Abstract
Objectives
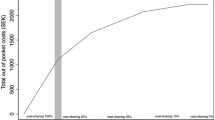
In this article we investigate the causal effect of cost-sharing schemes on compliance with statins in a quantile regression framework.
Methods
We use the health search CSD-LPD data, a longitudinal observational dataset containing computer-based patient records collected by Italian general practitioners. We exploit a series of natural experiments referring to several introductions of co-payment schemes in some of the Italian regions between 2000 and 2009. We adopt an extended difference-in-differences approach to provide quantile estimates of the impact of co-payments on compliance.
Results
We find that (i) introduction of co-payments hurts residents of regions with worse quality and provision of health care; (ii) within these regions, co-payments were particularly harmful for high compliers; (iii) gender, clinical history and geographic residence are important determinants of compliance among poor compliers; (iv) compliance decreases with the potency and dosage of statins, particularly for poor compliers.
Conclusions
In the presence of inefficient health-care provision, co-payments are harmful for drug compliance, and this is especially true for patients who are originally good compliers.


Similar content being viewed by others
References
Atella V, Kopinska J (2012) Criterio di ripartizione e simulazione a medio e lungo termine della spesa sanitaria in italia: una proposta operativa Mimeo
Atella V, Schafheutle E, Noyce P (2005) Affordability of medicines and patients’ cost-reducing behaviour: empirical evidence based on SUR estimates from Italy and the UK. Appl Health Econ Health Policy 4(1):23–35
Atella V, Peracchi F, Depalo D, Rossetti C (2006a) Drug compliance, co-payment and health outcomes: evidence from a panel of Italian patients. Health Econ 15:875–892
Atella V, Rosati FC, Rossi MC (2006) Precautionary saving and health risk. Evidence from the Italian households using a time series of cross sections. Rivista di Politica Economica 96(3):113–132
Avogaro A, Guida P, Giorda C, Mannucci E, Medea G, Comaschi M, Velussi M, Armienti G, Zucchetti R (2007) The under-use of statin in type 2 diabetic patients attending diabetic clinics in Italy. Nutr Metab Cardiovasc 17(1):32–40
Borah B (2011) Assessing predictors of medication adherence in unconditional quantile regression framework. Value Health 14(3):A8
Borah B, Burns M, Shah N (2011) Assessing the impact of high deductible health plans on health-care utilization and cost: a changes-in-changes approach. Health Econ 20:1025–1042
Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, Schwartz JS (2005) Determinants of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 165:1147–1152
Choudhry NK, Patrick AR, Antman EM, Avorn J, Shrank WH (2008) Costeffectiveness of providing full drug coverage to increase medication adherence in post myocardial infarction medicare beneficiaries. Am Heart Assoc Circ 117:1261–1268
Deambrosis P, Seramin C, Terrazzani G, Scaldaferri L, Debetto P, Giusti P, Chinellato A (2007) Evaluation of the prescription and utilization patterns of statins in an Italian local health unit during the period 1994–2003. Eur J Clin Pharmacol 63:197–203
Ellis JJ, Erickson RS, Stevenson JG, Bernstein SJ, Stiles SA, Fendrick AM (2004) Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. Should we target patients with the most to gain? J Gen Intern Med 19:638–645
Ess SM, Schneeweiss S, Szucs TD (2003) European healthcare policies for controlling drug expenditure. Pharmacoeconomics 21(2):89–103
Freemantle N, Bloor K (1996) Lessons from international experience in controlling pharmaceutical expenditure. I: influencing patients. Br Med J 312:1469–1471
Gebregziabher M, Lynch CP, Mueller M, Gilbert GE, Echols C, Zhao Y, Egede LE (2011) Using quantile regression to investigate racial differences in medication non-adherence. BMC Med Res Methodol 11:88
Gibson TB, Mark TL, McGuigan KA, Axelsen K, Shaohung W (2006) The effects of prescription drug co-payments on statin adherence. Am J Manag Care 12:509–517
Hockley T, Gemmill M (2007) European cholesterol guidelines report. Policy analysis centre LSE
Jackevicius CA, Mamdani M, Tu JV (2002) Adherence with statin therapy in elderly patients with and without acute coronary syndrome. Ann Pharmacother 39(11):1792–1797
Jappelli J, Pistaferri L, Weber G (2007) Healthcare quality, economic inequality, and precautionary saving. Health Econ 16(4):327–346
Koenker R (2005) Quantile Regression, Cambridge University Press ISBN 0-521-60827-9
Luepker RV (1993) Patient adherence: a “risk factor” for cardiovascular disease. Heart Dis Stroke 2:418–421
Lundberg L, Johannesson M, Isacson DGL, Borgquist L (1998) Effects of user charges on the use of prescription medicines in different socio-economic groups. Health Policy 44:123–134
Roy S, Madhavan SS (2008) Making a case for employing a societal perspective in the evaluation of medicaid prescription drug interventions. Pharmacoeconomics 26(4):281–296
Sabate E (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
Schultz JS, O’Donnell JC, McDonough KL, Sasane R, Meyer J (2005) Determinants of compliance with statin therapy and low-density lipoprotein cholesterol goal attainment in a managed care population. Am J Manag Care 11:306–312
Shrank WH, Hoang T, Ettner SL, Glassmanand PA, Nair K, DeLapp D, Dirstine J, Avorn J, Asch S (2006) The implications of choice prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med 166:332–337
Yoon J, Ettner S (2009) Cost-sharing and adherence to antihypertensives for low and high adherers. Am J Manag Care 15(11):833–940
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Atella, V., Kopinska, J.A. The impact of cost-sharing schemes on drug compliance in Italy: evidence based on quantile regression. Int J Public Health 59, 329–339 (2014). https://doi.org/10.1007/s00038-013-0528-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-013-0528-4