Abstract
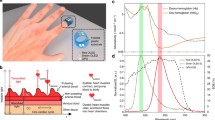
Pulse oximetry is the most widespread method of monitoring heart rate and blood oxygen levels in both clinical and non-clinical settings. Current devices are ridged, bulky, and suitable only for short-term use. While the next generation of devices are moving toward wearable technologies, this focus on being unobtrusive is insufficient. To enable continuous high quality long-term monitoring, implanted devices are required. These will eliminate interference from light and sensitivity to skin pigmentation, allow enhanced performance during movement, and have no concerns around percussive damage. Here, an inexpensive, ultra-flexible pulse oximetry probe is demonstrated. The hybrid devices are fabricated on 5 µm Parylene C using laser ablation to define the circuit, and integrate small, rigid optoelectronic components. These are demonstrated in vivo on anesthetized pigs. Both transmission mode, and the novel reflection mode, are shown to be effective geometries for this. The heart rate measured by these devices shows < 2% variance from concurrent peripheral pulse oximetry measurements, along with an average variance of around 2.5% attributed predominantly to differences between central and peripheral oxygen saturations. In addition, it is shown that when implemented directly on the femoral artery, these devices record a more acute response to the variation in oxygen intake compared to the peripheral measurements. Finally, the same devices are shown to have the potential for use in monitoring venous oxygen content. This could open up the possibility of continuous monitoring of arteriovenous oxygen difference. These devices are straightforward to produce, biocompatible, and can be easily implanted during cardiovascular surgery, offering a route toward long-term implantation for continuous patient monitoring.





Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
A. Jubran, Pulse oximetry. Crit. Care. 19(1), 272 (2015). https://doi.org/10.1186/s13054-015-0984-8
M.T. Petterson, V.L. Begnoche, J.M. Graybeal, The effect of motion on pulse oximetry and its clinical significance. Anesth. Analg 105(6), S78–S84 (2007). https://doi.org/10.1213/01.ane.0000278134.47777.a5
T.D. Brooks, D.A. Paulus, W.E. Winkle, Infrared heat lamps interfere with pulse oximeters. Anesthesiology 61(5), 630–630 (1984). https://doi.org/10.1097/00000542-198411000-00042
J.R. Feiner, J.W. Severinghaus, P.E. Bickler, Dark skin decreases the accuracy of pulse oximeters at low oxygen saturation: the effects of oximeter probe type and gender. Anesth. Analg. 105(6), S18–S23 (2007). https://doi.org/10.1213/01.ane.0000285988.35174.d9
P.E. Bickler, J.R. Feiner, J.W. Severinghaus, Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology 102(4), 715–719 (2005). https://doi.org/10.1097/00000542-200504000-00004
M.W. Sjoding, R.P. Dickson, T.J. Iwashyna, S.E. Gay, T.S. Valley, Racial bias in pulse oximetry measurement. N. Engl. J. Med. 383(25), 2477–2478 (2020). https://doi.org/10.1056/nejmc2029240
M. Rothmaier, B. Selm, S. Spichtig, D. Haensse, M. Wolf, Photonic textiles for pulse oximetry. Opt. Express 16(17), 12973 (2008). https://doi.org/10.1364/oe.16.012973
C.M. Lochner, Y. Khan, A. Pierre, A.C. Arias, All organic optoelectronic sensor for pulse oximetry. Nat. Commun. 5, 1–7 (2014). https://doi.org/10.1038/ncomms6745
Y. Khan, A.E. Ostfeld, C.M. Lochner, A. Pierre, A.C. Arias, Monitoring of vital signs with flexible and wearable medical devices. Adv. Mater. 28(22), 4373–4395 (2016). https://doi.org/10.1002/adma.201504366
J. Kim, P. Gutruf, A.M. Chiarelli, S.Y. Heo, K. Cho, Z. Xie et al., Miniaturized battery-free wireless systems for wearable pulse oximetry. Adv. Func. Mater. 27(1), 1–8 (2017). https://doi.org/10.1002/adfm.201604373
Y. Khan, D. Han, A. Pierre, J. Ting, X. Wang, C.M. Lochner et al., A flexible organic reflectance oximeter array. Proc. Natl. Acad. Sci. USA 115(47), E11015–E11024 (2018). https://doi.org/10.1073/pnas.1813053115
S. Biswas, Y. Shao, T. Hachisu, T. Nguyen-Dang, Y. Visell, Integrated soft optoelectronics for wearable health monitoring. Adv. Mater. Technol. 5(8), 1–9 (2020). https://doi.org/10.1002/admt.202000347
D. Han, Y. Khan, J. Ting, J. Zhu, C. Combe, A. Wadsworth et al., Pulse oximetry using organic optoelectronics under ambient light. Adv. Mater. Technol. 5(5), 1–9 (2020). https://doi.org/10.1002/admt.201901122
L.Z. Pipek, R.F.V. Nascimento, M.M.P. Acencio, L.R. Teixeira, Comparison of SpO2 and heart rate values on Apple Watch and conventional commercial oximeters devices in patients with lung disease. Sci. Rep. 11(1), 1–7 (2021). https://doi.org/10.1038/s41598-021-98453-3
I. Lee, N. Park, H. Lee, C. Hwang, J.H. Kim, S. Park, Systematic review on human skin-compatible wearable photoplethysmography sensors. Appl. Sci. 3(11), 2313 (2021). https://doi.org/10.3390/app11052313
M.M. Kmiec, D. Tse, J.M. Mast, R. Ahmad, P. Kuppusamy, Implantable microchip containing oxygen-sensing paramagnetic crystals for long-term, repeated, and multisite in vivo oximetry. Biomed. Microdevice 9(21), 71 (2019). https://doi.org/10.1007/s10544-019-0421-x
E.Y. Chen, D. Tse, H. Hou, W.A. Schreiber, P.E. Schaner, M.M. Kmiec et al., Evaluation of a refined implantable resonator for deep-tissue EPR oximetry in the clinic. Appl. Magn. Reson. 10(52), 1321–1342 (2021). https://doi.org/10.1007/s00723-021-01376-5
H.H. Asada, P. Shaltis, A. Reisner, R. Sokwoo, R.C. Hutchinson, Mobile monitoring with wearable photoplethysmographic biosensors. IEEE Eng. Med. Biol. Magaz. 22(3), 28–40 (2003). https://doi.org/10.1109/MEMB.2003.1213624
P. Bingger, J. Fiala, A. Seifert, N. Weber, K. Foerster, C. Heilmann, et al., In vivo monitoring of blood oxygenation using an implantable MEMS-based sensor. Proceedings of the IEEE International Conference on Micro Electro Mechanical Systems (MEMS), 1031–1034 (2010). https://doi.org/10.1109/MEMSYS.2010.5442385
M. Chushkin, L. Popova, E. Shergina, E. Krasnikova, O. Gordeeva, N. Karpina, Comparative analysis of the arterial oxygen saturation (SaO2) and pulse oximetry measurements (SpO2) in patients with pulmonary tuberculosis. Eur Resp So. (2020). https://doi.org/10.1183/13993003.congress-2020.3209
M. Thijssen, L. Janssen, J. le Noble, N. Foudraine, Facing SpO2 and SaO2 discrepancies in ICU patients: is the perfusion index helpful? J Clin Monitor Compu. 34(4), 693–698 (2020). https://doi.org/10.1007/s10877-019-00371-3
D. Journois, D. Safran, Monitorage continu de la saturation du sang veineux meleen oxygene. Annales Francaises d’Anesthesie et de Reanimation. 12(4), 393–408 (1993). https://doi.org/10.1016/S0750-7658(05)80107-8
S. Nebout, R. Pirracchio, Should we monitor ScVO2 in critically Ill patients? Cardiol. Res. Practice. 2012, 1–7 (2012). https://doi.org/10.1155/2012/370697
M. Khan, C.G. Pretty, A.C. Amies, J. Balmer, H.E. Banna, G.M. Shaw et al., Proof of concept non-invasive estimation of peripheral venous oxygen saturation. Biomed. Eng. Online 16(1), 1–16 (2017). https://doi.org/10.1186/s12938-017-0351-x
C.S. Robertson, R.K. Narayan, Z.L. Gokaslan, R. Pahwa, R.G. Grossman, P. Caram et al., Cerebral arteriovenous oxygen difference as an estimate of cerebral blood flow in comatose patients. J Neurosurg. 70(2), 222–230 (1989). https://doi.org/10.3171/jns.1989.70.2.0222
W. Lu, W. Bai, H. Zhang, C. Xu, A.M. Chiarelli, A. Vazquez-Guardado et al., Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation. Sci. Adv. 2(7), 22 (2021). https://doi.org/10.1126/sciadv.abe0579
N. Sugita, K. Obara, M. Yoshizawa, M. Abe, A. Tanaka, N. Homma, Techniques for estimating blood pressure variation using video images. Proc Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. EMBS. 2015(8), 4218–4221 (2015). https://doi.org/10.1109/EMBC.2015.7319325
J.M.J. Huttunen, L. Karkkainen, H. Lindholm, Pulse transit time estimation of aortic pulse wave velocity and blood pressure using machine learning and simulated training data. PLoS Comput. Biol. (2019). https://doi.org/10.1371/journal.pcbi.1007259
Y. Lee, J.D. Bok, H.J. Lee, H.G. Lee, D. Kim, I. Lee et al., Body temperature monitoring using subcutaneously implanted thermo-loggers from Holstein Steers. Asian-Australas. J. Anim. Sci. 29(2), 299–306 (2016). https://doi.org/10.5713/ajas.15.0353
A.J. Müller, M. Knuth, K.S. Nikolaus, R. Krivanek, F. Kuster, C. Hasslacher et al., Blood glucose self-monitoring with a long-term subconjunctival glucose sensor. J. Diab. Sci. Technol. 7(1), 24–34 (2013). https://doi.org/10.1177/193229681300700104
M. Mortellaro, A. DeHennis, Performance characterization of an abiotic and fluorescent-based continuous glucose monitoring system in patients with type 1 diabetes. Biosens. Bioelectron. 2014(61), 227–231 (2014). https://doi.org/10.1016/j.bios.2014.05.022
F. Lellouche, P.A. Bouchard, M. Karimi, N. Juteau, Q. Mascret, E. Bharucha et al., Proof of concept for implantable oximetry: results of a feasibility study. Am. Thorac. Soc. (2019). https://doi.org/10.1164/ajrccm-conference.2019.199.1
S. Kuppusami, R.H. Oskouei, Parylene coatings in medical devices and implants: a review. Univ. J. Biomed. Eng.. 3(2), 9–14 (2015). https://doi.org/10.13189/ujbe.2015.030201
C. Hassler, R.P. Von Metzen, P. Ruther, T. Stieglitz, Characterization of Parylene C as an encapsulation material for implanted neural prostheses. J Biomed. Mater. Res.—B Appl. Biomater. 93(1), 266–274 (2010). https://doi.org/10.1002/jbm.b.31584
A. Lecomte, A. Degache, E. Descamps, L. Dahan, C. Bergaud, In vitro and in vivo biostability assessment of chronically-implanted Parylene C neural sensors. Sens Actuat B. 251, 1001–1008 (2017). https://doi.org/10.1016/j.snb.2017.05.057
J. del Valle, N. de la Oliva, M. Muller, T. Stieglitz, X. Navarro, Biocompatibility evaluation of Parylene C and polyimide as substrates for peripheral nerve interfaces. IEEE (2015). https://doi.org/10.1109/NER.2015.7146654
N. De La Oliva, M. Mueller, T. Stieglitz, X. Navarro, J. Del Valle, On the use of Parylene C polymer as substrate for peripheral nerve electrodes. Sci. Rep. 8(1), 1–12 (2018). https://doi.org/10.1038/s41598-018-24502-z
VSi.: Parylene biocompatibility—it does a body good. https://vsiparylene.com/resources/parylene-biocompatibility/
D. Zeniieh, L. Ledernez, G. Urban, Parylene-C as high performance encapsulation material for implantable sensors. Procedia Eng. 87, 1398–1401 (2014). https://doi.org/10.1016/j.proeng.2014.11.704
M. Golda-Cepa, K. Engvall, M. Hakkarainen, A. Kotarba, Recent progress on Parylene C polymer for biomedical applications: a review. Progress Org Coat. 3(140), 105493 (2020). https://doi.org/10.1016/j.porgcoat.2019.105493
S. Reichelt, J. Fiala, A. Werber, K. Forster, C. Heilmann, R. Klemm et al., Development of an implantable pulse oximeter. IEEE Trans. Biomed. Eng. 55(2), 581–588 (2008). https://doi.org/10.1109/TBME.2007.902242
P. Bingger, J. Fiala, A. Seifert, N. Weber, A. Moser, F. Goldschmidtboeing, et al., Implantable multi sensor system for in vivo monitoring of cardiovascular parameters. TRANSDUCERS 2009—15th Int. Conf. Solid-State Sens. Actuat. Microsyst., 1469–1472 (2009). https://doi.org/10.1109/SENSOR.2009.5285821
M. Theodor, D. Ruh, S. Subramanian, K. Forster, C. Heilmann, F. Beyersdorf et al., Implantable pulse oximetry on subcutaneous tissue. 2014 36th Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. EMBC 2014, 2089–2092 (2014). https://doi.org/10.1109/EMBC.2014.6944028
L. Lu, P. Gutruf, L. Xia, D.L. Bhatti, X. Wang, A. Vazquez-Guardado, et al., Wireless optoelectronic photometers for monitoring neuronal dynamics in the deep brain. Proc. Natl. Acad. Sci. USA 2(115), E1374–E1383 (2018). https://doi.org/10.1073/pnas.1718721115
H. Zhang, P. Gutruf, K. Meacham, M.C. Montana, X. Zhao, A.M. Chiarelli et al., Wireless, battery-free optoelectronic systems as subdermal implants for local tissue oximetry. Sci. Adv. (2019). https://doi.org/10.1126/sciadv.aaw0873
R.M. Pearse, A. Rhodes, Mixed and central venous oxygen saturation. Yearbook Intensive Care Emerg. Med. 2005, 592–602 (2005). https://doi.org/10.1007/0-387-26272-551
Frazier J. Theory and clinical application of continuous fiberoptic central venous oximetry (ScvO2) monitoring. Irvine, California: Edwards Lifesciences. https://edwardsprodjp.blob.core.windows.net/media/Zh/devices/monitoring/hemodynamic%20monitoring/ar12912-pediasatheory clinical app 1lr.pdf. Accessed 10 Sept 2022
J.G. Webster, Design of pulse oximeters (Institute of Physics Publishing, Bristol, 1997)
J. Moyle, Pulse oximetry (BMJ Books, London, 2002)
P.D. Mannheimer, The light-tissue interaction of pulse oximetry. Anesth. Analg. 12(105), S10–S17 (2007). https://doi.org/10.1213/01.ane.0000269522.84942.54
M. van Gastel, S. Stuijk, G. De Haan, New principle for measuring arterial blood oxygenation, enabling motion-robust remote monitoring. Sci. Rep. 6(November), 1–16 (2016). https://doi.org/10.1038/srep38609
J.E. Sinex, Pulse oximetry: principles and limitations. Am. J. Emerg. Med. 1(17), 59–66 (1999). https://doi.org/10.1016/S0735-6757(99)90019-0
N. Stubán, N. Masatsugu, Non-invasive calibration method for pulse oximeters. Periodica Polytechn. Electr. Eng. 52(1–2), 91 (2008). https://doi.org/10.3311/pp.ee.2008-1-2.11
P.D. Mannheimer, J.R. Casciani, M.E. Fein, S.L. Nierlich, Wavelength selection for low-saturation pulse oximetry. IEEE Trans. Biomed. Eng. 44(3), 148–158 (1997). https://doi.org/10.1109/10.554761
S.K. Lyons, P.S. Patrick, K.M. Brindle, Imaging mouse cancer models in vivo using reporter transgenes. Cold Spring Harb. Protoc. 2013(8), 685–699 (2013). https://doi.org/10.1101/pdb.top069864
H. Kobayashi, M. Ogawa, R. Alford, P.L. Choyke, Y. Urano, New strategies for fluorescent probe design in medical diagnostic imaging. Chem. Rev. 110(5), 2620–2640 (2010). https://doi.org/10.1021/cr900263j
M. Faulhaber, H. Gatterer, T. Haider, T. Linser, N. Netzer, M. Burtscher, Heart rate and blood pressure responses during hypoxic cycles of a 3-Week intermittent hypoxia breathing program in patients at risk for or with mild COPD. Int. J. COPD. 10, 339–345 (2015). https://doi.org/10.2147/COPD.S75749
J.D. Campbell, C.G. Pretty, J.G. Chase, P.J. Bones, Near-real-time detection of pulse oximeter PPG peaks using wavelet decomposition. IFAC-Papers OnLine. 51(27), 146–151 (2018). https://doi.org/10.1016/j.ifacol.2018.11.652
P.H.C. Eilers, A perfect smoother. Anal. Chem. 75(14), 3631–3636 (2003). https://doi.org/10.1021/ac034173t
P.H. Eilers, H.F. Boelens, Baseline correction with asymmetric least squares smoothing. Leiden Univ Med Centre Rep. 1(1), 5 (2005)
U.A. Leuenberger, J.C. Hardy, M.D. Herr, K.S. Gray, L.I. Sinoway, Hypoxia augments apnea-induced peripheral vasoconstriction in humans. J. Appl. Physiol. 90(4), 1516–1522 (2001). https://doi.org/10.1152/jappl.2001.90.4.1516
V.A. Imadojemu, K. Gleeson, K.S. Gray, L.I. Sinoway, U.A. Leuenberger, Obstructive apnea during sleep is associated with peripheral vasoconstriction. Am. J. Res. Crit. Care Med. 165(1), 61–66 (2002). https://doi.org/10.1164/ajrccm.165.1.2009062
A. Schäfer, I. Vagedes, How accurate is pulse rate variability as an estimate of heart rate variability? Int. J. Cardiol. 166(1), 15–29 (2013). https://doi.org/10.1016/j.ijcard.2012.03.119
Walton, Z.D.: Measuring Venous Oxygen Saturation Using the Photoplethysmograph Waveform [Doctor of Medicine]. Yale.
K. Shafqat, R.M. Langford, P.A. Kyriacou, Estimation of instantaneous venous blood saturation using the photoplethysmograph waveform. Physiol. Meas. 10(36), 2203–2214 (2015). https://doi.org/10.1088/0967-3334/36/10/2203
I. Garcıa-Lopez, E. Rodriguez-Villegas, Extracting the jugular venous pulse from anterior neck contact photoplethysmography. Sci. Rep. 12(10), 3466 (2020). https://doi.org/10.1038/s41598-020-60317-7
Chapter one—introduction to exercise physiology. In: Glynn, A., Fiddler, H., Demetriou-Swanwick, R., Watkins, V., Dickie, A., Sukumar, S. et al., Eds. The physiotherapist’s pocket guide to exercise. Edinburgh: Churchill Livingstone, pp. 1–11 (2009).
T. LaPier, Impaired aerobic capacity/endurance, 3rd edn. (Elsevier Inc., 2012)
P. Schonle, Q. Wang, N. Brun, J. Bosser, P. Meier, Q. Huang, Towards an implantable telemetry system for SpO2 and PWV measurement in small animals. IEEE (2017). https://doi.org/10.1109/BIOCAS.2017.8325211
J. Fiala, R. Gehrke, N. Weber, P. Bingger, H. Zappe, A. Seifert, Implantable optical sensor for continuous monitoring of various hemoglobin derivatives and tissue perfusion. IEEE (2009). https://doi.org/10.1109/ICSENS.2009.5398324
F. Marefat, R. Erfani, K.L. Kilgore, P. Mohseni, Minimally invasive muscle-based recording of photoplethysmogram toward chronic implantation. IEEE (2016). https://doi.org/10.1109/BioCAS.2016.7833813
J.M. Valero-Sarmiento, P. Ahmmed, A. Bozkurt, In vivo evaluation of a subcutaneously injectable implant with a low-power photoplethysmography ASIC for animal monitoring. Sensors. 12(20), 7335 (2020). https://doi.org/10.3390/s20247335
M. Chan, V. Ganti, J. Heller, C. Abdallah, M. Etemadi, O. Inan, Enabling continuous wearable reflectance pulse oximetry at the sternum. Biosensors 11(12), 521 (2021). https://doi.org/10.3390/bios11120521
Integrated analog front-end for pulse oximeters AFE4490; 2013. https://www.ti.com/lit/ds/symlink/afe4490.pdf. Accessed 10 Sept 2022
Bhat, V., Vaithy, B., Whitchurch, A., Kandan, M., Joice, T.M.: AFE4490 oximeter. GitHub. https://github.com/Protocentral/AFE4490Oximeter
S. de Mulatier, D. Coulon, R. Delattre, S. Blayac, M. Ramuz, Copper-leaf-based process for imperceptible computational electronics. Adv. Electron. Mater. (2020). https://doi.org/10.1002/aelm.201900787
C.D. Lee, E. Meng, Mechanical proper ties of thin-film Parylene–metal–Parylene devices. Front. Mech. Eng. 1(Sept), 1–14 (2015). https://doi.org/10.3389/fmech.2015.00010
T. Graven-Nielsen, L. Arendt-Nielsen, S. Mense, Thermosensitivity of muscle: High-intensity thermal stimulation of muscle tissue induces muscle pain in humans. J. Physiol. 540(2), 647–656 (2002). https://doi.org/10.1113/jphysiol.2001.013336
P.E. Bickler, J.R. Feiner, M.S. Lipnick, P. Batchelder, D.B. MacLeod, J.W. Severinghaus, Effects of acute, profound hypoxia on healthy humans. Anesth. Analg. 124(1), 146–153 (2017). https://doi.org/10.1213/ANE.0000000000001421
Acknowledgements
We thank the ID-Fab platform at the Centre Microélectronique de Provence for their support in preparing the devices used here.
Author information
Authors and Affiliations
Contributions
MR conceived the project. JT and MR designed the experiments. JT prepared materials and analyzed experimental data. JT, PB and MR performed the experiments. JT wrote the manuscript and prepared the figures. MR and PB revised the manuscript. MR supervised this work and provided financial support.
Corresponding author
Ethics declarations
Conflict of interest
The authors are aware of no conflicts of interest.
Ethical Approval
The animals were used in accordance with institutional and national guidelines for the care and use of animals. The experiments conducted on animals have been evaluated and accepted by an Ethical Committee (APAFIS#6342). Four Pietrain pigs (40 ± 5 kg) were used in total.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Troughton, J.G., Brige, P. & Ramuz, M. Flexible, Implantable, Pulse Oximetry Sensors: Toward Long-Term Monitoring of Blood Oxygen Saturations. Biomedical Materials & Devices 1, 912–924 (2023). https://doi.org/10.1007/s44174-022-00057-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44174-022-00057-6