Abstract
Objective
Asthma is an airway inflammatory disease caused by activation of numerous immune cells including macrophages. Bakuchicin (BKC) is known to exhibit anti-inflammatory effects and type 2 T helper (Th2) regulation, but has not been investigated for airway inflammation. This study aimed to evaluate the effects of BKC on airway inflammation and demonstrate the mechanisms of macrophage polarization.
Methods
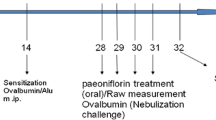
The anti-inflammatory effects were determined using lipopolysaccharide (LPS)-stimulated macrophages. The ovalbumin (OVA)-induced asthma mouse model was used to evaluate the effects of BKC on airway inflammation and Th2 responses. Moreover, the effect of BKC on macrophage polarization was confirmed in bone marrow-derived macrophages (BMDMs) differentiation.
Results
BKC suppressed nitric oxide production and expression of pro-inflammatory cytokines by inhibiting signaling pathway in LPS-stimulated macrophages. In an OVA-induced asthma model, BKC treatment alleviated histological changes and mast cell infiltration and reduced the levels of eosinophil peroxidase, β-hexosaminidase, and immunoglobulin levels. In addition, BKC alleviated Th2 responses and M2 macrophage populations in bronchoalveolar fluid. In BMDMs, BKC suppressed IL-4-induced M2 macrophage polarization and the expression of M2 markers such as arginase-1 and Fizz-1 through inhibiting sirtuin 2 levels.
Conclusion
BKC could be a drug candidate for the treatment of allergic asthma.







Similar content being viewed by others
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Draijer C, Peters-Golden M. Alveolar macrophages in allergic asthma: the forgotten cell awakes. Curr Allergy Asthma Rep. 2017;17:12. https://doi.org/10.1007/s11882-017-0681-6.
Akira S, Misawa T, Satoh T, Saitoh T. Macrophages control innate inflammation. Diab Obes Metab. 2013;15(Suppl 3):10–8. https://doi.org/10.1111/dom.12151.
Saradna A, Do DC, Kumar S, Fu QL, Gao P. Macrophage polarization and allergic asthma. Transl Res. 2018;191:1–14. https://doi.org/10.1016/j.trsl.2017.09.002.
Nie Y, Wang Z, Chai G, Xiong Y, Li B, Zhang H, et al. Dehydrocostus lactone suppresses LPS-induced acute lung injury and macrophage activation through NF-kappaB signaling pathway mediated by p38 MAPK and Akt. Molecules. 2019. https://doi.org/10.3390/molecules24081510.
Feng H, Yin Y, Zheng R, Kang J. Rosiglitazone ameliorated airway inflammation induced by cigarette smoke via inhibiting the M1 macrophage polarization by activating PPARgamma and RXRalpha. Int Immunopharmacol. 2021;97: 107809. https://doi.org/10.1016/j.intimp.2021.107809.
Shi Q, Zhao L, Xu C, Zhang L, Zhao H. High molecular weight hyaluronan suppresses macrophage M1 polarization and enhances IL-10 production in PM2.5-induced lung inflammation. Molecules. 2019. https://doi.org/10.3390/molecules24091766.
Byrne AJ, Mathie SA, Gregory LG, Lloyd CM. Pulmonary macrophages: key players in the innate defence of the airways. Thorax. 2015;70:1189–96. https://doi.org/10.1136/thoraxjnl-2015-207020.
Iwasaki N, Matsushita K, Fukuoka A, Nakahira M, Matsumoto M, Akasaki S, et al. Allergen endotoxins induce T-cell-dependent and non-IgE-mediated nasal hypersensitivity in mice. J Allergy Clin Immunol. 2017;139(258–68): e10. https://doi.org/10.1016/j.jaci.2016.03.023.
Girodet PO, Nguyen D, Mancini JD, Hundal M, Zhou X, Israel E, et al. Alternative macrophage activation is increased in asthma. Am J Respir Cell Mol Biol. 2016;55:467–75. https://doi.org/10.1165/rcmb.2015-0295OC.
Lee YG, Reader BF, Herman D, Streicher A, Englert JA, Ziegler M, et al. Sirtuin 2 enhances allergic asthmatic inflammation. JCI Insight. 2019. https://doi.org/10.1172/jci.insight.124710.
Gomes P, Fleming Outeiro T, Cavadas C. Emerging role of sirtuin 2 in the regulation of mammalian metabolism. Trends Pharmacol Sci. 2015;36:756–68. https://doi.org/10.1016/j.tips.2015.08.001.
Watroba M, Dudek I, Skoda M, Stangret A, Rzodkiewicz P, Szukiewicz D. Sirtuins, epigenetics and longevity. Ageing Res Rev. 2017;40:11–9. https://doi.org/10.1016/j.arr.2017.08.001.
Buechler N, Wang X, Yoza BK, McCall CE, Vachharajani V. Sirtuin 2 regulates microvascular inflammation during sepsis. J Immunol Res. 2017;2017:2648946. https://doi.org/10.1155/2017/2648946.
Lo Sasso G, Menzies KJ, Mottis A, Piersigilli A, Perino A, Yamamoto H, et al. SIRT2 deficiency modulates macrophage polarization and susceptibility to experimental colitis. PLoS One. 2014;9: e103573. https://doi.org/10.1371/journal.pone.0103573.
Lee AS, Jung YJ, Kim D, Nguyen-Thanh T, Kang KP, Lee S, et al. SIRT2 ameliorates lipopolysaccharide-induced inflammation in macrophages. Biochem Biophys Res Commun. 2014;450:1363–9. https://doi.org/10.1016/j.bbrc.2014.06.135.
Wang B, Zhang Y, Cao W, Wei X, Chen J, Ying W. SIRT2 plays significant roles in lipopolysaccharides-induced neuroinflammation and brain injury in mice. Neurochem Res. 2016;41:2490–500. https://doi.org/10.1007/s11064-016-1981-2.
Sun NJ, Woo SH, Cassady JM, Snapka RM. DNA polymerase and topoisomerase II inhibitors from Psoralea corylifolia. J Nat Prod. 1998;61:362–6. https://doi.org/10.1021/np970488q.
Khatune NA, Islam ME, Haque ME, Khondkar P, Rahman MM. Antibacterial compounds from the seeds of Psoralea corylifolia. Fitoterapia. 2004;75:228–30. https://doi.org/10.1016/j.fitote.2003.12.018.
Lim JS, Kim JY, Lee S, Choi JK, Kim EN, Choi YA, et al. Bakuchicin attenuates atopic skin inflammation. Biomed Pharmacother. 2020;129: 110466. https://doi.org/10.1016/j.biopha.2020.110466.
Oishi S, Takano R, Tamura S, Tani S, Iwaizumi M, Hamaya Y, et al. M2 polarization of murine peritoneal macrophages induces regulatory cytokine production and suppresses T-cell proliferation. Immunology. 2016;149:320–8. https://doi.org/10.1111/imm.12647.
Kim YY, Lee S, Kim MJ, Kang BC, Dhakal H, Choi YA, et al. Tyrosol attenuates lipopolysaccharide-induced acute lung injury by inhibiting the inflammatory response and maintaining the alveolar capillary barrier. Food Chem Toxicol. 2017;109:526–33. https://doi.org/10.1016/j.fct.2017.09.053.
Kim YY, Hur G, Lee SW, Lee SJ, Lee S, Kim SH, et al. AGK2 ameliorates mast cell-mediated allergic airway inflammation and fibrosis by inhibiting FcepsilonRI/TGF-beta signaling pathway. Pharmacol Res. 2020;159: 105027. https://doi.org/10.1016/j.phrs.2020.105027.
Borregaard N, Sorensen OE, Theilgaard-Monch K. Neutrophil granules: a library of innate immunity proteins. Trends Immunol. 2007;28:340–5. https://doi.org/10.1016/j.it.2007.06.002.
Acharya KR, Ackerman SJ. Eosinophil granule proteins: form and function. J Biol Chem. 2014;289:17406–15. https://doi.org/10.1074/jbc.R113.546218.
Cruse G, Bradding P. Mast cells in airway diseases and interstitial lung disease. Eur J Pharmacol. 2016;778:125–38. https://doi.org/10.1016/j.ejphar.2015.04.046.
Platts-Mills TA. The role of immunoglobulin E in allergy and asthma. Am J Respir Crit Care Med. 2001;164:S1-5. https://doi.org/10.1164/ajrccm.164.supplement_1.2103024.
Firacative C, Gressler AE, Schubert K, Schulze B, Muller U, Brombacher F, et al. Identification of T helper (Th)1- and Th2-associated antigens of Cryptococcus neoformans in a murine model of pulmonary infection. Sci Rep. 2018;8:2681. https://doi.org/10.1038/s41598-018-21039-z.
Zhu X, Cui J, Yi QJ, Tulake W, Teng F, et al. The role of T cells and macrophages in asthma pathogenesis: a new perspective on mutual crosstalk. Mediators Inflamm. 2020;2020:7835284. https://doi.org/10.1155/2020/7835284.
Joshi N, Walter JM, Misharin AV. Alveolar macrophages. Cell Immunol. 2018;330:86–90. https://doi.org/10.1016/j.cellimm.2018.01.005.
van der Veen TA, de Groot LES, Melgert BN. The different faces of the macrophage in asthma. Curr Opin Pulm Med. 2020;26:62–8. https://doi.org/10.1097/MCP.0000000000000647.
Draijer C, Robbe P, Boorsma CE, Hylkema MN, Melgert BN. Dual role of YM1+ M2 macrophages in allergic lung inflammation. Sci Rep. 2018;8:5105. https://doi.org/10.1038/s41598-018-23269-7.
Chen X, Xiao Z, Jiang Z, Jiang Y, Li W, Wang M. Schisandrin B attenuates airway inflammation and airway remodeling in asthma by inhibiting NLRP3 inflammasome activation and reducing pyroptosis. Inflammation. 2021;44:2217–31. https://doi.org/10.1007/s10753-021-01494-z.
Wang Q, Hong L, Chen M, Shi J, Lin X, Huang L, et al. Targeting M2 macrophages alleviates airway inflammation and remodeling in asthmatic mice via miR-378a-3p/GRB2 pathway. Front Mol Biosci. 2021;8: 717969. https://doi.org/10.3389/fmolb.2021.717969.
Maruthamuthu V, Henry LJK, Ramar MK, Kandasamy R. Myxopyrum serratulum ameliorates airway inflammation in LPS-stimulated RAW 264.7 macrophages and OVA-induced murine model of allergic asthma. J Ethnopharmacol. 2020;255:112369. https://doi.org/10.1016/j.jep.2019.112369.
Al-Alawi M, Hassan T, Chotirmall SH. Transforming growth factor beta and severe asthma: a perfect storm. Respir Med. 2014;108:1409–23. https://doi.org/10.1016/j.rmed.2014.08.008.
Haddad A, Gaudet M, Plesa M, Allakhverdi Z, Mogas AK, Audusseau S, et al. Neutrophils from severe asthmatic patients induce epithelial to mesenchymal transition in healthy bronchial epithelial cells. Respir Res. 2019;20:234. https://doi.org/10.1186/s12931-019-1186-8.
Chan BCL, Lam CWK, Tam LS, Wong CK. IL33: roles in allergic inflammation and therapeutic perspectives. Front Immunol. 2019;10:364. https://doi.org/10.3389/fimmu.2019.00364.
Melgert BN, ten Hacken NH, Rutgers B, Timens W, Postma DS, Hylkema MN. More alternative activation of macrophages in lungs of asthmatic patients. J Allergy Clin Immunol. 2011;127:831–3. https://doi.org/10.1016/j.jaci.2010.10.045.
Ichikawa T, Hayashi R, Suzuki K, Imanishi S, Kambara K, Okazawa S, et al. Sirtuin 1 activator SRT1720 suppresses inflammation in an ovalbumin-induced mouse model of asthma. Respirology. 2013;18:332–9. https://doi.org/10.1111/j.1440-1843.2012.02284.x.
Zou B, Fu Y, Cao C, Pan D, Wang W, Kong L. Gentiopicroside ameliorates ovalbumin-induced airway inflammation in a mouse model of allergic asthma via regulating SIRT1/NF-kappaB signaling pathway. Pulm Pharmacol Ther. 2021;68: 102034. https://doi.org/10.1016/j.pupt.2021.102034.
Colley T, Mercado N, Kunori Y, Brightling C, Bhavsar PK, Barnes PJ, et al. Defective sirtuin-1 increases IL-4 expression through acetylation of GATA-3 in patients with severe asthma. J Allergy Clin Immunol. 2016;137(1595–7): e7. https://doi.org/10.1016/j.jaci.2015.10.013.
Zhang XY, Li W, Zhang JR, Li CY, Zhang J, Lv XJ. Roles of sirtuin family members in chronic obstructive pulmonary disease. Respir Res. 2022;23:66. https://doi.org/10.1186/s12931-022-01986-y.
Jang HY, Gu S, Lee SM, Park BH. Overexpression of sirtuin 6 suppresses allergic airway inflammation through deacetylation of GATA3. J Allergy Clin Immunol. 2016;138(1452–5): e13. https://doi.org/10.1016/j.jaci.2016.05.019.
Wang QL, Yang L, Liu ZL, Peng Y, Gao M, Deng LT, et al. Sirtuin 6 regulates macrophage polarization to alleviate sepsis-induced acute respiratory distress syndrome via dual mechanisms dependent on and independent of autophagy. Cytotherapy. 2022;24:149–60. https://doi.org/10.1016/j.jcyt.2021.09.001.
Piracha ZZ, Kwon H, Saeed U, Kim J, Jung J, Chwae YJ, et al. Sirtuin 2 isoform 1 enhances hepatitis B virus RNA transcription and DNA synthesis through the AKT/GSK-3beta/beta-catenin signaling pathway. J Virol. 2018. https://doi.org/10.1128/JVI.00955-18.
Wang J, Koh HW, Zhou L, Bae UJ, Lee HS, Bang IH, et al. Sirtuin 2 aggravates postischemic liver injury by deacetylating mitogen-activated protein kinase phosphatase-1. Hepatology. 2017;65:225–36. https://doi.org/10.1002/hep.28777.
Acknowledgements
This work was supported by KRIBB Research Initiative Program (KGM5242322) and the National Research Foundation of Korea grants funded by the Korean government (2022M3A9G8082645).
Author information
Authors and Affiliations
Contributions
Y-YK and SJ performed data curation, formal analysis, methodology, validation, investigation, and visualization. SWL, S-JL, and M-CR participated in methodology, software, and validation. S-HK and SL contributed to the study conceptualization, supervision, project administration, resources, and funding acquisition. The original draft was written by Y-YK, and reviewed/edited by S-HK and SL. The final version of the manuscript was read and approved by all authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, YY., Jeong, S., Lee, S.W. et al. Bakuchicin alleviates ovalbumin-induced allergic asthma by regulating M2 macrophage polarization. Inflamm. Res. (2024). https://doi.org/10.1007/s00011-024-01859-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00011-024-01859-8