Abstract
Background
In multiple sclerosis (MS), disturbance of the plasminogen activation system (PAS) and blood brain barrier (BBB) disruption are physiopathological processes that might lead to an abnormal fibrin(ogen) extravasation into the parenchyma. Fibrin(ogen) deposits, usually degraded by the PAS, promote an autoimmune response and subsequent demyelination. However, the PAS disruption is not well understood and not fully characterized in this disorder.
Methods
Here, we characterized the expression of PAS actors during different stages of two mouse models of MS (experimental autoimmune encephalomyelitis—EAE), in the central nervous system (CNS) by quantitative RT-PCR, immunohistofluorescence and fluorescent in situ hybridization (FISH). Thanks to constitutive PAI-1 knockout mice (PAI-1 KO) and an immunotherapy using a blocking PAI-1 antibody, we evaluated the role of PAI-1 in EAE models and its impact on physiopathological processes such as fibrin(ogen) deposits, lymphocyte infiltration and demyelination.
Results
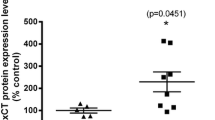
We report a striking overexpression of PAI-1 in reactive astrocytes during symptomatic phases, in two EAE mouse models of MS. This increase is concomitant with lymphocyte infiltration and fibrin(ogen) deposits in CNS parenchyma. By genetic invalidation of PAI-1 in mice and immunotherapy using a blocking PAI-1 antibody, we demonstrate that abolition of PAI-1 reduces the severity of EAE and occurrence of relapses in two EAE models. These benefits are correlated with a decrease in fibrin(ogen) deposits, infiltration of T4 lymphocytes, reactive astrogliosis, demyelination and axonal damage.
Conclusion
These results demonstrate that a deleterious overexpression of PAI-1 by reactive astrocytes leads to intra-parenchymal dysfibrinolysis in MS models and anti-PAI-1 strategies could be a new therapeutic perspective for MS.








Similar content being viewed by others
Availability of data and materials
The datasets of the current study are available from the corresponding author on reasonable request.
Abbreviations
- BBB:
-
Blood brain barrier
- CNS:
-
Central nervous system
- CTCF:
-
Corrected total cell fluorescence
- EAE:
-
Experimental autoimmune encephalomyelitis
- KO:
-
Knockout
- MS:
-
Multiple sclerosis
- NSP:
-
Neuroserpin
- PAI-1:
-
Type-1 plasminogen activator inhibitor
- PAS:
-
Plasminogen activation system
- PLG:
-
Plasminogen
- PN-1:
-
Protease nexin 1
- TAFI:
-
Thrombin-activatable fibrinolysis inhibitor
- tPA:
-
Tissue-type plasminogen
- WT:
-
Wild type
References
Petersen MA, Ryu JK, Akassoglou K (2018) Fibrinogen in neurological diseases: mechanisms, imaging and therapeutics. Nat Rev Neurosci 19(5):283–301
Gveric D, Hanemaaijer R, Newcombe J, van Lent NA, Sier CF, Cuzner ML (2001) Plasminogen activators in multiple sclerosis lesions: implications for the inflammatory response and axonal damage. Brain 124(Pt 10):1978–1988
Gveric D, Herrera B, Petzold A, Lawrence DA, Cuzner ML (2003) Impaired fibrinolysis in multiple sclerosis: a role for tissue plasminogen activator inhibitors. Brain 126(Pt 7):1590–1598
Ryu JK, Petersen MA, Murray SG, Baeten KM, Meyer-Franke A, Chan JP et al (2015) Blood coagulation protein fibrinogen promotes autoimmunity and demyelination via chemokine release and antigen presentation. Nat Commun 6:8164
Docagne F, Nicole O, Marti HH, MacKenzie ET, Buisson A, Vivien D (1999) Transforming growth factor-beta1 as a regulator of the serpins/t-PA axis in cerebral ischemia. FASEB J 13(11):1315–1324
Louessard M, Lacroix A, Martineau M, Mondielli G, Montagne A, Lesept F et al (2016) Tissue plasminogen activator expression is restricted to subsets of excitatory pyramidal glutamatergic neurons. Mol Neurobiol 53(7):5000–5012
Buisson A, Nicole O, Docagne F, Sartelet H, Mackenzie ET, Vivien D (1998) Up-regulation of a serine protease inhibitor in astrocytes mediates the neuroprotective activity of transforming growth factor beta1. FASEB J 12(15):1683–1691
Fernández-Monreal M, López-Atalaya JP, Benchenane K, Léveillé F, Cacquevel M, Plawinski L et al (2004) Is tissue-type plasminogen activator a neuromodulator? Mol Cell Neurosci 25(4):594–601
Cassé F, Bardou I, Danglot L, Briens A, Montagne A, Parcq J et al (2012) Glutamate controls tPA recycling by astrocytes, which in turn influences glutamatergic signals. J Neurosci 32(15):5186–5199
Briens A, Bardou I, Lebas H, Miles LA, Parmer RJ, Vivien D et al (2017) Astrocytes regulate the balance between plasminogen activation and plasmin clearance via cell-surface actin. Cell Discov 3:17001
Mehra A, Ali C, Parcq J, Vivien D, Docagne F (2016) The plasminogen activation system in neuroinflammation. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 1862(3):395–402
East E, Baker D, Pryce G, Lijnen HR, Cuzner ML, Gverić D (2005) A role for the plasminogen activator system in inflammation and neurodegeneration in the central nervous system during experimental allergic encephalomyelitis. Am J Pathol 167(2):545–554
East E, Gverić D, Baker D, Pryce G, Lijnen HR, Cuzner ML (2008) Chronic relapsing experimental allergic encephalomyelitis (CREAE) in plasminogen activator inhibitor-1 knockout mice: the effect of fibrinolysis during neuroinflammation. Neuropathol Appl Neurobiol 34(2):216–230
Davalos D, Ryu JK, Merlini M, Baeten KM, Le Moan N, Petersen MA et al (2012) Fibrinogen-induced perivascular microglial clustering is required for the development of axonal damage in neuroinflammation. Nat Commun 3:1227
Yates RL, Esiri MM, Palace J, Jacobs B, Perera R, DeLuca GC (2017) Fibrin(ogen) and neurodegeneration in the progressive multiple sclerosis cortex: Fibrin(ogen) and Neurodegeneration in MS Cortex. Ann Neurol août 82(2):259–270
Akenami FO, Koskiniemi M, Färkkilä M, Vaheri A (1997) Cerebrospinal fluid plasminogen activator inhibitor-1 in patients with neurological disease. J Clin Pathol 50(2):157–160
Onodera H, Nakashima I, Fujihara K, Nagata T, Itoyama Y (1999) Elevated plasma level of plasminogen activator inhibitor-1 (PAI-1) in patients with relapsing–remitting multiple sclerosis. Tohoku J Exp Med 189(4):259–265
Pérez-Martín MY, González-Platas M, Jiménez-Sosa A, Plata-Bello J, Carrillo-Padilla FJ, Franco-Maside A et al (2017) Can fibrinolytic system components explain cognitive impairment in multiple sclerosis? J Neurol Sci 382:66–72
Lundgaard I, Osório MJ, Kress BT, Sanggaard S, Nedergaard M (2014) White matter astrocytes in health and disease. Neuroscience 276:161–173
Fournier AP, Gauberti M, Quenault A, Vivien D, Macrez R, Docagne F (2019) Reduced spinal cord parenchymal cerebrospinal fluid circulation in experimental autoimmune encephalomyelitis. J Cereb Blood Flow Metab 39(7):1258–1265
Bruckert G, Vivien D, Docagne F, Roussel BD (2016) Normalization of reverse transcription quantitative PCR data during ageing in distinct cerebral structures. Mol Neurobiol 53(3):1540–1550
Watson C, Paxinos G, Kayalioglu G, Heise C (2009) Chapter 16 - Atlas of the Mouse Spinal Cord. In: Watson C, Paxinos G, Kayalioglu G (eds) The Spinal Cord [Internet]. Academic Press, San Diego, pp 308–379
Fournier AP, Quenault A, Martinez de Lizarrondo S, Gauberti M, Defer G, Vivien D et al (2017) Prediction of disease activity in models of multiple sclerosis by molecular magnetic resonance imaging of P-selectin. Proc Natl Acad Sci USA 114(23):6116–6121
Liddelow SA, Barres BA (2017) Reactive astrocytes: production, function, and therapeutic potential. Immunity 46(6):957–967
Van De Craen B, Scroyen I, Abdelnabi R, Brouwers E, Lijnen HR, Declerck PJ et al (2011) Characterization of a panel of monoclonal antibodies toward mouse PAI-1 that exert a significant profibrinolytic effect in vivo. Thromb Res 128(1):68–76
Dietzmann K, Bossanyi Pv, Krause D, Wittig H, Mawrin Ch, Kirches E (2000) Expression of the plasminogen activator system and the inhibitors PAI-1 and PAI-2 in posttraumatic lesions of the CNS and brain injuries following dramatic circulatory arrests: an immunohistochemical study. Pathol Res Practice 196(1):15–21
Liu R-M, van Groen T, Katre A, Cao D, Kadisha I, Ballinger C et al (2011) Knockout of plasminogen activator inhibitor 1 gene reduces amyloid beta peptide burden in a mouse model of Alzheimer’s disease. Neurobiol Aging 32(6):1079–1089
Boche D, Cunningham C, Docagne F, Scott H, Perry VH (2006) TGFβ1 regulates the inflammatory response during chronic neurodegeneration. Neurobiol Dis 22(3):638–650
Kroksveen AC, Opsahl JA, Guldbrandsen A, Myhr K-M, Oveland E, Torkildsen Ø et al (2015) Cerebrospinal fluid proteomics in multiple sclerosis. Biochim Biophys Acta 1854(7):746–756
Emeis JJ, Hoekzema R, de Vos AF (1995) Inhibiting interleukin-1 and tumor necrosis factor-alpha does not reduce induction of plasminogen activator inhibitor type-1 by endotoxin in rats in vivo. Blood 85(1):115–120
Zheng Z, Nakamura K, Gershbaum S, Wang X, Thomas S, Bessler M et al (2020) Interacting hepatic PAI-1/tPA gene regulatory pathways influence impaired fibrinolysis severity in obesity. J Clin Invest 130(8):4348–4359
Lenoir S, Varangot A, Lebouvier L, Galli T, Hommet Y, Vivien D (2019) Post-synaptic release of the neuronal tissue-type plasminogen activator (tPA). Front Cell Neurosci 13:164
Hultman K, Blomstrand F, Nilsson M, Wilhelmsson U, Malmgren K, Pekny M et al (2010) Expression of plasminogen activator inhibitor-1 and protease nexin-1 in human astrocytes: Response to injury-related factors. J Neurosci Res 88(11):2441–2449
Ko HM, Lee SH, Kim KC, Joo SH, Choi WS, Shin CY (2014) The role of TLR4 and Fyn interaction on lipopolysaccharide-stimulated PAI-1 expression in astrocytes. Mol Neurobiol 52(1):8–25
Escartin C, Galea E, Lakatos A, O’Callaghan JP, Petzold GC, Serrano-Pozo A et al (2021) Reactive astrocyte nomenclature, definitions, and future directions. Nat Neurosci 24(3):312–325
Groves A, Kihara Y, Jonnalagadda D, Rivera R, Kennedy G, Mayford M et al (2018) A functionally defined in vivo astrocyte population identified by c-Fos activation in a mouse model of multiple sclerosis modulated by S1P signaling: immediate-early astrocytes (ieAstrocytes). eNeuro 5(5):ENEURO.0239-18.2018
Itoh N, Itoh Y, Tassoni A, Ren E, Kaito M, Ohno A et al (2018) Cell-specific and region-specific transcriptomics in the multiple sclerosis model: focus on astrocytes. Proc Natl Acad Sci USA 115(2):E302–E309
Borggrewe M, Grit C, Vainchtein ID, Brouwer N, Wesseling EM, Laman JD et al (2021) Regionally diverse astrocyte subtypes and their heterogeneous response to EAE. Glia 69(5):1140–1154
Ryu JK, Rafalski VA, Meyer-Franke A, Adams RA, Poda SB, Rios Coronado PE et al (2018) Fibrin-targeting immunotherapy protects against neuroinflammation and neurodegeneration. Nat Immunol 19(11):1212–1223
Baumeier C, Escher F, Aleshcheva G, Pietsch H, Schultheiss H-P (2021) Plasminogen activator inhibitor-1 reduces cardiac fibrosis and promotes M2 macrophage polarization in inflammatory cardiomyopathy. Basic Res Cardiol 116(1):1
Kubala MH, Punj V, Placencio-Hickok VR, Fang H, Fernandez GE, Sposto R et al (2018) Plasminogen activator inhibitor-1 promotes the recruitment and polarization of macrophages in cancer. Cell Rep 25(8):2177-2191.e7
Poggi M, Paulmyer-Lacroix O, Verdier M, Peiretti F, Bastelica D, Boucraut J et al (2007) Chronic plasminogen activator inhibitor-1 (PAI-1) overexpression dampens CD25+ lymphocyte recruitment after lipopolysaccharide endotoxemia in mouse lung. J Thromb Haemost 5(12):2467–2475
Thapa B, Kim YH, Kwon H-J, Kim D-S (2014) The LRP1-independent mechanism of PAI-1-induced migration in CpG-ODN activated macrophages. Int J Biochem Cell Biol 49:17–25
Acknowledgements
This project was supported by grants from the French Ministry of Higher Education, the INSERM (French National Institute for Health and Medical Research), the regional Council of Normandy, the ARSEP foundation and the FRM (Fondation pour la recherche médicale). We thank Dr Paul Declerck for the gift of PAI-1 blocking antibody.
Funding
This project was supported by grants from the French Ministry of Higher Education, the INSERM (French National Institute for Health and Medical Research), the regional Council of Normandy, the ARSEP foundation and the FRM (Fondation pour la recherche médicale).
Author information
Authors and Affiliations
Contributions
HL designed the experiments, performed in vitro and in vivo studies, analyzed data, and participated in manuscript preparation. SG analyzed data and participated in manuscript preparation. AP performed reactive astrogliosis and axonal damage experiments and analyzed data. AF generated P-sel+ and P-sel− tissues. A-CB set up and performed FISH study. DV drafted the manuscript. MC-S gave expertise in the design of FISH study and drafted the article. FD designed the study and wrote the article. IB designed the study, analyzed data and wrote the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
Animal experiments were performed in accordance with French ethical laws (Decree 87/848) and European guidelines (Directive 2010/63/UE) for the care and use of laboratory animals. Experiments were undertaken in the housing and laboratories (approval #F14118001) and have been approved by the ethics committee no. 52 on animal experiments (CENOMEXA) and by the French Ministry of Research under the project license number #10799. All experiments were performed following the ARRIVE guidelines (www.nc3rs.org.uk), including randomization of treatment as well as analysis blind to the treatment.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
18_2022_4340_MOESM1_ESM.pdf
Supplementary file1 Additional file 1: Figure S1. PAS gene expression in forebrain, cerebellum and spinal cord during the course of MOG-induced EAE. Gene expression of a-c tPA, d-f NSP, g-i PN-1, j TAFI, k, l PAI-1 and m-o PLG in a, d, g, j, m the spinal cord, b, e, h, k, n the cerebellum and c, f, i, l, o the forebrain of mice during the course of MOG-induced EAE. RT-qPCR results expressed as mean ± SEM, n=5 per condition. Kruskal-Wallis test followed by FDR post-hoc test: * and § indicate significant difference (p < 0.05) compared to Sham and Pre-On respectively, Δ indicates other significant differences (p < 0.05) between specific stages. tPA: tissue-type plasminogen activator; NSP: Neuroserpin; PN-1: protease nexin-1; PLG: Plasminogen; TAFI: thrombin-activatable fibrinolysis inhibitor; PAI-1: type-1 plasminogen activator inhibitor. Pre-On: pre-onset; On: onset; Su: surge; Ch: chronic as depicted in Fig. 1a. (PDF 235 KB)
18_2022_4340_MOESM2_ESM.pdf
Supplementary file2 Additional file 2: Figure S2.PAS gene expression in forebrain, cerebellum and spinal cord during the course of PLP-induced EAE. Gene expression of a-c tPA, d-f NSP, g-i PN-1, j TAFI, k, l PAI-1 and m, n PLG in a, d, g, j, m the spinal cord, b, e, h, k, n the cerebellum and c, f, i, l the forebrain of mice during the course of PLP-induced EAE. RT-qPCR results expressed as mean ± SEM, n=5 per condition. Kruskal-Wallis test followed by FDR post-hoc test: *, §, #, † indicate significant difference (p < 0.05) compared to Sham, Pre-On, Rem and Rel respectively, Δ indicates other significant differences (p < 0.05) between specific stages. tPA: tissue-type plasminogen activator; NSP: Neuroserpin; PN-1: protease nexin-1; PLG: Plasminogen; TAFI: thrombin-activatable fibrinolysis inhibitor; PAI-1: type-1 plasminogen activator inhibitor. Pre-On: pre-onset; On: onset; Sc1/2/3/4/2R: score 1/2/3/4/2 remitting; Rem: remission; Rel: relapse as depicted in Fig. 1d. (PDF 295 KB)
18_2022_4340_MOESM3_ESM.pdf
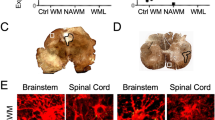
Supplementary file3 Additional file 3: Figure S3: PAI-1 immunostaining quantification in white matter spinal cord sections during the course of MOG-induced EAE model. a Representative PAI-1 immunostaining (red) in cervical, high thoracic, low thoracic and lumbar sections of spinal cord from Sham and MOG-induced EAE mice for each stage of the disease (DAPI: blue). b Quantification of PAI-1 immunostaining coverage in cervical, high thoracic, low thoracic and lumbar sections of spinal cord from Sham and MOG-induced EAE mice. Histograms show mean ± SEM, n=3 per condition. Kruskal-Wallis test followed by FDR post-hoc test: * indicates significant difference (p < 0.05) compared to Sham, Δ indicates other significant differences (p < 0.05) between specific stages. Sc1/2/3/4: score 1/2/3/4. Scale bars: 50µm. (PDF 496 KB)
18_2022_4340_MOESM4_ESM.pdf
Supplementary file4 Additional file 4: Figure S4: PAI-1 immunostaining quantification in white matter spinal cord sections during the course of PLP-induced EAE model. a Representative PAI-1 immunostaining (red) in cervical, high thoracic, low thoracic and lumbar sections of spinal cord from Sham and PLP-induced EAE mice for each stage of the disease (DAPI: blue). b PAI-1 immunostaining coverage in cervical, high thoracic, low thoracic and lumbar sections of spinal cord from Sham and PLP-induced EAE mice. Histograms show mean ± SEM, n=3 per condition. Kruskal-Wallis test followed by FDR post-hoc test: *, §, #, † indicate significant difference (p < 0.05) compared to Sham, Pre-on, Rem and Rel respectively, Δ indicates other significant differences (p < 0.05) between specific stages. Sc1/2/3/4/2R: score1/2/3/4/2 remitting; Rem: remission; Rel: relapse. Scale bars: 50µm. (PDF 672 KB)
18_2022_4340_MOESM5_ESM.pdf
Supplementary file5 Additional file 5: Figure S5: SMI32 immunostaining quantification in white matter spinal cord sections during the course of EAE models. a Representative SMI-32 immunostaining (red) in cervical spinal cord from PAI-1 WT and PAI-1 KO mice at onset (14 dpi), peak (18 dpi) and late stages (45 dpi) during MOG-induced EAE (DAPI: blue). b Corresponding quantifications of axonal damage in cervical spinal cord from PAI-1 WT and PAI-1 KO mice. c Representative SMI32 immunostaining (red) in spinal cord from control and anti-PAI-1 antibody-treated mice at acute (16 dpi), remission (28 dpi) and late stages (45 dpi) during PLP-induced EAE (DAPI: blue). d Corresponding quantifications of axonal damage in spinal cord from control and anti-PAI-1 antibody-treated mice. Histograms show mean ± SEM, n=3 per condition. Mann-Whitney U test; *p < 0.05. Scale bars: 40µm. (PDF 543 KB)
Rights and permissions
About this article
Cite this article
Lebas, H., Guérit, S., Picot, A. et al. PAI-1 production by reactive astrocytes drives tissue dysfibrinolysis in multiple sclerosis models. Cell. Mol. Life Sci. 79, 323 (2022). https://doi.org/10.1007/s00018-022-04340-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-022-04340-z