with Class I malocclusion. Nevertheless, a Class II malocclusion is more apt to reveal anterior disc displacement than a Class III malocclusion.
Zusammenfassung
Ziel
Überprüft werden sollte die Nullhypothese, dass nicht kieferorthopädisch behandelte Kinder mit Klasse-I-, -II- und -III-Malokklusion eine Diskusverlagerung aufweisen.
Material und Methoden
Das in der Studie retrospektiv untersuchte Material bestand aus 76 magnetresonanztomographischen Aufnahmen (MRT; unilateral links, schräg sagittal) des Kiefergelenkes (TMJ) und Fernröntgenseitaufnahmen von klinisch symptomfreien Patienten mit noch nicht kieferorthopädisch behandelter Klasse-I- (n = 30; 19 Mädchen, 11 Jungen), Klasse-II- (n = 26; 10 Mädchen, 16 Jungen) und Klasse-III-Malokklusion (n = 20; 5 Mädchen, 15 Jungen). Das durchschnittliche Lebensalter lag bei 10,55 ± 0,81, 11,71 ± 0,31 und 8,98 ± 1,80 Jahren. Die Gruppen wurden mit der Einwege-ANOVA-Analyse bzw. dem Welch-ANOVA-Test verglichen, Unterschiede wurden mit dem Tukey-HSD- bzw. dem Games-Howell-Test ausgewertet.
Ergebnisse
Die Kondylus-Diskus-Position war bei Klasse-I-Patienten fast im Normbereich. Bei Klassse-II-Malokklusion lag der Diskus relativ zum Kondylus anterior (p < 0,05), und der Kondylus war posterior positioniert in der Fossa glenoidalis (p < 0,05). Bei Klasse-III-Malokklusion befand sich der Diskus leicht anterior in Beziehung zum Kondylus (p < 0,05), und der Kondylus war posterior positioniert in der Fossa glenoidalis. Bei allen 3 Formen der Malokklusion waren fast identische Kondylus-Diskus-Position zu beobachten.
Schlussfolgerung
Die Kondylus-Diskus-Position war bei Klasse-I-Malokklusion nahezu regelrecht; bei Klasse-II-Malokklusion dagegen besteht eine höhere Wahrscheinlichkeit für eine Diskusverschiebung nach vorn als bei Klasse-III-Malokklusion.




Similar content being viewed by others
References
Atkinson WB, Bates RE Jr (1983) The effects of the angle of the articular eminence on anterior disk displacement. J Prosthet Dent 49:554–555
Bacetti T, Antonini A, Franchi L, Tonti M, Tollaro I (1997) Glenoid fossa position in different facial types: a cephalometric study. Br J Orthod 24:55–59
Bell WE (1990) Etiology of temporomandibular disorders. In: Temporomandibular disorder, 3rd edn. Yearbook Medico Publisher, Chicago, pp 104–18
Bery DC, Watkinson AC (1978) Mandibular dysfunction and incisor relation. A theoretical explanation for the clicking joint. Br Dent J 144:74–77
Christian H, Hoffmann J, Türp JC (2012) Are temporomandibular disorder symptoms and diag- noses associated with pubertal development in adolescents? An epidemiological study. J Orofac Orthop 73:6–18
Cohlmia JT, Ghosh J, Sinha PK, Nanda RS, Currier GF (1996) Tomographic assessment of temporomandibular joints patients with malocclusion. Angle Orthod 66:27–36
Dibbets JMH, van der Weele LT (1987) Orthodontic treatment in relation to symptoms attributed to dysfunction of the temporomandibular joint. A 10-year report of the University of Groningen study. Am J Orthod Dentofac Orthop 91:193–9
Dibbets JM, van der Weele LT (1991) Flattened condylar projection in children: reflection of seasonal growth? Eur J Orthod 13:161–165
Donlon WC, Moon KL (1987) Comparison of magnetic resonance imaging, arhtrography and clinical and surgical findings in temporomandibular joint internal derangements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 64:2–5
Drace JE, Enzmann DR (1989) Defining the normal temporomandibular joint: closed-, partly open-, and open-mouth MR Imaging of asymptomatic subjects. Radiology 177:67–71
Drace JE, Young SW, Enzmann DR (1990) TMJ meniscus and bilaminar zone: MR imaging of the structure—diagnostic landmarks and pitfalls of interpretation. Radiology 177:73–76
Dubrul EL (1980) The craniomandibular articulation. In: Dubrul EL (ed) Sicher’s oral anatomy, 7th edn. CV Mosby, St Louis, pp 107–16
Egermark I, Magnusson T, Carlsson GE (2003) A 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. Angle Orthod 73:109–115
Farrar WB (1972) Differentiation of temporomandibular joint dysfunction to simplify treatment. J Prosthet Dent 28:629–636
Galhardo AP, da Costa Leite C, Gebrim EM, Gomes RL, Mukai MK, Yamaguchi CA, Bernardo WM, Soares JM Jr, Baracat EC, Gil C (2013) The correlation of research diagnostic criteria for temporomandibular disorders and magnetic resonance imaging: a study of diagnostic accuracy. Oral Surg Oral Med Oral Pathol Oral Radiol 115:277–284
Gelb H, Bemstein I (1983) Clinical evaluation of two hundred patients with TMJ syndrome. J Prosthet Dent 49:234–243
Gökalp H, Türkkahraman H (2000) Changes in position of the temporomandibular joint disc and condyle after disc repositioning appliance therapy: a functional examination and magnetic resonance imaging study. Angle Orthod 70(5):400–408
Gökalp H (2003) Magnetic resonance imaging assessment of positional relationship between the disk and condyle in asymptomatic young adult mandibular prognathism. Angle Orthod 73:550–555
Gökalp H, Kurt G (2005) Magnetic resonance imaging of the condylar growth pattern and disk position after chin cup therapy: a preliminary study. Angle Orthod 75:568–575
Kantomaa T (1989) The relation between mandibular configuration and the shape of the glenoid fossa in the human. Eur J Orthod 11:77–81
Katsavrias EG, Halazonetis DJ (2005) Condyle and fossa shape in Class II and Class III skeletal patterns: a morphometric tomographic study. Am J Orthod Dentofac Orthop 128:337–346
Kim MR, Graber TM, Viana MA (2002) Orthodontics and temporomandibular disorder: a meta-analysis. Am J Orthod Dentofac Orthop 121:438–446
Laurell KA, Tootle R, Cunningham R, Beltran J, Simon D (1987) Magnetic resonance imaging of the temporomandibular joint, II: comparison with laminographic, autopsy, and histologic findings. J Prosthet Dent 58:211–218
Mohlin B, Axelsson S, Paulin G et al (2007) TMD in relation to malocclusion and orthodontic treatment. Angle Orthod 77:524–548
Nickel JC, Yao P, Spalding PM et al (2002) Validated numerical modeling of the effects of combined orthodontic and orthognathic surgical treatment of on TMJ loads and muscle forces. Am J Orthod Dentofac Orthop 121:73–83
Okeson JP (2008) Management of temporomandibular joint disorders and occlusion. Mosby, St Louis
Pullinger AG, Hollender L, Solberg KW et al (1985) A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent 53:706–713
Pullinger AG, Solberg WK, Hollender L et al (1987) Relationship mandibular condylar position to dental occlusion factors in an asymptomatic population. Am J Orthod Dentofac Orthop 91:200–206
Ricketts RM (1955) Abnormal function of the temporomandibular joint. Am J Orthod 41:435–441
Rickets RM (1989) Provocations and perceptions in cranio-facial orthopedics. Dental science and facial art. Rocky Mountain Orthodontics, Denver
Sadowsky C, Polson AM (1984) Temporomandibular disorders and functional occlusion after orthodontic treatment: results of two long-term studies. Am J Orthod 86:386–390
Wisth PJ, Tritrapunt A, Rygh P et al (1987) The effect of maxillary protraction on front occlusion and facial morphology. Acta Odontol Scand 45:227–237
Yatani H, Sonoyama W, Kuboki T et al (1998) The validity of clinical examination for diagnosing anterior disk displacement with reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:647–653
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gökalp, H. Disc position in clinically asymptomatic, pretreatment adolescents with Class I, II, or III malocclusion. J Orofac Orthop 77, 194–202 (2016). https://doi.org/10.1007/s00056-016-0024-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-016-0024-6
Keywords
- Mandibular condyle
- Disc position
- Magnetic resonance imaging
- Orthodontic treatment
- Temporomandibular joint