Abstract
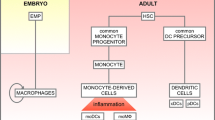
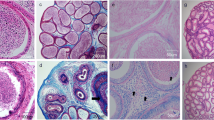
Mononuclear phagocytes (MPs) play an active role in the immunological homeostasis of the urogenital tract. In the epididymis, a finely tuned balance between tolerance to antigenic sperm and immune activation is required to maintain epididymal function while protecting sperm against pathogens and stressors. We previously characterized a subset of resident MPs that express the CX3CR1 receptor, emphasizing their role in antigen sampling and processing during sperm maturation and storage in the murine epididymis. Bacteria-associated epididymitis is the most common cause of intrascrotal inflammation and frequently leads to reproductive complications. Here, we examined whether the lack of functional CX3CR1 in homozygous mice (CX3CR1EGFP/EGFP, KO) alters the ability of MPs to initiate immune responses during epididymitis induced by LPS intravasal–epididymal injection. Confocal microscopy revealed that CX3CR1-deficient MPs located in the initial segments of the epididymis displayed fewer luminal-reaching membrane projections and impaired antigen capture activity. Moreover, flow cytometry showed a reduction of epididymal KO MPs with a monocytic phenotype under physiological conditions. In contrast, flow cytometry revealed an increase in the abundance of MPs with a monocytic signature in the distal epididymal segments after an LPS challenge. This was accompanied by the accumulation of CD103+ cells in the interstitium, and the prevention or attenuation of epithelial damage in the KO epididymis during epididymitis. Additionally, CX3CR1 deletion induced downregulation of Gja1 (connexin 43) expression in KO MPs. Together, our study provides evidence that MPs are gatekeepers of the immunological blood-epididymis barrier and reveal the role of the CX3CR1 receptor in epididymal mucosal homeostasis by inducing MP luminal protrusions and by regulating the monocyte population in the epididymis at steady state as well as upon infection. We also uncover the interaction between MPs and CD103+ dendritic cells, presumably through connexin 43, that enhance immune responses during epididymitis. Our study may lead to new diagnostics and therapies for male infertility and epididymitis by identifying immune mechanisms in the epididymis.








Similar content being viewed by others
Data availability
The datasets generated during this study are available from the corresponding author on reasonable request.
References
Battistone MA, Mendelsohn AC, Spallanzani RG, Brown D, Nair AV, Breton S (2020) Region-specific transcriptomic and functional signatures of mononuclear phagocytes in the epididymis. Mol Hum Reprod 26(1):14–29. https://doi.org/10.1093/molehr/gaz059
Mendelsohn AC, Sanmarco LM, Spallanzani RG, Brown D, Quintana FJ, Breton S et al (2020) From initial segment to cauda: a regional characterization of mouse epididymal CD11c(+) mononuclear phagocytes based on immune phenotype and function. Am J Physiol Cell Physiol 319(6):C997–C1010. https://doi.org/10.1152/ajpcell.00392.2020
Wang M, Yang Y, Cansever D, Wang Y, Kantores C, Messiaen S et al (2021) Two populations of self-maintaining monocyte-independent macrophages exist in adult epididymis and testis. Proc Natl Acad Sci USA 118:1. https://doi.org/10.1073/pnas.2013686117
Da Silva N, Cortez-Retamozo V, Reinecker HC, Wildgruber M, Hill E, Brown D et al (2011) A dense network of dendritic cells populates the murine epididymis. Reproduction 141(5):653–663. https://doi.org/10.1530/REP-10-0493
Da Silva N, Smith TB (2015) Exploring the role of mononuclear phagocytes in the epididymis. Asian J Androl 17(4):591–596. https://doi.org/10.4103/1008-682X.153540
Hume DA (2006) The mononuclear phagocyte system. Curr Opin Immunol 18(1):49–53. https://doi.org/10.1016/j.coi.2005.11.008
Hume DA (2008) Differentiation and heterogeneity in the mononuclear phagocyte system. Mucosal Immunol 1(6):432–441. https://doi.org/10.1038/mi.2008.36
Gordon S, Pluddemann A (2019) The mononuclear phagocytic system generation of diversity. Front Immunol 10:1893. https://doi.org/10.3389/fimmu.2019.01893
Joeris T, Muller-Luda K, Agace WW, Mowat AM (2017) Diversity and functions of intestinal mononuclear phagocytes. Mucosal Immunol 10(4):845–864. https://doi.org/10.1038/mi.2017.22
Jakubzick CV, Randolph GJ, Henson PM (2017) Monocyte differentiation and antigen-presenting functions. Nat Rev Immunol 17(6):349–362. https://doi.org/10.1038/nri.2017.28
Holt PG, Haining S, Nelson DJ, Sedgwick JD (1994) Origin and steady-state turnover of class II MHC-bearing dendritic cells in the epithelium of the conducting airways. J Immunol 153(1):256–61. https://www.ncbi.nlm.nih.gov/pubmed/8207240
Voisin A, Whitfield M, Damon-Soubeyrand C, Goubely C, Henry-Berger J, Saez F et al (2018) Comprehensive overview of murine epididymal mononuclear phagocytes and lymphocytes: unexpected populations arise. J Reprod Immunol 126:11–17. https://doi.org/10.1016/j.jri.2018.01.003
Smith TB, Cortez-Retamozo V, Grigoryeva LS, Hill E, Pittet MJ, Da Silva N (2014) Mononuclear phagocytes rapidly clear apoptotic epithelial cells in the proximal epididymis. Andrology 2(5):755–762. https://doi.org/10.1111/j.2047-2927.2014.00251.x
Battistone MA, Spallanzani RG, Mendelsohn AC, Capen D, Nair AV, Brown D et al (2019) Novel role of proton-secreting epithelial cells in sperm maturation and mucosal immunity. J Cell Sci 133:5. https://doi.org/10.1242/jcs.233239
Silva EJR, Ribeiro CM, Mirim AFM, Silva AAS, Romano RM, Hallak J et al (2018) Lipopolysaccharide and lipotheicoic acid differentially modulate epididymal cytokine and chemokine profiles and sperm parameters in experimental acute epididymitis. Sci Rep 8(1):103. https://doi.org/10.1038/s41598-017-17944-4
Wang F, Liu W, Jiang Q, Gong M, Chen R, Wu H et al (2019) Lipopolysaccharide-induced testicular dysfunction and epididymitis in mice: a critical role of tumor necrosis factor alpha. Biol Reprod 100(3):849–861. https://doi.org/10.1093/biolre/ioy235
McLachlan RI (2002) Basis, diagnosis and treatment of immunological infertility in men. J Reprod Immunol 57(1–2):35–45. https://doi.org/10.1016/s0165-0378(02)00014-1
Meinhardt A, Hedger MP (2011) Immunological, paracrine and endocrine aspects of testicular immune privilege. Mol Cell Endocrinol 335(1):60–68. https://doi.org/10.1016/j.mce.2010.03.022
Busacca M, Fusi F, Brigante C, Doldi N, Smid M, Vigano P (1989) Evaluation of antisperm antibodies in infertile couples with immunobead test: prevalence and prognostic value. Acta Eur Fertil 20(2):77–82. https://www.ncbi.nlm.nih.gov/pubmed/2800931
Ferrer MS, Laflin S, Anderson DE, Miesner MD, Wilkerson MJ, George A et al (2015) Prevalence of bovine sperm-bound antisperm antibodies and their association with semen quality. Theriogenology 84(1):94–100. https://doi.org/10.1016/j.theriogenology.2015.02.017
Pierucci-Alves F, Midura-Kiela MT, Fleming SD, Schultz BD, Kiela PR (2018) Transforming growth factor beta signaling in dendritic cells is required for immunotolerance to sperm in the epididymis. Front Immunol 9:1882. https://doi.org/10.3389/fimmu.2018.01882
Warren BD, Ahn SH, Brittain KS, Nanjappa MK, Wang H, Wang J et al (2021) Multiple lesions contribute to infertility in males lacking autoimmune regulator. Am J Pathol 191(9):1592–1609. https://doi.org/10.1016/j.ajpath.2021.05.021
Fijak M, Pilatz A, Hedger MP, Nicolas N, Bhushan S, Michel V et al (2018) Infectious, inflammatory and “autoimmune” male factor infertility: how do rodent models inform clinical practice? Hum Reprod Update 24(4):416–441. https://doi.org/10.1093/humupd/dmy009
Klein B, Bhushan S, Gunther S, Middendorff R, Loveland KL, Hedger MP et al (2020) Differential tissue-specific damage caused by bacterial epididymo-orchitis in the mouse. Mol Hum Reprod 26(4):215–227. https://doi.org/10.1093/molehr/gaaa011
Pleuger C, Silva EJR, Pilatz A, Bhushan S, Meinhardt A (2020) Differential immune response to infection and acute inflammation along the epididymis. Front Immunol 11:599594. https://doi.org/10.3389/fimmu.2020.599594
Wijayarathna R, Pasalic A, Nicolas N, Biniwale S, Ravinthiran R, Genovese R et al (2020) Region-specific immune responses to autoimmune epididymitis in the murine reproductive tract. Cell Tissue Res 381(2):351–360. https://doi.org/10.1007/s00441-020-03215-8
Michel V, Pilatz A, Hedger MP, Meinhardt A (2015) Epididymitis: revelations at the convergence of clinical and basic sciences. Asian J Androl 17(5):756–763. https://doi.org/10.4103/1008-682X.155770
Rupp TJ, Leslie SW. Epididymitis. StatPearls, https://www.ncbi.nlm.nih.gov/pubmed/28613565. Treasure Island (FL)2022.
Banyra O, Shulyak A (2012) Acute epididymo-orchitis: staging and treatment. Cent Eur J Urol 65(3):139–143. https://doi.org/10.5173/ceju.2012.03.art8
Lai Y, Yu Z, Shi B, Ni L, Liu Y, Yang S (2014) Chronic scrotal pain caused by mild epididymitis: report of a series of 44 cases. Pak J Med Sci. 30(3):638–641. https://doi.org/10.12669/pjms.303.4256
Pilatz A, Hossain H, Kaiser R, Mankertz A, Schuttler CG, Domann E et al (2015) Acute epididymitis revisited: impact of molecular diagnostics on etiology and contemporary guideline recommendations. Eur Urol 68(3):428–435. https://doi.org/10.1016/j.eururo.2014.12.005
Michel V, Duan Y, Stoschek E, Bhushan S, Middendorff R, Young JM et al (2016) Uropathogenic Escherichia coli causes fibrotic remodelling of the epididymis. J Pathol 240(1):15–24. https://doi.org/10.1002/path.4748
Pleuger C, Ai D, Hoppe ML, Winter LT, Bohnert D, Karl D, et al (2022) The regional distribution of resident immune cells shapes distinct immunological environments along the murine epididymis. eLife 11:e82193. https://doi.org/10.7554/eLife.82193
Segel GB, Halterman MW, Lichtman MA (2011) The paradox of the neutrophil’s role in tissue injury. J Leukoc Biol 89(3):359–372. https://doi.org/10.1189/jlb.0910538
Kruger P, Saffarzadeh M, Weber AN, Rieber N, Radsak M, von Bernuth H et al (2015) Neutrophils: between host defence, immune modulation, and tissue injury. PLoS Pathog 11(3):e1004651. https://doi.org/10.1371/journal.ppat.1004651
Breton S, Nair AV, Battistone MA (2019) Epithelial dynamics in the epididymis: role in the maturation, protection, and storage of spermatozoa. Andrology 7(5):631–643. https://doi.org/10.1111/andr.12632
Jung S, Aliberti J, Graemmel P, Sunshine MJ, Kreutzberg GW, Sher A et al (2000) Analysis of fractalkine receptor CX(3)CR1 function by targeted deletion and green fluorescent protein reporter gene insertion. Mol Cell Biol 20(11):4106–4114. https://doi.org/10.1128/MCB.20.11.4106-4114.2000
Battistone MA, Nair AV, Barton CR, Liberman RN, Peralta MA, Capen DE et al (2018) Extracellular adenosine stimulates vacuolar ATPase-dependent proton secretion in medullary intercalated cells. J Am Soc Nephrol 29(2):545–556. https://doi.org/10.1681/ASN.2017060643
Andrade AD, Almeida PGC, Mariani NAP, Freitas GA, Kushima H, Filadelpho AL et al (2021) Lipopolysaccharide-induced epididymitis modifies the transcriptional profile of Wfdc genes in mice. Biol Reprod 104(1):144–158. https://doi.org/10.1093/biolre/ioaa189
Barrachina F, Battistone MA, Castillo J, Mallofre C, Jodar M, Breton S et al (2022) Sperm acquire epididymis-derived proteins through epididymosomes. Hum Reprod 37(4):651–668. https://doi.org/10.1093/humrep/deac015
Brown D, Lydon J, McLaughlin M, Stuart-Tilley A, Tyszkowski R, Alper S (1996) Antigen retrieval in cryostat tissue sections and cultured cells by treatment with sodium dodecyl sulfate (SDS). Histochem Cell Biol 105(4):261–267. https://doi.org/10.1007/BF01463929
Kim B, Breton S (2022) The MAPK/ERK signaling pathway regulates the expression and localization of Cx43 in mouse proximal epididymis. Biol Reprod 106(5):919–927. https://doi.org/10.1093/biolre/ioac034
Pastor-Soler N, Bagnis C, Sabolic I, Tyszkowski R, McKee M, Van Hoek A et al (2001) Aquaporin 9 expression along the male reproductive tract. Biol Reprod 65(2):384–393. https://doi.org/10.1095/biolreprod65.2.384
Paunescu TG, Ljubojevic M, Russo LM, Winter C, McLaughlin MM, Wagner CA et al (2010) cAMP stimulates apical V-ATPase accumulation, microvillar elongation, and proton extrusion in kidney collecting duct A-intercalated cells. Am J Physiol Renal Physiol 298(3):F643–F654. https://doi.org/10.1152/ajprenal.00584.2009
Hulspas R, O’Gorman MR, Wood BL, Gratama JW, Sutherland DR (2009) Considerations for the control of background fluorescence in clinical flow cytometry. Cytometry B Clin Cytom 76(6):355–364. https://doi.org/10.1002/cyto.b.20485
Farache J, Koren I, Milo I, Gurevich I, Kim KW, Zigmond E et al (2013) Luminal bacteria recruit CD103+ dendritic cells into the intestinal epithelium to sample bacterial antigens for presentation. Immunity 38(3):581–595. https://doi.org/10.1016/j.immuni.2013.01.009
Mazzini E, Massimiliano L, Penna G, Rescigno M (2014) Oral tolerance can be established via gap junction transfer of fed antigens from CX3CR1(+) macrophages to CD103(+) dendritic cells. Immunity 40(2):248–261. https://doi.org/10.1016/j.immuni.2013.12.012
Coombes JL, Siddiqui KR, Arancibia-Carcamo CV, Hall J, Sun CM, Belkaid Y et al (2007) A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-beta and retinoic acid-dependent mechanism. J Exp Med 204(8):1757–1764. https://doi.org/10.1084/jem.20070590
Mese G, Richard G, White TW (2007) Gap junctions: basic structure and function. J Invest Dermatol 127(11):2516–2524. https://doi.org/10.1038/sj.jid.5700770
Barbe MT, Monyer H, Bruzzone R (2006) Cell-cell communication beyond connexins: the pannexin channels. Physiology (Bethesda) 21:103–114. https://doi.org/10.1152/physiol.00048.2005
Randolph GJ, Inaba K, Robbiani DF, Steinman RM, Muller WA (1999) Differentiation of phagocytic monocytes into lymph node dendritic cells in vivo. Immunity 11(6):753–761. https://doi.org/10.1016/s1074-7613(00)80149-1
Jakubzick C, Tacke F, Ginhoux F, Wagers AJ, van Rooijen N, Mack M et al (2008) Blood monocyte subsets differentially give rise to CD103+ and CD103- pulmonary dendritic cell populations. J Immunol 180(5):3019–3027. https://doi.org/10.4049/jimmunol.180.5.3019
Varol C, Landsman L, Fogg DK, Greenshtein L, Gildor B, Margalit R et al (2007) Monocytes give rise to mucosal, but not splenic, conventional dendritic cells. J Exp Med 204(1):171–180. https://doi.org/10.1084/jem.20061011
Vermaelen KY, Carro-Muino I, Lambrecht BN, Pauwels RA (2001) Specific migratory dendritic cells rapidly transport antigen from the airways to the thoracic lymph nodes. J Exp Med 193(1):51–60. https://doi.org/10.1084/jem.193.1.51
Bedoui S, Whitney PG, Waithman J, Eidsmo L, Wakim L, Caminschi I et al (2009) Cross-presentation of viral and self antigens by skin-derived CD103+ dendritic cells. Nat Immunol 10(5):488–495. https://doi.org/10.1038/ni.1724
Helft J, Ginhoux F, Bogunovic M, Merad M (2010) Origin and functional heterogeneity of non-lymphoid tissue dendritic cells in mice. Immunol Rev 234(1):55–75. https://doi.org/10.1111/j.0105-2896.2009.00885.x
Chieppa M, Rescigno M, Huang AY, Germain RN (2006) Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J Exp Med 203(13):2841–2852. https://doi.org/10.1084/jem.20061884
Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA et al (2005) CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science 307(5707):254–258. https://doi.org/10.1126/science.1102901
Morita N, Umemoto E, Fujita S, Hayashi A, Kikuta J, Kimura I et al (2019) GPR31-dependent dendrite protrusion of intestinal CX3CR1(+) cells by bacterial metabolites. Nature 566(7742):110–114. https://doi.org/10.1038/s41586-019-0884-1
Reshef R, Kudryavitskaya E, Shani-Narkiss H, Isaacson B, Rimmerman N, Mizrahi A et al (2017) The role of microglia and their CX3CR1 signaling in adult neurogenesis in the olfactory bulb. Elife. https://doi.org/10.7554/eLife.30809
Cardona SM, Kim SV, Church KA, Torres VO, Cleary IA, Mendiola AS et al (2018) Role of the fractalkine receptor in CNS autoimmune inflammation: new approach utilizing a mouse model expressing the human CX3CR1(I249/M280) variant. Front Cell Neurosci 12:365. https://doi.org/10.3389/fncel.2018.00365
Geissmann F, Jung S, Littman DR (2003) Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity 19(1):71–82. https://doi.org/10.1016/s1074-7613(03)00174-2
Browne JA, Yang R, Leir SH, Eggener SE, Harris A (2016) Expression profiles of human epididymis epithelial cells reveal the functional diversity of caput, corpus and cauda regions. Mol Hum Reprod 22(2):69–82. https://doi.org/10.1093/molehr/gav066
Rinaldi VD, Donnard E, Gellatly K, Rasmussen M, Kucukural A, Yukselen O et al (2020) An atlas of cell types in the mouse epididymis and vas deferens. Elife. https://doi.org/10.7554/eLife.55474
Liu P, Yu YR, Spencer JA, Johnson AE, Vallanat CT, Fong AM et al (2008) CX3CR1 deficiency impairs dendritic cell accumulation in arterial intima and reduces atherosclerotic burden. Arterioscler Thromb Vasc Biol 28(2):243–250. https://doi.org/10.1161/ATVBAHA.107.158675
Hulsmans M, Clauss S, Xiao L, Aguirre AD, King KR, Hanley A et al (2017) Macrophages facilitate electrical conduction in the heart. Cell 169(3):510–522. https://doi.org/10.1016/j.cell.2017.03.050
Zhao H, Yu C, He C, Mei C, Liao A, Huang D (2020) The immune characteristics of the epididymis and the immune pathway of the epididymitis caused by different pathogens. Front Immunol 11:2115. https://doi.org/10.3389/fimmu.2020.02115
Mullen TE Jr, Kiessling RL, Kiessling AA (2003) Tissue-specific populations of leukocytes in semen-producing organs of the normal, hemicastrated, and vasectomized mouse. AIDS Res Hum Retroviruses 19(3):235–243. https://doi.org/10.1089/088922203763315740
Denes A, Ferenczi S, Halasz J, Kornyei Z, Kovacs KJ (2008) Role of CX3CR1 (fractalkine receptor) in brain damage and inflammation induced by focal cerebral ischemia in mouse. J Cereb Blood Flow Metab 28(10):1707–1721. https://doi.org/10.1038/jcbfm.2008.64
Soriano SG, Amaravadi LS, Wang YF, Zhou H, Yu GX, Tonra JR et al (2002) Mice deficient in fractalkine are less susceptible to cerebral ischemia-reperfusion injury. J Neuroimmunol 125(1–2):59–65. https://doi.org/10.1016/s0165-5728(02)00033-4
Oh DJ, Dursun B, He Z, Lu L, Hoke TS, Ljubanovic D et al (2008) Fractalkine receptor (CX3CR1) inhibition is protective against ischemic acute renal failure in mice. Am J Physiol Renal Physiol 294(1):F264–F271. https://doi.org/10.1152/ajprenal.00204.2007
Zhou CZ, Wang RF, Cheng DL, Zhu YJ, Cao Q, Lv WF (2019) FLT3/FLT3L-mediated CD103(+) dendritic cells alleviates hepatic ischemia-reperfusion injury in mice via activation of treg cells. Biomed Pharmacother 118:109031. https://doi.org/10.1016/j.biopha.2019.109031
Acknowledgements
The authors thank the Microscopy Core of the Program in Membrane Biology (PMB) (MGH, Boston, MA) and the MGB Molecular Imaging Core (MGH, Charlestown, MA), in particular to Anil V. Nair and Mohammed Sami Saleh Mahamdeh, respectively, for their expertise and support in confocal microscopy. We also thank the HSCI-CRM Flow Cytometry Facility (MGH, Boston, MA), in particular Maris Handley, Daire D. Daly, and Jamie Kauffman for their guidance and assistance in flow cytometry analysis, and Yoshiko Iwamoto (Center for Systems Biology, Department of Radiology, MGH and Harvard Medical School, Boston, MA) for her help in performing the Hematoxylin and Eosin staining. We acknowledge Dr. Claudio Attardo-Parrinello for his assistance in performing one LPS experiment and Dr. Raul German Spallanzani for his assistance in the data interpretation.
Funding
This work was supported by the National Institutes of Health (grant HD104672-01 to M.A.B., grants HD040793, HD069623 to S.B.), the Lalor Foundation (to F.B.), and the IBSA Foundation for Scientific Research (to F.B.) The Microscopy Core facility of the Massachusetts General Hospital (MGH) Program in Membrane Biology receives support from the Boston Area Diabetes and Endocrinology Research Center (DK57521) and the Center for the Study of Inflammatory Bowel Disease (DK43351). The Zeiss LSM 800 microscope was acquired using an NIH Shared Instrumentation Grant S10-OD-021577–01. M.A.B is the recipient of the 2021 MGH Claflin Distinguished Scholar Research Award.
Author information
Authors and Affiliations
Contributions
FB and MAB were involved in the study design and conceptualization. FB, KO, LJT, and MAB performed the experiments and data analysis. FB, RJS, DB, SB, and MAB were involved in data interpretation. FB and MAB wrote the original manuscript. All authors contributed to the writing of the manuscript, made critical comments, and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
All animal procedures were approved by the Massachusetts General Hospital (MGH) Subcommittee on Research Animal Care and were performed following the NIH Guide for the Care and Use of Laboratory Animals (National Academies Press, 2011; protocol 2003N000216).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file11 (MOV 10988 KB)
Supplementary file12 (MOV 33772 KB)
Supplementary file13 (MOV 43248 KB)
Supplementary file14 (MOV 20979 KB)
Supplementary file15 (MOV 12746 KB)
Supplementary file16 (MOV 25481 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barrachina, F., Ottino, K., Tu, L.J. et al. CX3CR1 deficiency leads to impairment of immune surveillance in the epididymis. Cell. Mol. Life Sci. 80, 15 (2023). https://doi.org/10.1007/s00018-022-04664-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-022-04664-w