Abstract
Glutathione (GSH) is an endogenous tripeptide (Glu-Cys-Gly) and the most abundant endogenous antioxidant. It protects the body against oxidative stress and reactive electrophiles. GSH and its oxidized form glutathione disulfide (GSSG) make up the most important thiol redox buffer in the body, and its homeostasis is critical to many important cellular functions. Dysfunction or disruption of the redox buffer has been implicated in various diseases and the implications make GSH, GSSG, and their related systems valid and effective targets for medicinal chemistry interventions. For example, increased levels of GSH and GSH related systems in cancer have been employed as a basis for anticancer prodrug activation, anticancer drug delivery and anticancer drug development. The enriched GSH transporters in the blood brain barrier has been effectively employed for the design of brain targeting prodrugs and brain drug delivery systems. Further, a glutathione conjugate can serve as a marker for the presence of a reactive electrophile providing valid information for the evaluation of a drug candidate. This review focuses on GSH/GSSG system-based biomedical and pharmaceutical applications with relevant basic and comprehensive background information.











Similar content being viewed by others
References
Forman HJ. Glutathione in health and disease. Mol Asp Med. 2009;30:1–110.
Aoyama K, Nakaki T. Impaired glutathione synthesis in neurodegeneration. Int J Mol Sci. 2013;14:21021–44. https://doi.org/10.3390/ijms141021021.
Aoyama K. Glutathione in the brain. Int J Mol Sci. 2021;22. https://doi.org/10.3390/ijms22095010.
Potega A. Glutathione-mediated conjugation of anticancer drugs: an overview of reaction mechanisms and biological significance for drug detoxification and bioactivation. Molecules. 2022;27. https://doi.org/10.3390/molecules27165252.
Kennedy L, Sandhu JK, Harper ME. Cuperlovic-Culf M role of glutathione in cancer: from mechanisms to therapies. Biomolecules. 2020;10. https://doi.org/10.3390/biom10101429.
Wu G, Fang YZ, Yang S, Lupton JR, Turner ND. Glutathione metabolism and its implications for health. J Nutr. 2004;134:489–92. https://doi.org/10.1093/jn/134.3.489.
Gu F, Chauhan V, Chauhan A. Glutathione redox imbalance in brain disorders. Curr Opin Clin Nutr Metab Care. 2015;18:89–95. https://doi.org/10.1097/MCO.0000000000000134.
Holmay MJ, Terpstra M, Coles LD, Mishra U, Ahlskog M, Oz G, et al. N-Acetylcysteine boosts brain and blood glutathione in Gaucher and Parkinson diseases. Clin Neuropharmacol. 2013;36:103–6. https://doi.org/10.1097/WNF.0b013e31829ae713.
Graminski GF, Kubo Y, Armstrong RN. Spectroscopic and kinetic evidence for the thiolate anion of glutathione at the active site of glutathione S-transferase. Biochemistry. 1989;28:3562–8. https://doi.org/10.1021/bi00434a062.
Tew KD, Townsend DM. Glutathione-s-transferases as determinants of cell survival and death. Antioxid Redox Signal. 2012;17:1728–37. https://doi.org/10.1089/ars.2012.4640.
Hermanson GT. The reaction of bioconjugation. In: Hermanson GT, editor. Bioconjugate Techniques 3ed. London ; Waltham, MA: Elsevier/AP; 2013. p. 244–6.
Rooney JP. The role of thiols, dithiols, nutritional factors and interacting ligands in the toxicology of mercury. Toxicology. 2007;234:145–56. https://doi.org/10.1016/j.tox.2007.02.016.
Flora SJ, Shrivastava R, Mittal M. Chemistry and pharmacological properties of some natural and synthetic antioxidants for heavy metal toxicity. Curr Med Chem. 2013;20:4540–74. https://doi.org/10.2174/09298673113209990146.
Cotgreave IA, Moldeus P. Methodologies for the application of monobromobimane to the simultaneous analysis of soluble and protein thiol components of biological systems. J Biochem Biophys Methods. 1986;13:231–49. https://doi.org/10.1016/0165-022x(86)90102-8.
Guan X, Hoffman B, Dwivedi C, Matthees DP. A simultaneous liquid chromatography/mass spectrometric assay of glutathione, cysteine, homocysteine and their disulfides in biological samples. J Pharm Biomed Anal. 2003;31:251–61. https://doi.org/10.1016/s0731-7085(02)00594-0.
Couto N, Wood J, Barber J. The role of glutathione reductase and related enzymes on cellular redox homoeostasis network. Free Radic Biol Med. 2016;95:27–42. https://doi.org/10.1016/j.freeradbiomed.2016.02.028.
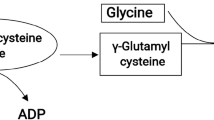
Lu SC. Regulation of glutathione synthesis. Mol Asp Med. 2009;30:42–59. https://doi.org/10.1016/j.mam.2008.05.005.
Lu SC. Glutathione synthesis. Biochim Biophys Acta. 2013;1830:3143–53. https://doi.org/10.1016/j.bbagen.2012.09.008.
Kalinina E, Novichkova M. Glutathione in Protein Redox Modulation through S-Glutathionylation and S-Nitrosylation. Molecules. 2021;26. https://doi.org/10.3390/molecules26020435.
Jefferies H, Coster J, Khalil A, Bot J, McCauley RD, Hall JC. Glutathione. ANZ J Surg. 2003;73:517–22. https://doi.org/10.1046/j.1445-1433.2003.02682.x.
Bachhawat AK, Thakur A, Kaur J, Zulkifli M. Glutathione transporters. Biochim Biophys Acta. 2013;1830:3154–64. https://doi.org/10.1016/j.bbagen.2012.11.018.
Hansen JM, Go YM, Jones DP. Nuclear and mitochondrial compartmentation of oxidative stress and redox signaling. Annu Rev Pharm Toxicol. 2006;46:215–34. https://doi.org/10.1146/annurev.pharmtox.46.120604.141122.
Go YM, Jones DP. Redox compartmentalization in eukaryotic cells. Biochim Biophys Acta. 2008;1780:1273–90. https://doi.org/10.1016/j.bbagen.2008.01.011.
Desideri E, Ciccarone F, Ciriolo MR. Targeting glutathione metabolism: partner in crime in anticancer therapy. Nutrients. 2019;11. https://doi.org/10.3390/nu11081926.
Lv H, Zhen C, Liu J, Yang P, Hu L, Shang P. Unraveling the potential role of glutathione in multiple forms of cell death in cancer therapy. Oxid Med Cell Longev. 2019;2019:3150145 https://doi.org/10.1155/2019/3150145.
Lo M, Ling V, Wang YZ, Gout PW. The xc- cystine/glutamate antiporter: a mediator of pancreatic cancer growth with a role in drug resistance. Br J Cancer. 2008;99:464–72. https://doi.org/10.1038/sj.bjc.6604485.
Bachhawat AK, Kaur A. Glutathione degradation. Antioxid Redox Signal. 2017;27:1200–16. https://doi.org/10.1089/ars.2017.7136.
Hinchman CA, Matsumoto H, Simmons TW, Ballatori N. Intrahepatic conversion of a glutathione conjugate to its mercapturic acid. Metabolism of 1-chloro-2,4-dinitrobenzene in isolated perfused rat and guinea pig livers. J Biol Chem. 1991;266:22179–85.
Hinchman CA, Ballatori N. Glutathione conjugation and conversion to mercapturic acids can occur as an intrahepatic process. J Toxicol Environ Health. 1994;41:387–409. https://doi.org/10.1080/15287399409531852.
Guan X, Dwivedi C, Kim SY, Fine T, Ratzsch A, Seefeldt T, et al. Mercapturic acid biosynthesis of 1-Chloro-2,4-dinitrobenzene in Rat Kidney. Curr Top Toxicol.1:153–60.
Ren X, Zou L, Zhang X, Branco V, Wang J, Carvalho C, et al. Redox signaling mediated by thioredoxin and glutathione systems in the central nervous system. Antioxid Redox Signal 2017;27:989–1010. https://doi.org/10.1089/ars.2016.6925.
Iskusnykh IY, Zakharova AA, Pathak D. Glutathione in brain disorders and aging. Molecules. 2022;27. https://doi.org/10.3390/molecules27010324.
Higashi Y, Aratake T, Shimizu T, Shimizu S, Saito M. Protective role of glutathione in the hippocampus after brain ischemia. Int J Mol Sci. 2021;22. https://doi.org/10.3390/ijms22157765.
Bachhawat AK, Yadav S, Jainarayanan AK, Dubey P. Heart failure and the glutathione cycle: an integrated view. Biochem J. 2020;477:3123–30. https://doi.org/10.1042/BCJ20200429.
Morris G, Anderson G, Dean O, Berk M, Galecki P, Martin-Subero M, et al. The glutathione system: a new drug target in neuroimmune disorders. Mol Neurobiol. 2014;50:1059–84. https://doi.org/10.1007/s12035-014-8705-x.
Fraternale A, Paoletti MF, Casabianca A, Nencioni L, Garaci E, Palamara AT, et al. GSH and analogs in antiviral therapy. Mol Asp Med. 2009;30:99–110. https://doi.org/10.1016/j.mam.2008.09.001.
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis. 2010;37:13–25. https://doi.org/10.1016/j.nbd.2009.07.030.
Estrela JM, Ortega A, Mena S, Sirerol JA, Obrador E. Glutathione in metastases: from mechanisms to clinical applications. Crit Rev Clin Lab Sci. 2016;53:253–67. https://doi.org/10.3109/10408363.2015.1136259.
Goralski T, Ram JL. Extracellular calcium receptor as a target for glutathione and its derivatives. Int J Mol Sci. 2022;23. https://doi.org/10.3390/ijms23020717.
Lim JC, Grey AC, Zahraei A, Donaldson PJ. Age-dependent changes in glutathione metabolism pathways in the lens: New insights into therapeutic strategies to prevent cataract formation-A review. Clin Exp Ophthalmol. 2020;48:1031–42. https://doi.org/10.1111/ceo.13801.
Reynaert NL. Glutathione biochemistry in asthma. Biochim Biophys Acta. 2011;1810:1045–51. https://doi.org/10.1016/j.bbagen.2011.01.010.
Cheng X, Xu HD, Ran HH, Liang G, Wu FG. Glutathione-depleting nanomedicines for synergistic cancer therapy. ACS Nano. 2021;15:8039–68. https://doi.org/10.1021/acsnano.1c00498.
Morales-Borges RH, Gonzalez MJ, Duconge J, Minich DM. N-Acetyl cysteine and glutathione in health and cancer-pharmacogenomics, research, and clinical practice: hypothesis and review. Alter Ther Health Med. 2022;28:169–77.
Chaurasiya A, Gorajiya A, Panchal K, Katke S, Singh AK. A review on multivesicular liposomes for pharmaceutical applications: preparation, characterization, and translational challenges. Drug Deliv Transl Res. 2022;12:1569–87. https://doi.org/10.1007/s13346-021-01060-y.
To K, Cao R, Yegiazaryan A, Owens J, Nguyen T, Sasaninia K, et al. Effects of oral liposomal glutathione in altering the immune responses against mycobacterium tuberculosis and the mycobacterium bovis BCG strain in individuals with Type 2 diabetes. Front Cell Infect Microbiol. 2021;11:657775 https://doi.org/10.3389/fcimb.2021.657775.
Zeevalk GD, Bernard LP, Guilford FT. Liposomal-glutathione provides maintenance of intracellular glutathione and neuroprotection in mesencephalic neuronal cells. Neurochem Res. 2010;35:1575–87. https://doi.org/10.1007/s11064-010-0217-0.
Sinha R, Sinha I, Calcagnotto A, Trushin N, Haley JS, Schell TD, et al. Oral supplementation with liposomal glutathione elevates body stores of glutathione and markers of immune function. Eur J Clin Nutr. 2018;72:105–11. https://doi.org/10.1038/ejcn.2017.132.
Shen H, Wang W. Effect of glutathione liposomes on diabetic nephropathy based on oxidative stress and polyol pathway mechanism. J Liposome Res. 2021;31:317–25. https://doi.org/10.1080/08982104.2020.1780607.
Cacciatore I, Cornacchia C, Pinnen F, Mollica A, Di Stefano A. Prodrug approach for increasing cellular glutathione levels. Molecules. 2010;15:1242–64. https://doi.org/10.3390/molecules15031242.
Pinnen F, Cacciatore I, Cornacchia C, Sozio P, Iannitelli A, Costa M, et al. Synthesis and study of L-dopa-glutathione codrugs as new anti-Parkinson agents with free radical scavenging properties. J Med Chem. 2007;50:2506–15. https://doi.org/10.1021/jm070037v.
Wu JH, Batist G. Glutathione and glutathione analogues; therapeutic potentials. Biochim Biophys Acta. 2013;1830:3350–3. https://doi.org/10.1016/j.bbagen.2012.11.016.
Traverso N, Ricciarelli R, Nitti M, Marengo B, Furfaro AL, Pronzato MA, et al. Role of glutathione in cancer progression and chemoresistance. Oxid Med Cell Longev. 2013;2013:972913 https://doi.org/10.1155/2013/972913.
Burgunder JM, Varriale A, Lauterburg BH. Effect of N-acetylcysteine on plasma cysteine and glutathione following paracetamol administration. Eur J Clin Pharm. 1989;36:127–31. https://doi.org/10.1007/BF00609183.
Haddad M, Herve V, Ben Khedher MR, Rabanel JM, Ramassamy C. Glutathione: an old and small molecule with great functions and new applications in the brain and in Alzheimer’s disease. Antioxid Redox Signal. 2021;35:270–92. https://doi.org/10.1089/ars.2020.8129.
Kinoshita C, Kikuchi-Utsumi K, Aoyama K, Suzuki R, Okamoto Y, Matsumura N, et al. Inhibition of miR-96-5p in the mouse brain increases glutathione levels by altering NOVA1 expression. Commun Biol. 2021;4:182 https://doi.org/10.1038/s42003-021-01706-0.
Yoo D, Jung E, Noh J, Hyun H, Seon S, Hong S, et al. Glutathione-depleting pro-oxidant as a selective anticancer therapeutic agent. ACS Omega. 2019;4:10070–7. https://doi.org/10.1021/acsomega.9b00140.
Xiong Y, Xiao C, Li Z, Yang X. Engineering nanomedicine for glutathione depletion-augmented cancer therapy. Chem Soc Rev. 2021;50:6013–41. https://doi.org/10.1039/d0cs00718h.
Reber U, Wullner U, Trepel M, Baumgart J, Seyfried J, Klockgether T, et al. Potentiation of treosulfan toxicity by the glutathione-depleting agent buthionine sulfoximine in human malignant glioma cells: the role of bcl-2. Biochem Pharm. 1998;55:349–59. https://doi.org/10.1016/s0006-2952(97)00480-2.
Anderson CP, Tsai JM, Meek WE, Liu RM, Tang Y, Forman HJ, et al. Depletion of glutathione by buthionine sulfoxine is cytotoxic for human neuroblastoma cell lines via apoptosis. Exp Cell Res. 1999;246:183–92. https://doi.org/10.1006/excr.1998.4303.
Friesen C, Kiess Y, Debatin KM. A critical role of glutathione in determining apoptosis sensitivity and resistance in leukemia cells. Cell Death Differ. 2004;11:S73–85. https://doi.org/10.1038/sj.cdd.4401431.
D'Alessio M, Cerella C, Amici C, Pesce C, Coppola S, Fanelli C, et al. Glutathione depletion up-regulates Bcl-2 in BSO-resistant cells. FASEB J. 2004;18:1609–11. https://doi.org/10.1096/fj.04-1813fje.
Wondrak GT. Redox-directed cancer therapeutics: molecular mechanisms and opportunities. Antioxid Redox Signal. 2009;11:3013–69. https://doi.org/10.1089/ars.2009.2541.
Asanuma M, Miyazaki I. Glutathione and Related Molecules in Parkinsonism. Int J Mol Sci. 2021;22. https://doi.org/10.3390/ijms22168689.
Wada F, Koga H, Akiba J, Niizeki T, Iwamoto H, Ikezono Y, et al. High expression of CD44v9 and xCT in chemoresistant hepatocellular carcinoma: Potential targets by sulfasalazine. Cancer Sci. 2018;109:2801–10. https://doi.org/10.1111/cas.13728.
Toyoda M, Kaira K, Ohshima Y, Ishioka NS, Shino M, Sakakura K, et al. Prognostic significance of amino-acid transporter expression (LAT1, ASCT2, and xCT) in surgically resected tongue cancer. Br J Cancer 2014;110:2506–13. https://doi.org/10.1038/bjc.2014.178.
Habib E, Linher-Melville K, Lin HX, Singh G. Expression of xCT and activity of system xc(-) are regulated by NRF2 in human breast cancer cells in response to oxidative stress. Redox Biol. 2015;5:33–42. https://doi.org/10.1016/j.redox.2015.03.003.
Sugano K, Maeda K, Ohtani H, Nagahara H, Shibutani M, Hirakawa K. Expression of xCT as a predictor of disease recurrence in patients with colorectal cancer. Anticancer Res. 2015;35:677–82.
Okuno S, Sato H, Kuriyama-Matsumura K, Tamba M, Wang H, Sohda S, et al. Role of cystine transport in intracellular glutathione level and cisplatin resistance in human ovarian cancer cell lines. Br J Cancer. 2003;88:951–6. https://doi.org/10.1038/sj.bjc.6600786.
Roh JL, Kim EH, Jang H, Shin D. Aspirin plus sorafenib potentiates cisplatin cytotoxicity in resistant head and neck cancer cells through xCT inhibition. Free Radic Biol Med. 2017;104:1–9. https://doi.org/10.1016/j.freeradbiomed.2017.01.002.
Ma MZ, Chen G, Wang P, Lu WH, Zhu CF, Song M, et al. Xc- inhibitor sulfasalazine sensitizes colorectal cancer to cisplatin by a GSH-dependent mechanism. Cancer Lett. 2015;368:88–96. https://doi.org/10.1016/j.canlet.2015.07.031.
Sleire L, Skeie BS, Netland IA, Forde HE, Dodoo E, Selheim F, et al. Drug repurposing: sulfasalazine sensitizes gliomas to gamma knife radiosurgery by blocking cystine uptake through system Xc-, leading to glutathione depletion. Oncogene. 2015;34:5951–9. https://doi.org/10.1038/onc.2015.60.
Narang VS, Pauletti GM, Gout PW, Buckley DJ, Buckley AR. Sulfasalazine-induced reduction of glutathione levels in breast cancer cells: enhancement of growth-inhibitory activity of Doxorubicin. Chemotherapy. 2007;53:210–7. https://doi.org/10.1159/000100812.
Circu ML, Stringer S, Rhoads CA, Moyer MP, Aw TY. The role of GSH efflux in staurosporine-induced apoptosis in colonic epithelial cells. Biochem Pharm. 2009;77:76–85. https://doi.org/10.1016/j.bcp.2008.09.011.
Brechbuhl HM, Kachadourian R, Min E, Chan D, Day BJ. Chrysin enhances doxorubicin-induced cytotoxicity in human lung epithelial cancer cell lines: the role of glutathione. Toxicol Appl Pharm. 2012;258:1–9. https://doi.org/10.1016/j.taap.2011.08.004.
Barattin R, Perrotton T, Trompier D, Lorendeau D, Di Pietro A, d'Hardemare Adu M, et al. Iodination of verapamil for a stronger induction of death, through GSH efflux, of cancer cells overexpressing MRP1. Bioorg Med Chem. 2010;18:6265–74. https://doi.org/10.1016/j.bmc.2010.07.031.
Marengo B, Pulliero A, Izzotti A, Domenicotti C. miRNA regulation of glutathione homeostasis in cancer initiation, progression and therapy resistance. Microrna. 2020;9:187–97. https://doi.org/10.2174/2211536609666191218103220.
Seefeldt T, Dwivedi C, Peitz G, Herman J, Carlson L, Zhang Z, et al. 2-Acetylamino-3-[4-(2-acetylamino-2-carboxyethylsulfanylcarbonylamino)- phenylcarbamoylsulfanyl]propionic acid and its derivatives as a novel class of glutathione reductase inhibitors. J Med Chem. 2005;48:5224–31. https://doi.org/10.1021/jm050030i.
Seefeldt T, Zhao Y, Chen W, Raza AS, Carlson L, Herman J, et al. Characterization of a novel dithiocarbamate glutathione reductase inhibitor and its use as a tool to modulate intracellular glutathione. J Biol Chem. 2009;284:2729–37. https://doi.org/10.1074/jbc.M802683200.
Zhao Y, Seefeldt T, Chen W, Carlson L, Stoebner A, Hanson S, et al. Increase in thiol oxidative stress via glutathione reductase inhibition as a novel approach to enhance cancer sensitivity to X-ray irradiation. Free Radic Biol Med. 2009;47:176–83. https://doi.org/10.1016/j.freeradbiomed.2009.04.022.
Sadhu SS, Xie J, Zhang H, Perumal O, Guan X. Glutathione disulfide liposomes - a research tool for the study of glutathione disulfide associated functions and dysfunctions. Biochem Biophys Rep. 2016;7:225–9. https://doi.org/10.1016/j.bbrep.2016.06.017.
Sadhu SS, Wang S, Dachineni R, Averineni RK, Seefeldt T, Xie J, et al. In Vitro and In Vivo antimetastatic effect of glutathione disulfide liposomes. Cancer Growth Metastasis. 2017;10:1179064417695255 https://doi.org/10.1177/1179064417695255.
Sadhu SS, Wang S, Dachineni R, Averineni RK, Yang Y, Yin H, et al. In Vitro and In Vivo tumor growth inhibition by glutathione disulfide liposomes. Cancer Growth Metastasis. 2017;10:1179064417696070 https://doi.org/10.1177/1179064417696070.
Townsend DM, Pazoles CJ, Tew KD. NOV-002, a mimetic of glutathione disulfide. Expert Opin Investig Drugs. 2008;17:1075–83. https://doi.org/10.1517/13543784.17.7.1075.
Di Pietro G, Magno LA, Rios-Santos F. Glutathione S-transferases: an overview in cancer research. Expert Opin Drug Metab Toxicol. 2010;6:153–70. https://doi.org/10.1517/17425250903427980.
Han T, Wu Y, Han W, Yan K, Zhao J, Sun Y. Antitumor effect of organometallic half-sandwich Ru(II)-Arene complexes bearing a glutathione S-Transferase inhibitor. Inorg Chem. 2021;60:13051–61. https://doi.org/10.1021/acs.inorgchem.1c01482.
Ramsay EE, Dilda PJ. Glutathione S-conjugates as prodrugs to target drug-resistant tumors. Front Pharm. 2014;5:181 https://doi.org/10.3389/fphar.2014.00181.
Gunnarsdottir S, Rucki M, Elfarra AA. Novel glutathione-dependent thiopurine prodrugs: evidence for enhanced cytotoxicity in tumor cells and for decreased bone marrow toxicity in mice. J Pharm Exp Ther. 2002;301:77–86. https://doi.org/10.1124/jpet.301.1.77.
Navya PN, Kaphle A, Srinivas SP, Bhargava SK, Rotello VM, Daima HK. Current trends and challenges in cancer management and therapy using designer nanomaterials. Nano Converg. 2019;6:23 https://doi.org/10.1186/s40580-019-0193-2.
Mieszawska AJ, Mulder WJ, Fayad ZA, Cormode DP. Multifunctional gold nanoparticles for diagnosis and therapy of disease. Mol Pharm. 2013;10:831–47. https://doi.org/10.1021/mp3005885.
Giljohann DA, Seferos DS, Daniel WL, Massich MD, Patel PC, Mirkin CA. Gold nanoparticles for biology and medicine. Angew Chem Int Ed Engl. 2010;49:3280–94. https://doi.org/10.1002/anie.200904359.
Ock KS, Ganbold EO, Park J, Cho K, Joo SW, Lee SY. Label-free Raman spectroscopy for accessing intracellular anticancer drug release on gold nanoparticles. Analyst. 2012;137:2852–9. https://doi.org/10.1039/c2an35170f.
Du Y, Xia L, Jo A, Davis RM, Bissel P, Ehrich MF, et al. Synthesis and evaluation of doxorubicin-loaded gold nanoparticles for tumor-targeted drug delivery. Bioconjug Chem. 2018;29:420–30. https://doi.org/10.1021/acs.bioconjchem.7b00756.
Ding Y, Zhou YY, Chen H, Geng DD, Wu DY, Hong J, et al. The performance of thiol-terminated PEG-paclitaxel-conjugated gold nanoparticles. Biomaterials. 2013;34:10217–27. https://doi.org/10.1016/j.biomaterials.2013.09.008.
Gu YJ, Cheng J, Man CW, Wong WT, Cheng SH. Gold-doxorubicin nanoconjugates for overcoming multidrug resistance. Nanomedicine .2012;8:204–11. https://doi.org/10.1016/j.nano.2011.06.005.
Garcia-Garrido E, Cordani M, Somoza A. Modified Gold Nanoparticles to Overcome the Chemoresistance to Gemcitabine in Mutant p53 Cancer Cells. Pharmaceutics. 2021;13. https://doi.org/10.3390/pharmaceutics13122067.
Ghosh PS, Kim CK, Han G, Forbes NS, Rotello VM. Efficient gene delivery vectors by tuning the surface charge density of amino acid-functionalized gold nanoparticles. ACS Nano. 2008;2:2213–8. https://doi.org/10.1021/nn800507t.
Yuan Y, Zhang X, Zeng X, Liu B, Hu F, Zhang G. Glutathione-mediated release of functional miR-122 from gold nanoparticles for targeted induction of apoptosis in cancer treatment. J Nanosci Nanotechnol. 2014;14:5620–7. https://doi.org/10.1166/jnn.2014.8735.
Latorre A, Couleaud P, Aires A, Cortajarena AL, Somoza A. Multifunctionalization of magnetic nanoparticles for controlled drug release: a general approach. Eur J Med Chem. 2014;82:355–62. https://doi.org/10.1016/j.ejmech.2014.05.078.
Chen D, Zhang G, Li R, Guan M, Wang X, Zou T, et al. Biodegradable, hydrogen peroxide, and glutathione dual responsive nanoparticles for potential programmable paclitaxel release. J Am Chem Soc. 2018;140:7373–6. https://doi.org/10.1021/jacs.7b12025.
Chakrapani H, Kalathur RC, Maciag AE, Citro ML, Ji X, Keefer LK, et al. Synthesis, mechanistic studies, and anti-proliferative activity of glutathione/glutathione S-transferase-activated nitric oxide prodrugs. Bioorg Med Chem. 2008;16:9764–71. https://doi.org/10.1016/j.bmc.2008.09.063.
Tew KD. TLK-286: a novel glutathione S-transferase-activated prodrug. Expert Opin Investig Drugs. 2005;14:1047–54. https://doi.org/10.1517/13543784.14.8.1047.
Prezioso JA, Hughey RP, Wang N, Damodaran KM, Bloomer WD. Gamma-glutamyltranspeptidase expression regulates the growth-inhibitory activity of the anti-tumor prodrug gamma-L-glutaminyl-4-hydroxy-3-iodobenzene. Int J Cancer. 1994;56:874–9. https://doi.org/10.1002/ijc.2910560620.
Slivka A, Mytilineou C, Cohen G. Histochemical evaluation of glutathione in brain. Brain Res. 1987;409:275–84. https://doi.org/10.1016/0006-8993(87)90712-8.
Raps SP, Lai JC, Hertz L, Cooper AJ. Glutathione is present in high concentrations in cultured astrocytes but not in cultured neurons. Brain Res. 1989;493:398–401. https://doi.org/10.1016/0006-8993(89)91178-5.
Kannan R, Yi JR, Tang D, Li Y, Zlokovic BV, Kaplowitz N. Evidence for the existence of a sodium-dependent glutathione (GSH) transporter. Expression of bovine brain capillary mRNA and size fractions in Xenopus laevis oocytes and dissociation from gamma-glutamyltranspeptidase and facilitative GSH transporters. J Biol Chem. 1996;271:9754–8. https://doi.org/10.1074/jbc.271.16.9754.
Kannan R, Mittur A, Bao Y, Tsuruo T, Kaplowitz N. GSH transport in immortalized mouse brain endothelial cells: evidence for apical localization of a sodium-dependent GSH transporter. J Neurochem. 1999;73:390–9. https://doi.org/10.1046/j.1471-4159.1999.0730390.x.
Lash LH. Renal glutathione transport: Identification of carriers, physiological functions, and controversies. Biofactors. 2009;35:500–8. https://doi.org/10.1002/biof.65.
Brechbuhl HM, Gould N, Kachadourian R, Riekhof WR, Voelker DR, Day BJ. Glutathione transport is a unique function of the ATP-binding cassette protein ABCG2. J Biol Chem. 2010;285:16582–7. https://doi.org/10.1074/jbc.M109.090506.
More SS, Vince R. Design, synthesis and biological evaluation of glutathione peptidomimetics as components of anti-Parkinson prodrugs. J Med Chem. 2008;51:4581–8. https://doi.org/10.1021/jm800239v.
Englert C, Trutzschler AK, Raasch M, Bus T, Borchers P, Mosig AS, et al. Crossing the blood-brain barrier: glutathione-conjugated poly(ethylene imine) for gene delivery. J Control Release. 2016;241:1–14. https://doi.org/10.1016/j.jconrel.2016.08.039.
Birngruber T, Raml R, Gladdines W, Gatschelhofer C, Gander E, Ghosh A, et al. Enhanced doxorubicin delivery to the brain administered through glutathione PEGylated liposomal doxorubicin (2B3-101) as compared with generic Caelyx,((R))/Doxil((R))–a cerebral open flow microperfusion pilot study. J Pharm Sci. 2014;103:1945–8. https://doi.org/10.1002/jps.23994.
Gaillard PJ, Appeldoorn CC, Rip J, Dorland R, van der Pol SM, Kooij G, et al. Enhanced brain delivery of liposomal methylprednisolone improved therapeutic efficacy in a model of neuroinflammation. J Control Release. 2012;164:364–9. https://doi.org/10.1016/j.jconrel.2012.06.022.
Lindqvist A, Rip J, Gaillard PJ, Bjorkman S, Hammarlund-Udenaes M. Enhanced brain delivery of the opioid peptide DAMGO in glutathione pegylated liposomes: a microdialysis study. Mol Pharm. 2013;10:1533–41. https://doi.org/10.1021/mp300272a.
Gaillard PJ, Appeldoorn CC, Dorland R, van Kregten J, Manca F, Vugts DJ, et al. Pharmacokinetics, brain delivery, and efficacy in brain tumor-bearing mice of glutathione pegylated liposomal doxorubicin (2B3-101). PLoS One. 2014;9:e82331 https://doi.org/10.1371/journal.pone.0082331.
Geldenhuys W, Wehrung D, Groshev A, Hirani A, Sutariya V. Brain-targeted delivery of doxorubicin using glutathione-coated nanoparticles for brain cancers. Pharm Dev Technol. 2015;20:497–506. https://doi.org/10.3109/10837450.2014.892130.
Maussang D, Rip J, van Kregten J, van den Heuvel A, van der Pol S, van der Boom B, et al. Glutathione conjugation dose-dependently increases brain-specific liposomal drug delivery in vitro and in vivo. Drug Discov Today Technol. 2016;20:59–69. https://doi.org/10.1016/j.ddtec.2016.09.003.
Najmi A, Wang S, Huang Y, Seefeldt T, Alqahtani Y, Guan X. 2-(2-Cholesteroxyethoxyl)ethyl 3'-S-glutathionylpropionate and its self-assembled micelles for brain delivery: Design, synthesis and evaluation. Int J Pharm. 2021;600:120520 https://doi.org/10.1016/j.ijpharm.2021.120520.
Najmi AW S, Huang Y, Alqahtani Y, Seefeldt T, Guan X. 2-(2-Cholesteroxyethoxyl)ethyl-3′-S-glutathionylpropionate (COXP) for brain-targeting liposomes. J Drug Deliv Sci Technol. 2022;75:103674 https://doi.org/10.1016/j.jddst.2022.103674.
Baillie TA, Davis MR. Mass spectrometry in the analysis of glutathione conjugates. Biol Mass Spectrom. 1993;22:319–25. https://doi.org/10.1002/bms.1200220602.
Dieckhaus CM, Fernandez-Metzler CL, King R, Krolikowski PH, Baillie TA. Negative ion tandem mass spectrometry for the detection of glutathione conjugates. Chem Res Toxicol. 2005;18:630–8. https://doi.org/10.1021/tx049741u.
Stachulski AV, Baillie TA, Park BK, Obach RS, Dalvie DK, Williams DP, et al. The generation, detection, and effects of reactive drug metabolites. Med Res Rev. 2013;33:985–1080. https://doi.org/10.1002/med.21273.
Wang S, Huang Y, Guan X. Fluorescent Probes for Live Cell Thiol Detection. Molecules. 2021;26. https://doi.org/10.3390/molecules26123575.
Li X, Qian S, He Q, Yang B, Li J, Hu Y. Design and synthesis of a highly selective fluorescent turn-on probe for thiol bioimaging in living cells. Org Biomol Chem. 2010;8:3627–30.
Niu L-Y, Guan Y-S, Chen Y-Z, Wu L-Z, Tung C-H, Yang Q-Z. BODIPY-based ratiometric fluorescent sensor for highly selective detection of glutathione over cysteine and homocysteine. J Am Chem Soc. 2012;134:18928–31. https://doi.org/10.1021/ja309079f.
Tang B, Xing Y, Li P, Zhang N, Yu F, Yang G. A rhodamine-based fluorescent probe containing a Se-N bond for detecting thiols and its application in living cells. J Am Chem Soc. 2007;129:11666–7.
Hedley DWCS. Evaluation of methods for measuring cellular glutathione content using flow cytometry. Cytometry .1994;15:9.
Shiu HY, Chong HC, Leung YC, Wong MK, Che CM. A highly selective FRET‐based fluorescent probe for detection of cysteine and homocysteine. Chem–A Eur J. 2010;16:3308–13.
JungáKim M. A thiol-specific fluorescent probe and its application for bioimaging. Chem Commun. 2010;46:2751–3.
Gu Y, Zhao Z, Niu G, Zhang R, Zhang H, Shan G-G, et al. Ratiometric detection of mitochondrial thiol with a two-photon active AIEgen. ACS Appl Bio Mater. 2019;2:3120–7.
Kim G-J, Lee K, Kwon H, Kim H-J. Ratiometric fluorescence imaging of cellular glutathione. Org Lett. 2011;13:2799–801.
Lin W, Yuan L, Cao Z, Feng Y, Long L. A sensitive and selective fluorescent thiol probe in water based on the conjugate 1, 4‐addition of thiols to α, β‐unsaturated ketones. Chem–A Eur J. 2009;15:5096–103.
Pang L, Zhou Y, Gao W, Zhang J, Song H, Wang X, et al. Curcumin-based fluorescent and colorimetric probe for detecting cysteine in living cells and zebrafish. Ind Eng Chem Res. 2017;56:7650–5.
Ahn YH, Lee JS, Chang YT. Combinatorial rosamine library and application to in vivo glutathione probe. J Am Chem Soc. 2007;129:4510–1. https://doi.org/10.1021/ja068230m.
Lee MH, Han JH, Kwon PS, Bhuniya S, Kim JY, Sessler JL, et al. Hepatocyte-targeting single galactose-appended naphthalimide: a tool for intracellular thiol imaging in vivo. J Am Chem Soc. 2012;134:1316–22. https://doi.org/10.1021/ja210065g.
Tang L, Yu F, Tang B, Yang Z, Fan W, Zhang M, et al. Tumor microenvironment-activated ultrasensitive nanoprobes for specific detection of intratumoral glutathione by ratiometric photoacoustic imaging. ACS Appl Mater interfaces. 2019;11:27558–67.
Lee HY, Choi YP, Kim S, Yoon T, Guo Z, Lee S et al. Selective homocysteine turn-on fluorescent probes and their bioimaging applications. Chem Commun. 2014;50. https://doi.org/10.1039/c4cc00243a.
Li Y, Yang Y, Guan X. Benzofurazan sulfides for thiol imaging and quantification in live cells through fluorescence microscopy. Anal Chem. 2012;84:6877–83. https://doi.org/10.1021/ac301306s.
Wang S, Yin H, Huang Y, Guan X. Thiol specific and mitochondria selective fluorogenic benzofurazan sulfide for live cell nonprotein thiol imaging and quantification in mitochondria. Anal Chem. 2018;90:8170–7. https://doi.org/10.1021/acs.analchem.8b01469.
Alqahtani Y, Wang S, Huang Y, Najmi A, Guan X. Design, synthesis, and characterization of Bis(7-(N-(2-morpholinoethyl)sulfamoyl)benzo[c][1,2,5]oxadiazol-5-yl)sulfane for nonprotein thiol imaging in lysosomes in live cells. Anal Chem. 2019;91:15300–7. https://doi.org/10.1021/acs.analchem.9b04552.
Alqahtani Y, Wang S, Najmi A, Huang Y, Guan X. Thiol-specific fluorogenic agent for live cell non-protein thiol imaging in lysosomes. Anal Bioanal Chem. 2019;411:6463–73. https://doi.org/10.1007/s00216-019-02026-3.
Farber PM, Arscott LD, Williams CH Jr., Becker K, Schirmer RH. Recombinant Plasmodium falciparum glutathione reductase is inhibited by the antimalarial dye methylene blue. FEBS Lett. 1998;422:311–4. https://doi.org/10.1016/s0014-5793(98)00031-3.
Schonleben-Janas A, Kirsch P, Mittl PR, Schirmer RH, Krauth-Siegel RL. Inhibition of human glutathione reductase by 10-arylisoalloxazines: crystalline, kinetic, and electrochemical studies. J Med Chem. 1996;39:1549–54. https://doi.org/10.1021/jm950511+.
Davioud-Charvet E, Delarue S, Biot C, Schwobel B, Boehme CC, Mussigbrodt A, et al. A prodrug form of a Plasmodium falciparum glutathione reductase inhibitor conjugated with a 4-anilinoquinoline. J Med Chem. 2001;44:4268–76. https://doi.org/10.1021/jm010268g.
FitzGerald GB, Bauman C, Hussoin MS, Wick MM. 2,4-Dihydroxybenzylamine: a specific inhibitor of glutathione reductase. Biochem Pharm. 1991;41:185–90. https://doi.org/10.1016/0006-2952(91)90475-k.
Becker K, Gui M, Schirmer RH. Inhibition of human glutathione reductase by S-nitrosoglutathione. Eur J Biochem. 1995;234:472–8. https://doi.org/10.1111/j.1432-1033.1995.472_b.x.
Singh RR, Reindl KM. Glutathione S-Transferases in Cancer. Antioxidants (Basel). 2021;10. https://doi.org/10.3390/antiox10050701.
Kunze T, Heps S. Phosphono analogs of glutathione: inhibition of glutathione transferases, metabolic stability, and uptake by cancer cells. Biochem Pharm. 2000;59:973–81. https://doi.org/10.1016/s0006-2952(99)00401-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guan, X. Glutathione and glutathione disulfide – their biomedical and pharmaceutical applications. Med Chem Res 32, 1972–1994 (2023). https://doi.org/10.1007/s00044-023-03116-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-023-03116-9