Abstract
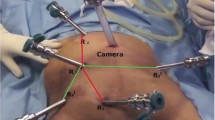
Because of rapid technological progress, precision in rectal cancer therapy has assumed a new dimension. Thus, special attention can be given to the inferior rectal plexus. As a secondary plexus of the inferior hypogastric plexus, its nerve outflow is of great importance for proper pelvic floor function. Our leading question is what the transanal total mesorectal excision (TaTME) perspective could add to the topographical debate about the inferior rectal plexus. After TaTME cadaver training sessions and during TaTME in patients with rectal carcinoma, we can conclude that trained surgeons are capable of accessing the inferior rectal plexus in their operative field.
Zusammenfassung
Aufgrund der rasanten technischen Weiterentwicklung erreicht die Präzision bei der Therapie des Rektumkarzinoms eine neue Dimension. Nicht zuletzt könnte daher dem Plexus rectalis inferior ein besonderes Augenmerk geschenkt werden. Als organorientierter Abschnitt des Plexus hypogastricus inferior haben seine nervalen Vernetzungen besondere Bedeutung für die Funktion des Beckenbodens. Hier wird die Frage erörtert, inwieweit der minimalinvasive transanale Zugang zur totalen mesorektalen Exzision (TaTME) neue Aspekte zur Debatte über die Topographie des Plexus rectalis inferior hervorbringt. Nach ersten anatomischen und klinischen Untersuchungen kann als Fazit festgehalten werden, dass der trainierte Chirurg durch den videoendoskopisch assistierten transanalen Zugang zur totalen mesorektalen Exzision (TME) in der Lage ist, den Plexus rectalis inferior darzustellen.


Similar content being viewed by others
References
Baader B, Herrmann M (2003) Topography of the pelvic autonomic nervous system and its potential impact on surgical intervention in the pelvis. Clin Anat 16:119–130
He JH, Wang Q, Cai QP et al (2010) Quantitative anatomical study of male pelvic autonomic plexus and its clinical potential in rectal resection. Surg Radiol Anat 32:783–790
Stelzner S, Holm T, Moran BJ et al (2011) Deep pelvic anatomy revisted for description of crucial steps in extralevator abdominoperineal excision for rectal cancer. Dis Colon Rectum 54:947–957
Ishiyama G, Hinata N, Kinugasa Y, Murakami G, Fujimiya M (2014) Nerves supplying the internal anal sphincter: an immunohistochemical study using donated elderly cadavers. Surg Radiol Anat 36:1033–1042
Moszkowicz D, Peschaud F, Bessede T, Benoit G, Alsaid B (2012) Internal anal sphincter parasympathetic-nitrergic and sympathetic-adrenergic innervation: a 3-dimensional morphological and functional analysis. Dis Colon Rectum 55:473–481
Goetze O (1951) Chirurgische Beobachtungen zur vegetativen Innervation der Becken-Organe, speziell des After-Schließmuskels. Dtsch Z Nervenheilkd 166:177–188
Stelzner F, Fleischhauer K, Holstein AF (1966) Die Bedeutung des Sphincter internus für die Analkontinenz. Langenbecks Arch Chir 314:132–136
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery – the clue to pelvic recurrence? Br J Surg 69:613–616
Kneist W, Kauff DW, Lang H (2014) Laparoscopic neuromapping in pelvic surgery: scopes of application. Surg Innov 21:213–220
Aigner F, Hörmann R, Fritsch H et al (2015) Anatomical considerations for transanal minimal-invasive surgery: the caudal to cephalic approach. Colorectal Dis 17:O47–53. doi:10.1111/codi.12846
Bertrand MM, Colombo PE, Alsaid B, Prudhomme M, Rouanet P (2014) Transanal endoscopic proctectomy and nerve injury risk: bottom to top surgical anatomy, key points. Dis Colon Rectum 57:1145–1148
Kneist W, Rink AD, Kauff DW, Konerding MA, Lang H (2015) Topography of the extrinsic internal anal sphincter nerve supply during laparoscopic-assisted TAMIS TME: five key zones of risk from the surgeons’ view. Int J Colorectal Dis 30:71–78
Kneist W, Hanke L, Kauff DW, Lang H (2016) Surgeons’ assessment of internal anal sphincter nerve supply during TaTME. Minim Invasive Ther Allied Technol 25:241–246
Atallah S, Albert M, Monson JR (2016) Critical concepts and important anatomic landmarks encountered during transanal total mesorectal excision (taTME): toward the mastery of a new operation for rectal cancer surgery. Tech Coloproctol 20:483–494
McLemore EC, Harnsberger CR, Broderick RC et al (2016) Transanal total mesorectal excision (taTME) for rectal cancer: a training pathway. Surg Endosc 30:4130–4135
Penna M, Hompes R, Mackenzie H, Carter F, Francis NK (2016) First international training and assessment consensus workshop on transanal total mesorectal excision (taTME). Tech Coloproctol 20:343–352
Chand M, Moran B, Wexner S (2016) Which technique to choose in the high-tech era of minimal-access rectal cancer surgery? Colorectal Dis 18:839–841
Chouillard E, Regnier A, Vitte RL et al (2016) Transanal NOTES total mesorectal excision (TME) in patients with rectal cancer: Is anatomy better preserved? Tech Coloproctol 20:537–544
de Lacy AM, Rattner DW, Adelsdorfer C et al (2013) Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to-up” total mesorectal excision (TME) – short-term outcomes in the first 20 cases. Surg Endosc 27:3165–3172
Atallah S, Nassif G, Polavarapu H et al (2013) Robotic-assisted transanal surgery for total mesorectal excision (RATS-TME): a description of a novel surgical approach with video demonstration. Tech Coloproctol 17:441–447
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
W. Kneist, S. Stelzner, L.I. Hanke, and T. Wedel declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Kneist, W., Stelzner, S., Hanke, L.I. et al. Inferior rectal plexus is no longer isolated in no man’s land. coloproctology 39, 85–87 (2017). https://doi.org/10.1007/s00053-016-0134-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00053-016-0134-z
Keywords
- Rectal cancer
- Transanal minimally invasive surgery
- Transanal total mesorectal excision
- Anatomy
- Surgical education
- Autonomic nerves