Abstract
Background: Limitations associated with the under-reporting of enteric illnesses have long been recognized but the extent and variation of this under-reporting in Canada has not been examined. Given the public health value of surveillance data, a closer examination of under-reporting of enteric illnesses in Canada was warranted.
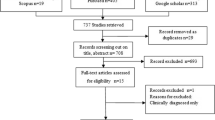
Methods: Paper-based surveys were administered (a) to all laboratories in Canada licensed to process stool specimens and (b) to all local public health authorities in two provinces.
Results: Of the laboratories surveyed, 67% (n=274) conducted on-site testing of stool specimens for enteric bacteria, 31% (n=126) for parasites and 10% (n=42) for viruses. In the year 2000, these laboratories processed 459,982 stool specimens, of which 5%, 15%, 8% and 19% were positive for enteric bacteria (excluding C. difficile), C. difficile, parasites and viruses, respectively. Variations in laboratory testing and health authority reporting protocols and policies were identified. Of the laboratory-confirmed cases of AGI reported to local public health authorities, 5% (n=846) were not reported to provincial counterparts.
Conclusion: A significant proportion of AGI cases submitting stool specimens are not captured in Canada’s passive surveillance system due to unknown etiology. A much smaller proportion of laboratory-confirmed cases reported to local public health authorities are not captured at the provincial or national level.
Given that the number of laboratory-confirmed AGI cases represents such a small fraction of all community cases, strategies to compensate for under-reporting and efforts directed at harmonizing laboratory and local public health authority policies and practices would be welcomed.
Résumé
Contexte: On connaît depuis longtemps les limites associées à l’insuffisance de notification des maladies entériques, mais l’envergure et les variations de cette sous-notification au Canada n’ont pas été étudiées. Étant donné l’utilité des données de surveillance pour la santé publique, la sous-notification des maladies entériques au Canada mérite que l’on s’y intéresse de plus près.
Méthode: Nous avons administré des questionnaires écrits a) dans tous les laboratoires du Canada autorisés à analyser des échantillons de selles et b) auprès de toutes les autorités locales de santé publique de deux provinces.
Résultats: De tous les laboratoires sondés, 67 % (n=274) procédaient sur place à la détection d’entébactéries, 31 % (n=126) à la détection de parasites, et 10 % (n=42) à la détection de virus dans des échantillons de selles. En 2000, ces laboratoires avaient analysé 459 982 échantillons de selles, dont 5 %, 15 %, 8 % et 19 % avaient révélé la présence d’entébactéries (autres que C. difficile), de C. difficile, de parasites et de virus, respectivement. Nous avons constaté des écarts entre les épreuves de laboratoire et les protocoles et politiques des autorités sanitaires en matière de rapports. Sur les cas de maladie gastro-intestinale aiguë (MGA) confirmés en laboratoire et déclarés aux autorités locales de santé publique, 5 % (n=846) n’avaient pas été déclarés aux autorités provinciales.
Conclusion: Une proportion significative des cas de MGA qui soumettent des échantillons de selles n’est pas enregistrée par le système de surveillance passive du Canada en raison d’une étiologie inconnue. La proportion des cas confirmés en laboratoire et déclarés aux autorités locales de santé publique qui ne sont pas enregistrés au palier provincial ou national est beaucoup plus faible. Puisque le nombre de cas de MGA confirmés en laboratoire représente une si petite fraction de tous les cas dans la population, il serait bon d’avoir des stratégies pour pallier l’insuffisance de notification et de consacrer des efforts à l’harmonisation des politiques et des pratiques des laboratoires et des autorités locales de santé publique.
Similar content being viewed by others
References
Handysides S. Underascertainment of infectious intestinal disease. Commun Dis Public Health 1999;2:78–79.
Van Gilder T, Christensen D, Shallow S, Fiorentino T, Desai S, Wicklund J, et al. Variations in stool handling and culturing practices among clinical microbiology laboratories within the Foodborne Diseases Active Surveillance network (FoodNet): Do we need practice guidelines? 99th American Society of Microbiology. Chicago, IL, June 1999 (Abstract).
Wheeler JG, Sethi D, Cowden JM, Wall PG, Rodrigues LC, Tompkins DS, et al. Study of infectious intestinal disease in England: Rates in the community, presenting to general practice, and reported to national surveillance. The Infectious Intestinal Disease Study Executive. BMJ 1999;318:1046–50.
Valenstein P, Pfaller M, Yungbluth M. The use and abuse of routine stool microbiology: A College of American Pathologists Q-probes study of 601 institutions. Arch Pathol Lab Med 1996;120:206–11.
Craven D, Brick D, Morrisey A, O’Riordan MA, Petran V, Schreiber JR. Low yield of bacterial stool culture in children with nosocomial diarrhea. Pediatr Infect Dis J 1998;17:1040–44.
de Wit MAS, Koopmans MPG, Kortbeek LM, van Leeuwen NJ, Bartelds AIM, van Duynhoven YTHP. Gastroenteritis in sentinel general practices, the Netherlands. Emerging Infectious Diseases 2001;7:82–91.
Fan K, Morris AJ, Reller LB. Application of rejection criteria for stool cultures for bacterial enteric pathogens. J Clin Microbiol 1993;31:2233–35.
McIver CJ, Hansman G, White P, Doultree JC, Catton M, Rawlinson WD. Diagnosis of enteric pathogens in children with gastroenteritis. Pathology 2001;33:353–58.(Abstract).
Rohner P, Pittet D, Pepey B, Nije-Kinge T, Auckenthaler R. Etiological agents of infectious diarrhea: Implications for requests for microbial culture. J Clin Microbiol 1997;35:1427–32.
Tompkins DS, Hudson MJ, Smith HR, Eglin RP, Wheeler JG, Brett MM, et al. A study of infectious intestinal disease in England: Microbiological findings in cases and controls. Commun Dis Public Health 1999;2:108–13.
Zaidi AK, Macone A, Goldmann AD. Impact of simple screening criteria on utilization of low-yield bacterial stool cultures in a Children’s Hospital. Pediatrics 1999;103:1189–92.
Alfa MJ, Du T, Beda G. Survey of incidence of Clostridium difficile infection in Canadian hospitals and diagnostic approaches. J Clin Microbiol 1998;36:2076–80.
Siegel DL, Edelstein PH, Nachamkin I. Inappropriate testing for diarrheal diseases in the hospital. JAMA 1990;263:979–82.(Abstract).
Morris AJ, Wilson ML, Reller LB. Application of rejection criteria for stool ovum and parasite examinations. J Clin Microbiol 1992;30:3213–16.
Marie-Cardine A, Gourlain K, Mouterde O, Castignolles N, Hellot MF, Mallet E, et al. Epidemiology of acute viral gastroenteritis in children hospitalized in Rouen, France. CID 2002;34:1170–78.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flint, J.A., Doré, K., Majowicz, S.E. et al. From Stool to Statistics. Can J Public Health 95, 309–313 (2004). https://doi.org/10.1007/BF03405138
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03405138