Abstract
Estrogen is the major female hormone involved in reproductive functions, but it also exerts a variety of additional roles in non-reproductive organs. In this review, we highlight the preclinical and clinical studies that have pointed out sex differences and estrogenic influence on audition. We also describe the experimental evidences supporting a protective role of estrogen towards acquired forms of hearing loss. Although a high level of endogenous estrogen is associated with a better hearing function, hormonal treatments at menopause have provided contradictory outcomes. The various factors that are likely to explain these discrepancies include the treatment regimen as well as the hormonal status and responsiveness of the patients. The complexity of estrogen signaling is being untangled and many downstream effectors of its genomic and non-genomic actions have been identified in other systems. Based on these advances and on the common physio-pathological events that underlie age-related, drug or noise-induced hearing loss, we discuss potential mechanisms for their protective actions in the cochlea.




Similar content being viewed by others
References
Roth TN (2015) Aging of the auditory system. Handb Clin Neurol 129:357–373
Davis A, McMahon CM, Pichora-Fuller KM, Russ S, Lin F, Olusanya BO, Chadha S, Tremblay KL (2016) Aging and hearing health: the life-course approach. Gerontologist 56(Suppl 2):S256–S267
Kim SY, Lim JS, Kong IG, Choi HG (2018) Hearing impairment and the risk of neurodegenerative dementia: a longitudinal follow-up study using a national sample cohort. Sci Rep 8:15266
Lin FR et al (2013) Hearing loss and cognitive decline in older adults. JAMA Intern Med 173:293–299
Gruber CJ, Tschugguel W, Schneeberger C, Huber JC (2002) Production and actions of estrogens. N Engl J Med 346:340–352
Barakat R, Oakley O, Kim H, Jin J, Ko CJ (2016) Extra-gonadal sites of estrogen biosynthesis and function. BMB Rep 49:488–496
Tremere LA, Burrows K, Jeong JK, Pinaud R (2011) Organization of estrogen-associated circuits in the mouse primary auditory cortex. J Exp Neurosci 2011:45–60
Caras ML (2013) Estrogenic modulation of auditory processing: a vertebrate comparison. Front Neuroendocrinol 34:285–299
Maney DL, Pinaud R (2011) Estradiol-dependent modulation of auditory processing and selectivity in songbirds. Front Neuroendocrinol 32:287–302
Remage-Healey L, Saldanha CJ, Schlinger BA (2011) Estradiol synthesis and action at the synapse: evidence for “synaptocrine” signaling. Front Endocrinol (Lausanne) 2:28
Forlano PM, Deitcher DL, Bass AH (2005) Distribution of estrogen receptor alpha mRNA in the brain and inner ear of a vocal fish with comparisons to sites of aromatase expression. J Comp Neurol 483:91–113
Yasar P, Ayaz G, User SD, Gupur G, Muyan M (2017) Molecular mechanism of estrogen-estrogen receptor signaling. Reprod Med Biol 16:4–20
Arnal JF et al (2017) Membrane and nuclear estrogen receptor alpha actions: from tissue specificity to medical implications. Physiol Rev 97:1045–1087
Levin ER, Hammes SR (2016) Nuclear receptors outside the nucleus: extranuclear signalling by steroid receptors. Nat Rev Mol Cell Biol 17:783–797
Motohashi R, Takumida M, Shimizu A, Konomi U, Fujita K, Hirakawa K, Suzuki M, Anniko M (2010) Effects of age and sex on the expression of estrogen receptor alpha and beta in the mouse inner ear. Acta Otolaryngol 130:204–214
Stenberg AE, Wang H, Sahlin L, Hultcrantz M (1999) Mapping of estrogen receptors alpha and beta in the inner ear of mouse and rat. Hear Res 136:29–34
Stenberg AE, Wang H, Sahlin L, Stierna P, Enmark E, Hultcrantz M (2002) Estrogen receptors alpha and beta in the inner ear of the ‘Turner mouse’ and an estrogen receptor beta knockout mouse. Hear Res 166:1–8
Simonoska R, Stenberg AE, Duan M, Yakimchuk K, Fridberger A, Sahlin L, Gustafsson JA, Hultcrantz M (2009) Inner ear pathology and loss of hearing in estrogen receptor-beta deficient mice. J Endocrinol 201:397–406
Meltser I, Tahera Y, Simpson E, Hultcrantz M, Charitidi K, Gustafsson JA, Canlon B (2008) Estrogen receptor beta protects against acoustic trauma in mice. J Clin Invest 118:1563–1570
Andersson S et al (2017) Insufficient antibody validation challenges oestrogen receptor beta research. Nat Commun 8:15840
Nelson AW et al (2017) Comprehensive assessment of estrogen receptor beta antibodies in cancer cell line models and tissue reveals critical limitations in reagent specificity. Mol Cell Endocrinol 440:138–150
Yang L, Xu Y, Zhang Y, Vijayakumar S, Jones SM, Lundberg YYW (2018) Mechanism underlying the effects of estrogen deficiency on otoconia. J Assoc Res Otolaryngol 19:353–362
Scheffer DI, Shen J, Corey DP, Chen ZY (2015) Gene expression by mouse inner ear hair cells during development. J Neurosci 35:6366–6380
Simpson ER (2003) Sources of estrogen and their importance. J Steroid Biochem Mol Biol 86:225–230
Dehan CP, Jerger J (1990) Analysis of gender differences in the auditory brainstem response. Laryngoscope 100:18–24
Jerger J, Hall J (1980) Effects of age and sex on auditory brainstem response. Arch Otolaryngol 106:387–391
Wharton JA, Church GT (1990) Influence of menopause on the auditory brainstem response. Audiology 29:196–201
Bilger RC, Matthies ML, Hammel DR, Demorest ME (1990) Genetic implications of gender differences in the prevalence of spontaneous otoacoustic emissions. J Speech Hear Res 33:418–432
McFadden D, Loehlin JC, Pasanen EG (1996) Additional findings on heritability and prenatal masculinization of cochlear mechanisms: click-evoked otoacoustic emissions. Hear Res 97:102–119
Hoffman HJ, Dobie RA, Losonczy KG, Themann CL, Flamme GA (2017) Declining prevalence of hearing loss in US adults aged 20 to 69 years. JAMA Otolaryngol Head Neck Surg 143:274–285
Jun HJ, Hwang SY, Lee SH, Lee JE, Song JJ, Chae S (2015) The prevalence of hearing loss in South Korea: data from a population-based study. Laryngoscope 125:690–694
Park YH, Shin SH, Byun SW, Kim JY (2016) Age- and gender-related mean hearing threshold in a highly-screened population: the Korean National Health and Nutrition Examination Survey 2010–2012. PLoS One 11:e0150783
Snihur AW, Hampson E (2011) Sex and ear differences in spontaneous and click-evoked otoacoustic emissions in young adults. Brain Cogn 77:40–47
Adriztina I, Adnan A, Adenin I, Haryuna SH, Sarumpaet S (2016) Influence of hormonal changes on audiologic examination in normal ovarian cycle females: an analytic study. Int Arch Otorhinolaryngol 20:294–299
Serra A, Maiolino L, Agnello C, Messina A, Caruso S (2003) Auditory brain stem response throughout the menstrual cycle. Ann Otol Rhinol Laryngol 112:549–553
Upadhayay N, Paudel BH, Singh PN, Bhattarai BK, Agrawal K (2014) Pre- and postovulatory auditory brainstem response in normal women. Indian J Otolaryngol Head Neck Surg 66:133–137
Kim SH, Kang BM, Chae HD, Kim CH (2002) The association between serum estradiol level and hearing sensitivity in postmenopausal women. Obstet Gynecol 99:726–730
Jönsson R, Rosenhall U, Gause-Nilsson I, Steen B (1998) Auditory function in 70- and 75-year-olds of four age cohorts. A cross-sectional and time-lag study of presbyacusis. Scand Audiol 27:81–93
Kim S, Lim EJ, Kim HS, Park JH, Jarng SS, Lee SH (2010) Sex differences in a cross sectional study of age-related hearing loss in Korean. Clin Exp Otorhinolaryngol 3:27–31
Pearson JD, Morrell CH, Gordon-Salant S, Brant LJ, Metter EJ, Klein LL, Fozard JL (1995) Gender differences in a longitudinal study of age-associated hearing loss. J Acoust Soc Am 97:1196–1205
Roth TN, Hanebuth D, Probst R (2011) Prevalence of age-related hearing loss in Europe: a review. Eur Arch Otorhinolaryngol 268:1101–1107
Balogova Z, Popelar J, Chiumenti F, Chumak T, Burianova JS, Rybalko N, Syka J (2017) Age-related differences in hearing function and cochlear morphology between male and female fischer 344 rats. Front Aging Neurosci 9:428
Guimaraes P, Zhu X, Cannon T, Kim S, Frisina RD (2004) Sex differences in distortion product otoacoustic emissions as a function of age in CBA mice. Hear Res 192:83–89
Henry KR (2004) Males lose hearing earlier in mouse models of late-onset age-related hearing loss; females lose hearing earlier in mouse models of early-onset hearing loss. Hear Res 190:141–148
Alves C, Oliveira CS (2014) Hearing loss among patients with Turner’s syndrome: literature review. Braz J Otorhinolaryngol 80:257–263
Bonnard A, Hederstierna C, Bark R, Hultcrantz M (2017) Audiometric features in young adults with Turner syndrome. Int J Audiol 56:650–656
Kubba H, Smyth A, Wong SC, Mason A (2017) Ear health and hearing surveillance in girls and women with Turner’s syndrome: recommendations from the Turner’s Syndrome Support Society. Clin Otolaryngol 42:503–507
Hultcrantz M, Stenberg AE, Fransson A, Canlon B (2000) Characterization of hearing in an X,0 ‘Turner mouse’. Hear Res 143:182–188
Caruso S, Maiolino L, Agnello C, Garozzo A, Di Mari L, Serra A (2003) Effects of patch or gel estrogen therapies on auditory brainstem response in surgically postmenopausal women: a prospective, randomized study. Fertil Steril 79:556–561
Hederstierna C, Hultcrantz M, Collins A, Rosenhall U (2007) Hearing in women at menopause. Prevalence of hearing loss, audiometric configuration and relation to hormone replacement therapy. Acta Otolaryngol 127:149–155
Khaliq F, Tandon OP, Goel N (2003) Auditory evoked responses in postmenopausal women on hormone replacement therapy. Indian J Physiol Pharmacol 47:393–399
Kilicdag EB, Yavuz H, Bagis T, Tarim E, Erkan AN, Kazanci F (2004) Effects of estrogen therapy on hearing in postmenopausal women. Am J Obstet Gynecol 190:77–82
Curhan SG, Eliassen AH, Eavey RD, Wang M, Lin BM, Curhan GC (2017) Menopause and postmenopausal hormone therapy and risk of hearing loss. Menopause 24:1049–1056
Strachan D (1996) Sudden sensorineural deafness and hormone replacement therapy. J Laryngol Otol 110:1148–1150
Ostberg JE, Beckman A, Cadge B, Conway GS (2004) Oestrogen deficiency and growth hormone treatment in childhood are not associated with hearing in adults with turner syndrome. Horm Res 62:182–186
Coleman JR, Campbell D, Cooper WA, Welsh MG, Moyer J (1994) Auditory brainstem responses after ovariectomy and estrogen replacement in rat. Hear Res 80:209–215
Cooper WA, Ross KC, Coleman JR (1999) Estrogen treatment and age effects on auditory brainstem responses in the post-breeding Long-Evans rat. Audiology 38:7–12
Price K, Zhu X, Guimaraes PF, Vasilyeva ON, Frisina RD (2009) Hormone replacement therapy diminishes hearing in peri-menopausal mice. Hear Res 252:29–36
Guimaraes P, Frisina ST, Mapes F, Tadros SF, Frisina DR, Frisina RD (2006) Progestin negatively affects hearing in aged women. Proc Natl Acad Sci USA 103:14246–14249
Mohammed H et al (2015) Progesterone receptor modulates ERalpha action in breast cancer. Nature 523:313–317
Li J, Wang H, Johnson SM, Horner-Glister E, Thompson J, White IN, Al-Azzawi F (2008) Differing transcriptional responses to pulsed or continuous estradiol exposure in human umbilical vein endothelial cells. J Steroid Biochem Mol Biol 111:41–49
Marriott LK, McGann-Gramling KR, Hauss-Wegrzyniak B, Sheldahl LC, Shapiro RA, Dorsa DM, Wenk GL (2007) Brain infusion of lipopolysaccharide increases uterine growth as a function of estrogen replacement regimen: suppression of uterine estrogen receptor-alpha by constant, but not pulsed, estrogen replacement. Endocrinology 148:232–240
Gonzalez L, Witchel SF (2012) The patient with Turner syndrome: puberty and medical management concerns. Fertil Steril 98:780–786
Ing NH, Tornesi MB (1997) Estradiol up-regulates estrogen receptor and progesterone receptor gene expression in specific ovine uterine cells. Biol Reprod 56:1205–1215
Potier M, Elliot SJ, Tack I, Lenz O, Striker GE, Striker LJ, Karl M (2001) Expression and regulation of estrogen receptors in mesangial cells: influence on matrix metalloproteinase-9. J Am Soc Nephrol 12:241–251
Rink TL (2004) The gender gap. Occup Health Saf 73:179–183
Hu X, Wang Y, Lau CC (2016) Effects of noise exposure on the auditory function of ovariectomized rats with estrogen deficiency. J Int Adv Otol 12:261–265
Pillai JA, Siegel JH (2011) Interaction of tamoxifen and noise-induced damage to the cochlea. Hear Res 282:161–166
Petrie WK, Dennis MK, Hu C, Dai D, Arterburn JB, Smith HO, Hathaway HJ, Prossnitz ER (2013) G protein-coupled estrogen receptor-selective ligands modulate endometrial tumor growth. Obstet Gynecol Int 2013:472720
Breglio AM et al (2017) Cisplatin is retained in the cochlea indefinitely following chemotherapy. Nat Commun 8:1654
Olgun Y et al (2016) Analysis of genetic and non genetic risk factors for cisplatin ototoxicity in pediatric patients. Int J Pediatr Otorhinolaryngol 90:64–69
Yancey A, Harris MS, Egbelakin A, Gilbert J, Pisoni DB, Renbarger J (2012) Risk factors for cisplatin-associated ototoxicity in pediatric oncology patients. Pediatr Blood Cancer 59:144–148
Hu XJ, Li FF, Wang Y, Lau CC (2017) Effects of cisplatin on the auditory function of ovariectomized rats with estrogen deficiency. Acta Otolaryngol 137:606–610
Jiang M, Karasawa T, Steyger PS (2017) Aminoglycoside-induced cochleotoxicity: a review. Front Cell Neurosci 11:308
Nakamagoe M, Tabuchi K, Uemaetomari I, Nishimura B, Hara A (2010) Estradiol protects the cochlea against gentamicin ototoxicity through inhibition of the JNK pathway. Hear Res 261:67–74
Pooley AE, Luong M, Hussain A, Nathan BP (2015) Neurite outgrowth promoting effect of 17-beta estradiol is mediated through estrogen receptor alpha in an olfactory epithelium culture. Brain Res 1624:19–27
Milon B et al (2018) The impact of biological sex on the response to noise and otoprotective therapies against acoustic injury in mice. Biol Sex Differ 9:12
Thomas S, Munster PN (2009) Histone deacetylase inhibitor induced modulation of anti-estrogen therapy. Cancer Lett 280:184–191
Wang J, Wang Y, Chen X, Zhang PZ, Shi ZT, Wen LT, Qiu JH, Chen FQ (2015) Histone deacetylase inhibitor sodium butyrate attenuates gentamicin-induced hearing loss in vivo. Am J Otolaryngol 36:242–248
Lauer AM, Schrode KM (2017) Sex bias in basic and preclinical noise-induced hearing loss research. Noise Health 19:207–212
Villavisanis DF, Schrode KM, Lauer AM (2018) Sex bias in basic and preclinical age-related hearing loss research. Biol Sex Differ 9:23
Tremblay AM, Giguere V (2007) The NR3B subgroup: an ovERRview. Nucl Recept Signal 5:e009
Ben Said M et al (2011) A novel missense mutation in the ESRRB gene causes DFNB35 hearing loss in a Tunisian family. Eur J Med Genet 54:e535–e541
Collin RW et al (2008) Mutations of ESRRB encoding estrogen-related receptor beta cause autosomal-recessive nonsyndromic hearing impairment DFNB35. Am J Hum Genet 82:125–138
Bhatt I, Phillips S, Richter S, Tucker D, Lundgren K, Morehouse R, Henrich V (2016) A polymorphism in human estrogen-related receptor beta (ESRRbeta) predicts audiometric temporary threshold shift. Int J Audiol 55:571–579
Nolan LS et al (2013) Estrogen-related receptor gamma and hearing function: evidence of a role in humans and mice. Neurobiol Aging 34(2077):e1–e9
Schilit SL et al (2016) Estrogen-related receptor gamma implicated in a phenotype including hearing loss and mild developmental delay. Eur J Hum Genet 24:1622–1626
Chen J, Nathans J (2007) Estrogen-related receptor beta/NR3B2 controls epithelial cell fate and endolymph production by the stria vascularis. Dev Cell 13:325–337
Buniello A et al (2016) Wbp2 is required for normal glutamatergic synapses in the cochlea and is crucial for hearing. EMBO Mol Med 8:191–207
Stefkovich ML, Arao Y, Hamilton KJ, Korach KS (2018) Experimental models for evaluating non-genomic estrogen signaling. Steroids 133:34–37
Dinh CT, Goncalves S, Bas E, Van De Water TR, Zine A (2015) Molecular regulation of auditory hair cell death and approaches to protect sensory receptor cells and/or stimulate repair following acoustic trauma. Front Cell Neurosci 9:96
Yang CH, Schrepfer T, Schacht J (2015) Age-related hearing impairment and the triad of acquired hearing loss. Front Cell Neurosci 9:276
Fiocchetti M, Ascenzi P, Marino M (2012) Neuroprotective effects of 17beta-estradiol rely on estrogen receptor membrane initiated signals. Front Physiol 3:73
Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M (2017) The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ 8:33
Lagranha CJ, Silva TLA, Silva SCA, Braz GRF, da Silva AI, Fernandes MP, Sellitti DF (2018) Protective effects of estrogen against cardiovascular disease mediated via oxidative stress in the brain. Life Sci 192:190–198
Lean JM, Davies JT, Fuller K, Jagger CJ, Kirstein B, Partington GA, Urry ZL, Chambers TJ (2003) A crucial role for thiol antioxidants in estrogen-deficiency bone loss. J Clin Invest 112:915–923
Lacort M, Leal AM, Liza M, Martin C, Martinez R, Ruiz-Larrea MB (1995) Protective effect of estrogens and catecholestrogens against peroxidative membrane damage in vitro. Lipids 30:141–146
Mukai K, Daifuku K, Yokoyama S, Nakano M (1990) Stopped-flow investigation of antioxidant activity of estrogens in solution. Biochim Biophys Acta 1035:348–352
Rao AK, Dietrich AK, Ziegler YS, Nardulli AM (2011) 17beta-Estradiol-mediated increase in Cu/Zn superoxide dismutase expression in the brain: a mechanism to protect neurons from ischemia. J Steroid Biochem Mol Biol 127:382–389
Zhu X, Tang Z, Cong B, Du J, Wang C, Wang L, Ni X, Lu J (2013) Estrogens increase cystathionine-gamma-lyase expression and decrease inflammation and oxidative stress in the myocardium of ovariectomized rats. Menopause 20:1084–1091
Bellanti F, Matteo M, Rollo T, De Rosario F, Greco P, Vendemiale G, Serviddio G (2013) Sex hormones modulate circulating antioxidant enzymes: impact of estrogen therapy. Redox Biol 1:340–346
Unfer TC, Figueiredo CG, Zanchi MM, Maurer LH, Kemerich DM, Duarte MM, Konopka CK, Emanuelli T (2015) Estrogen plus progestin increase superoxide dismutase and total antioxidant capacity in postmenopausal women. Climacteric 18:379–388
Ada S, Hanci D, Ulusoy S, Vejselova D, Burukoglu D, Muluk NB, Cingi C (2017) Potential protective effect of N-acetyl cysteine in acoustic trauma: an experimental study using scanning electron microscopy. Adv Clin Exp Med 26:893–897
Feldman L, Efrati S, Eviatar E, Abramsohn R, Yarovoy I, Gersch E, Averbukh Z, Weissgarten J (2007) Gentamicin-induced ototoxicity in hemodialysis patients is ameliorated by N-acetylcysteine. Kidney Int 72(3):359–363
Marie A et al (2018) N-acetylcysteine treatment reduces age-related hearing loss and memory impairment in the senescence-accelerated Prone 8 (SAMP8) mouse model. Aging Dis 9(4):664–673
Redza-Dutordoir M, Averill-Bates DA (2016) Activation of apoptosis signalling pathways by reactive oxygen species. Biochim Biophys Acta 1863:2977–2992
Nakamagoe M, Tabuchi K, Nishimura B, Hara A (2011) Effects of neuroactive steroids on cochlear hair cell death induced by gentamicin. Steroids 76:1443–1450
Garcia-Segura LM, Cardona-Gomez P, Naftolin F, Chowen JA (1998) Estradiol upregulates Bcl-2 expression in adult brain neurons. NeuroReport 9:593–597
Pike CJ (1999) Estrogen modulates neuronal Bcl-xL expression and beta-amyloid-induced apoptosis: relevance to Alzheimer’s disease. J Neurochem 72:1552–1563
Perillo B, Sasso A, Abbondanza C, Palumbo G (2000) 17beta-estradiol inhibits apoptosis in MCF-7 cells, inducing bcl-2 expression via two estrogen-responsive elements present in the coding sequence. Mol Cell Biol 20:2890–2901
Yune TY, Park HG, Lee JY, Oh TH (2008) Estrogen-induced Bcl-2 expression after spinal cord injury is mediated through phosphoinositide-3-kinase/Akt-dependent CREB activation. J Neurotrauma 25:1121–1131
Wang L, Andersson S, Warner M, Gustafsson JA (2001) Morphological abnormalities in the brains of estrogen receptor beta knockout mice. Proc Natl Acad Sci USA 98:2792–2796
Liberman MC, Kujawa SG (2017) Cochlear synaptopathy in acquired sensorineural hearing loss: manifestations and mechanisms. Hear Res 349:138–147
Kujawa SG, Liberman MC (2009) Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci 29:14077–14085
Sohrabji F, Miranda RC, Toran-Allerand CD (1995) Identification of a putative estrogen response element in the gene encoding brain-derived neurotrophic factor. Proc Natl Acad Sci USA 92:11110–11114
Wan G, Gómez-Casati ME, Gigliello AR, Liberman MC, Corfas G (2014) Neurotrophin-3 regulates ribbon synapse density in the cochlea and induces synapse regeneration after acoustic trauma. eLife 3:e03564
Zuccotti A et al (2012) Lack of brain-derived neurotrophic factor hampers inner hair cell synapse physiology, but protects against noise-induced hearing loss. J Neurosci 32:8545–8553
Meltser I, Cederroth CR, Basinou V, Savelyev S, Lundkvist GS, Canlon B (2014) TrkB-mediated protection against circadian sensitivity to noise trauma in the murine cochlea. Curr Biol 24:658–663
Oberlander JG, Woolley CS (2016) 17beta-estradiol acutely potentiates glutamatergic synaptic transmission in the hippocampus through distinct mechanisms in males and females. J Neurosci 36:2677–2690
Jain A, Huang GZ, Woolley CS (2019) Latent sex differences in molecular signaling that underlies excitatory synaptic potentiation in the hippocampus. J Neurosci 39:1552–1565
Koss WA, Haertel JM, Philippi SM, Frick KM (2018) Sex differences in the rapid cell signaling mechanisms underlying the memory-enhancing effects of 17beta-estradiol. eNeuro. https://doi.org/10.1523/ENEURO.0267-18.2018
Nilsen J, Chen S, Brinton RD (2002) Dual action of estrogen on glutamate-induced calcium signaling: mechanisms requiring interaction between estrogen receptors and src/mitogen activated protein kinase pathway. Brain Res 930:216–234
Zhao L, Wu TW, Brinton RD (2004) Estrogen receptor subtypes alpha and beta contribute to neuroprotection and increased Bcl-2 expression in primary hippocampal neurons. Brain Res 1010:22–34
Guidolin D, Tortorella C, Marcoli M, Maura G, Agnati LF (2016) Neuroglobin, a factor playing for nerve cell survival. Int J Mol Sci 17(11):1817–1832
De Marinis E, Fiocchetti M, Acconcia F, Ascenzi P, Marino M (2013) Neuroglobin upregulation induced by 17beta-estradiol sequesters cytocrome c in the mitochondria preventing H2O2-induced apoptosis of neuroblastoma cells. Cell Death Dis 4:e508
Reuss S et al (2016) Neuroglobin expression in the mammalian auditory system. Mol Neurobiol 53:1461–1477
Vorasubin N, Hosokawa S, Hosokawa K, Ishiyama G, Ishiyama A, Lopez IA (2016) Neuroglobin immunoreactivity in the human cochlea. Brain Res 1630:56–63
Hequembourg S, Liberman MC (2001) Spiral ligament pathology: a major aspect of age-related cochlear degeneration in C57BL/6 mice. J Assoc Res Otolaryngol 2:118–129
Kow LM, Pfaff DW (2016) Rapid estrogen actions on ion channels: a survey in search for mechanisms. Steroids 111:46–53
Saint-Criq V, Rapetti-Mauss R, Yusef YR, Harvey BJ (2012) Estrogen regulation of epithelial ion transport: implications in health and disease. Steroids 77:918–923
Chang Q, Wang J, Li Q, Kim Y, Zhou B, Wang Y, Li H, Lin X (2015) Virally mediated Kcnq1 gene replacement therapy in the immature scala media restores hearing in a mouse model of human Jervell and Lange-Nielsen deafness syndrome. EMBO Mol Med 7:1077–1086
Wangemann P et al (2004) Loss of KCNJ10 protein expression abolishes endocochlear potential and causes deafness in Pendred syndrome mouse model. BMC Med 2:30
Lee JH, Marcus DC (2001) Estrogen acutely inhibits ion transport by isolated stria vascularis. Hear Res 158:123–130
Shi X (2011) Physiopathology of the cochlear microcirculation. Hear Res 282:10–24
Guo X, Razandi M, Pedram A, Kassab G, Levin ER (2005) Estrogen induces vascular wall dilation: mediation through kinase signaling to nitric oxide and estrogen receptors alpha and beta. J Biol Chem 280:19704–19710
Yamane H, Takayama M, Konishi K, Iguchi H, Shibata S, Sunami K, Nakai Y (1997) Nitric oxide synthase and contractile protein in the rat cochlear lateral wall: possible role of nitric oxide in regulation of strial blood flow. Hear Res 108:65–73
Brechtelsbauer PB, Nuttall AL, Miller JM (1994) Basal nitric oxide production in regulation of cochlear blood flow. Hear Res 77:38–42
Fujioka M, Okano H, Ogawa K (2014) Inflammatory and immune responses in the cochlea: potential therapeutic targets for sensorineural hearing loss. Front Pharmacol 5:287
Thakkar R, Wang R, Sareddy G, Wang J, Thiruvaiyaru D, Vadlamudi R, Zhang Q, Brann D (2016) NLRP3 inflammasome activation in the brain after global cerebral ischemia and regulation by 17beta-estradiol. Oxid Med Cell Longev 2016:8309031
Xu Y, Sheng H, Bao Q, Wang Y, Lu J, Ni X (2016) NLRP3 inflammasome activation mediates estrogen deficiency-induced depression- and anxiety-like behavior and hippocampal inflammation in mice. Brain Behav Immun 56:175–186
Tschopp J, Schroder K (2010) NLRP3 inflammasome activation: the convergence of multiple signalling pathways on ROS production? Nat Rev Immunol 10:210–215
Shi X et al (2017) NLRP3-inflammasomes are triggered by age-related hearing loss in the inner ear of mice. Am J Transl Res 9:5611–5618
Nakanishi H et al (2017) NLRP3 mutation and cochlear autoinflammation cause syndromic and nonsyndromic hearing loss DFNA34 responsive to anakinra therapy. Proc Natl Acad Sci USA 114:E7766–E7775
Vambutas A, Lesser M, Mullooly V, Pathak S, Zahtz G, Rosen L, Goldofsky E (2014) Early efficacy trial of anakinra in corticosteroid-resistant autoimmune inner ear disease. J Clin Invest 124:4115–4122
Paciello F, Fetoni AR, Rolesi R, Wright MB, Grassi C, Troiani D, Paludetti G (2018) Pioglitazone represents an effective therapeutic target in preventing oxidative/inflammatory cochlear damage induced by noise exposure. Front Pharmacol 9:1103
Acknowledgements
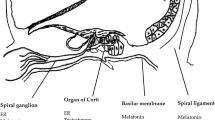
We thank Bernard Minguet for the illustrations of this manuscript. This work was supported by grants from the Belgian National Funds for Scientific Research (FSR-FNRS), the fondation Léon-Frédéricq (ULiège, Belgium) and the Fonds spéciaux (University of Liège, Belgium).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Delhez, A., Lefebvre, P., Péqueux, C. et al. Auditory function and dysfunction: estrogen makes a difference. Cell. Mol. Life Sci. 77, 619–635 (2020). https://doi.org/10.1007/s00018-019-03295-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-019-03295-y