Abstract
Background
The effect of severity of screening result on delays to diagnosis has primarily been examined for mammographic abnormalities. This study will examine delays to assessment and diagnosis for women with an abnormal mammogram compared to women with an abnormal clinical breast examination (CBE) or abnormal CBE and mammogram.
Methods
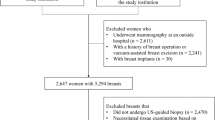
Using data routinely collected by Ontario Breast Screening Program (OBSP), 12,675 women aged 50 to 69 with an abnormal screening result between January 1, 2000 and December 31, 2000 were followed prospectively to the completion of their assessment process. Median waiting times from abnormal screen to first assessment procedure and diagnosis were compared by modality of referral and among women with a breast cancer diagnosis by prognostic features.
Results
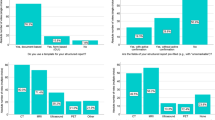
The median waiting time to first assessment and to diagnosis was significantly longer for women with only a clinical abnormality compared to women with a mammographic abnormality. In addition, women diagnosed with cancers of larger size had longer delays when the abnormality was detected only clinically. However, women referred by both modalities had significantly shorter waiting times to first assessment procedure and to diagnosis of poor prognosis cancers compared to women referred by mammography alone.
Interpretation
Women with an abnormal CBE and mammogram are assessed more promptly and have shorter diagnostic times. However, women with only a CBE abnormality had delays to diagnosis as a result of longer waiting times to first assessment procedure. Integration of the OBSP with assessment centres should improve times to diagnosis irrespective of modality of referral.
Résumé
Contexte
Le rapport entre la gravité du résultat d’un test de dépistage et le délai d’obtention d’un diagnostic a surtout été étudié pour les mammographies anormales. Nous avons étudié les délais d’évaluation et de diagnostic des femmes ayant eu des résultats anormaux à une mammographie, et nous les avons comparés aux délais des femmes ayant eu des résultats anormaux à un examen clinique des seins (ECS), ou à un ECS combiné à une mammographie.
Méthode
à l’aide des données recueillies systématiquement par le Programme ontarien de dépistage du cancer du sein, nous avons suivi rétrospectivement 12 675 femmes âgées de 50 à 69 ans ayant obtenu des résultats anormaux entre le 1er janvier et le 31 décembre 2000 jusqu’à l’aboutissement de leur processus d’évaluation. Nous avons comparé les délais d’attente médians entre le test de dépistage et la première évaluation et le diagnostic, d’abord selon le mode d’acheminement des patientes, puis, pour les femmes ayant reçu un diagnostic de cancer du sein, selon leur pronostic.
Résultats
Le délai d’attente médian avant la première évaluation et le diagnostic était sensiblement plus long pour les femmes ayant eu un ECS anormal que pour celles ayant eu une mammographie anormale. De plus, les femmes chez qui on avait diagnostiqué des cancers avancés attendaient plus longtemps lorsque l’anomalie avait été décelée par ECS seulement. Toutefois, les femmes dirigées après un ECS combiné à une mammographie attendaient sensiblement moins longtemps avant la première évaluation, et donc avant le diagnostic de cancer avancé, que les femmes dirigées après une mammographie seulement.
Interprétation
Les femmes dont l’ECS et la mammographie sont tous les deux anormaux sont évaluées plus rapidement, et elles attendent moins longtemps leur diagnostic. Pour les femmes n’ayant qu’un ECS anormal, le délai de diagnostic est plus long, du fait qu’elles attendent plus longtemps avant leur première évaluation. En intégrant le Programme ontarien de dépistage du cancer du sein dans les centres d’évaluation, on devrait pouvoir améliorer les délais de diagnostic, quel que soit le mode d’acheminement des patientes.
Similar content being viewed by others
References
Kerlikowske K, Grady D, Rubin SM, Sandrock C, Ernster VL. Efficacy of screening mammography. A meta-analysis. JAMA 1995;273:149–54.
Humphrey LL, Helfand M, Chan BKS, Woolf SH. Breast cancer screening. A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002;137:347–60.
IARC Working Group. Handbooks of Cancer Prevention, Volume 7: Breast Cancer Screening. Lyon, France: IARC Press, 2002;87–117.
The Workshop Group. Reducing deaths from breast cancer in Canada-Workshop report. CMAJ 1989;141:199–201.
Rimer BK, Bluman LG. The psychosocial conse-quences of mammography. J Nat Cancer Inst Monogr 1997;22:131–38.
Bret J, Austoker J, Ong G. Do women who undergo further investigation for breast screening suffer adverse psychological consequences? A multi-centre follow-up study comparing different breast screening result groups five months after their last breast screening appointment. J Pub Health Med 1998;20:396–403.
Brett J, Austoker J. Women who are recalled for further investigation for breast screening: Psychological consequences 3 years after recall and factors affecting reattendance. J Pub Health Med 2001;23:292–300.
Olivotto IA, Gomi A, Bancej C, Brisson J, Tonita J, Kan L, et al. Influence to delay to diagnosis on prognostic indicators of screen-detected breast carcinoma. Cancer 2002;94:2143–50.
Ganry O, Peng J, Dubreuil A. Influence of abnormal screen on delays and prognostic indicators of screen-detected breast carcinoma. J Med Screen 2004;11:28–31.
Caplan LS, May DS, Richardson L. Time to diagnosis and treatment of breast cancer: Results from the National Breast and Cervical Cancer Early Detection Program, 1991–1995. Am J Public Health 2000;90:130–34.
Olivotto IA, Bancej C, Goel V, Snider J, McAuley RG, Irvine B, et al. Waiting times from abnormal breast screen to diagnosis in 7 Canadian provinces. CMAJ 2001;165:277–83.
Duijm LEM, Groenewould JH, Jansen FH, Fracheboud J, vanBeek M, deKoning HJ. Mammography screening in the Netherlands: Delay in the diagnosis of breast cancer after breast cancer screening. Br J Cancer 2004;91;1795–99.
Shootman M, Myers-Geadelmann J, Laurence F. Factors associated with adequacy of diagnostic workup after abnormal breast cancer screening results. J Am Board Fam Pract 2000;13:94–100.
Ballard-Barbash R, Klabunde C, Paci E, Broeders M, Coleman EA, Fracheboud J, et al. Breast cancer screening in 21 countries: Delivery of services, abnormal breast screening result. Cancer Detection and Prevention 2004;28:361–67.
Libstug AR, Moravan V, Aitken SE. Results from the Ontario Breast Screening Program, 1990–1995. J Med Screen 1998;5:73–80.
Kuzma JW, Bohnenblust SE. Basic Statistics for the Health Sciences. Mountain View, CA: Mayfield Publishing Company, 2001;238–45.
SAS Institute Inc.: SAS System version 6.12. Cary, North Carolina, 1989–1996.
Psooy BJ, Schreuer D, Borganokar J, Caines JS. Patient navigation: Improving timeliness in the diagnosis of breast abnormalities. Can Assoc Radiol J 2004;55:145–50.
Olivotto IA, Borugian MJ, Kan L, Harris SR, Rousseau EJ, Thorne SE, et al. Improving the time to diagnosis after an abnormal screening mammogram. Can J Public Health 2001;92:366–71.
Decker KM, Harrison M, Chateau D. Influence of direct referrals on time to diagnosis after an abnormal breast screening result. Cancer Detection and Prevention 2004;28:361–67.
Miller AB. Organized breast cancer screening in Canada. CMAJ 2000;163:1150–51.
Report of the Working Group on the Integration of Screening and Diagnosis for the Canadian Breast Cancer Screening Initiative. Waiting for a diagnosis after an abnormal breast cancer screen in Canada. Ottawa: Health Canada, 2000. Cat No. H39-526/2000E, pp. 21–22. https://doi.org/www.phac-aspc.gc.ca/ccdpc-cpcmc/bc-cds/pdf/diagnosis-report_e.pdf.
Canadian Breast Cancer Screening Initiative. Organized Breast Cancer Screening Programs in Canada: 1999 and 2000 Report. Ottawa: Health Canada, 2003. Cat. No. H1-9/13-2000, pp 27. https://doi.org/www.phac-aspc.gc.ca/publicat/obcsp- podcs00/index.html.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiarelli, A.M., Mai, V., Halapy, E.E. et al. Effect of Screening Result on Waiting Times to Assessment and Breast Cancer Diagnosis. Can J Public Health 96, 259–263 (2005). https://doi.org/10.1007/BF03405159
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03405159