Abstract
Objectives: Prenatal alcohol exposure is a significant public health issue with lifelong psychological, emotional and financial costs associated with caring for an affected individual. In 2005, the Public Health Agency of Canada and Health Canada’s First Nations and Inuit Health Branch developed evidence-based guidelines for the diagnosis of a Fetal Alcohol Spectrum Disorder (FASD). We examined the extent to which prenatal records across Canadian provinces and territories currently integrate key recommendations from these guidelines.
Methods: A content analysis of prenatal record forms retrieved from each Canadian province and territory (N=12) was conducted to identify all questions or intervention prompts related to prenatal screening, exposure assessment, counseling or referral for maternal alcohol use during pregnancy. Findings were reviewed in relation to recommendations extrapolated from the Canadian guidelines and the FASD literature.
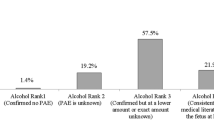
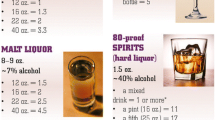
Results: All the prenatal record forms contained questions to assess maternal alcohol use during pregnancy. However, the dimensions of alcohol consumption assessed and the format, wording and number of items related to each dimension varied markedly across provinces/territories. Only five prenatal record forms included a validated screening tool to identify risky alcohol drinking behaviour. Most of the forms lacked prompts to encourage providers to intervene or refer pregnant clients with high-risk drinking behaviour.
Conclusion: Integration of the Canadian recommendations into Canadian prenatal record forms may be an effective public health strategy for helping identify pregnancies at high risk for alcohol exposure, reducing the incidence of a FASD through appropriate prenatal intervention and referral, and facilitating early diagnosis of a FASD.
Résumé
Objectifs: L’exposition prénatale à l’alcool est une importante question de santé publique, entraînant des coûts financiers, émotionnels et psychologiques associés aux soins à donner à une personne affectée, et ce, pendant toute une vie. En 2005, l’Agence canadienne de la santé publique et la Direction générale de la santé des Premières nations et des Inuits (DGSPNI) ont élaboré des lignes directrices fondées sur des données probantes pour le diagnostic de l’ensemble des troubles causés par l’alcoolisation fœtale (ETCAF). Nous avons examiné la mesure dans laquelle les dossiers prénataux des provinces et des territoires canadiens intègrent actuellement les recommandations clés de ces lignes directrices.
Méthodes: Nous avons mené une analyse du contenu des formulaires prénataux récupérés dans chaque province et territoire du Canada (N=12) afin de déterminer toutes les questions ou les moteurs d’intervention liés au dépistage prénatal, à l’évaluation de l’exposition, à la consultation ou à la recommandation en ce qui a trait à la consommation d’alcool pendant la grossesse. Nous avons examiné les résultats en relation avec les recommandations extrapolées des lignes directrices canadiennes et de la documentation sur l’ETCAF.
Résultats: Tous les formulaires prénataux contenaient des questions visant à évaluer la consommation d’alcool par la mère pendant la grossesse. Toutefois, l’ampleur et la forme consommation d’alcool évaluée, le vocabulaire et le nombre d’articles associé à chaque forme, variaient considérablement entre les provinces et les territoires. Seulement cinq formulaires prénataux comprenaient un outil de dépistage validé permettant de déterminer la présence d’un comportement associé à une consommation d’alcool à risque. Nous avons pu noter l’absence de messages-guides dans les formulaires pour encourager les fournisseurs de soins à intervenir ou à diriger les clientes enceintes présentant une consommation d’alcool à risque élevé.
Conclusion: L’intégration des recommandations canadiennes dans les formulaires prénataux serait une stratégie de santé publique efficace pour aider à déceler les grossesses présentant un risque élevé d’exposition à l’alcool, à réduire l’incidence d’ETCAF grâce à une intervention prénatale et à des recommandations, et à faciliter le diagnostic précoce de l’ETCAF.
Similar content being viewed by others
References
Streissguth AP, O’Malley K. Neuropsychiatric implications and long-term consequences of fetal alcohol spectrum disorders. Semin Clin Neuropsychiatry 2000;5(3):177–90.
Clarren SK, Smith DW. The fetal alcohol syndrome. N Engl J Med 1978;298(19):1063–67.
Connor P, Streissguth A. Effects of prenatal exposure to alcohol across the life span. Alcohol Health Res World 1996;20(3):170–74.
Sokol RJ, Clarren SK. Guidelines for use of terminology describing the impact of prenatal alcohol on the offspring. Alcoholism Clin Exp Res 1989;13(4):597–98.
A document review and synthesis of information on Fetal Alcohol Spectrum Disorders (FASD) in Atlantic Canada, 2007. Prepared by Gary Roberts and Associates for the Public Health Agency of Canada, Atlantic Region, and Health Canada, Atlantic Region — First Nations and Inuit Health.
Health Canada. It takes a community: Fetal alcohol spectrum disorder. Ottawa, ON: Minister of Health (published in collaboration with the Public Health Agency of Canada), 2006. Available online at: http://www.hc-sc.gc.ca/iyh-vsv/diseases-maladies/fasd-etcaf_e.html (Accessed June 20, 2008).
Abel EL, Sokol RJ. A revised conservative estimate of the incidence of FAS and its economic impact. Alcohol Clin Exp Res 1991;15(3):514–24.
Poitra BA, Marion S, Dionne M, Wilkie E, Dauphinais P, Wilkie-Pepion M, et al. A school-based screening program for fetal alcohol syndrome. Neurotoxi-col Teratol 2003;25(6):725–29.
Williams RJ, Odaibo FS, McGee JM. Incidence of fetal alcohol syndrome in northeastern Manitoba. Can J Public Health 1999;90(3):192–94.
Anderson B, Novick E. Fetal alcohol syndrome and pregnant women who abuse alcohol: An overview of the issue and the federal response. Washington, DC: Division of Children and Youth Policy (DHHS), 1992.
Smith I, Coles C. Multilevel intervention for prevention of fetal alcohol syndrome and effects of prenatal alcohol exposure. Recent Dev Alcohol 1991;9:165–80.
Roberts G, Nanson, J. Best practices: Fetal alcohol syndrome/fetal alcohol effects and the effects of other substance use during pregnancy. Ottawa: Minister of Public Works and Government Services Canada, Health Canada, 2001.
Masotti P, Szala-Meneok K, Selby P, Ranford J, Van AK. Urban FASD interventions: Bridging the cultural gap between Aboriginal women and primary care physicians. J FAS International 2003;1(e17):1–8.
Stade B. The burden of prenatal exposure to alcohol: Measurement of quality of life and costs [dissertation]. Toronto: University of Toronto, 2002.
Stade B, Ungar WJ, Stevens B, Beyen J, Koren G. Cost of fetal alcohol spectrum disorder in Canada. Can Fam Phys 2007;53(8):1303–4.
Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ 2005;172(5 Suppl):S1–S21.
Burd L, Martsolf J, Klug MG, O’Conner E, Peterson M. Prenatal alcohol exposure assessment: Multiple embedded measures in a prenatal questionnaire. Neurotoxicol Teratol 2003;26(6):675–79.
Burd L, Klug MG, Martsolf JT, Martsolf C, Deal E, Kerbeshian J. A staged screening strategy for prenatal alcohol exposure and maternal risk stratification. J R Soc Health 2006;126(2):86–94.
Maier SE, West JR. Drinking patterns and alcohol-related birth defects. Alcohol Res Health 2001;25(3):168–74.
Stromland K. Fetal alcohol syndrome — A birth defect recognized worldwide. Fetal & Maternal Med Rev 2004;15(1):59–71.
Royal College of Obstetricians and Gynaecologists. Alcohol consumption and the outcomes of pregnancy. RCOG Statement No. 5., 2006.
Public Health Agency of Canada. Table G3.2 — Rate of maternal alcohol consumption during pregnancy, by province/region, Canada, 2000–2001, 2003 and 2005. Canadian Perinatal Health Report, 2008 Edition. Ottawa: Published by authority of the Minister of Health, 2008, p. 240. Available online at: http://www.phac-aspc.gc.ca/publicat/2008/cphr-rspc/pdf/cphr-rspc08-eng.pdf (Accessed February 8, 2009).
Chang G, McNamara TK, Orav EJ, Koby D, Lavigne A, Ludman B, et al. Brief intervention for prenatal alcohol use: A randomized trial. Obstet Gynecol 2005;105(5 Pt 1):991–98.
Tough S, Clarke K, Cook J. Fetal alcohol spectrum disorder prevention approaches among Canadian physicians by proportion of Native/Aboriginal patients: Practices during the preconception and prenatal periods. Matern Child Health J 2007;11(4):385–93.
Kesmodel U. Binge drinking in pregnancy — Frequency and methodology. Am J Epidemiol 2001;154(8):777–82.
Tough S, Tofflemire K, Clarke M, Newburn-Cook C. Do women change their drinking behaviors while trying to conceive? An opportunity for preconception counseling. Clin Med Res 2006;4(2):97–105.
McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: The case of smoking cessation. Health Educ Res 2003;18(2):156–70.
Floyd RL, Rimer BK, Giovino GA, Mullen PD, Sullivan SE. A review of smoking in pregnancy: Effects on pregnancy outcomes and cessation efforts. Annu Rev Public Health 1993;14:379–411.
Autti-Ramo I, Korkman M, Hilakivi-Clarke L, Lehtonen M, Halmesmaki E, Granstrom ML. Mental health development of 2-year-old children exposed to alcohol in utero. J Pediatr 1992;120(5):740–46.
Floyd RL, O’Connor MJ, Bertrand J, Sokol R. Reducing adverse outcomes from prenatal alcohol exposure: A clinical plan of action. Alcohol Clin Exp Res 2006;30(8):1271–75.
Edwards N, Semenic S, Premji S, Montgomery P, Williams B, Olson J, Mansi O. Provincial prenatal record revision: A multiple case study of evidence-based decision-making at the population-policy level (protocol). BMC Health Serv Res 2008;8:266–77.
CMA Annual General Meeting Resolution (Confirmed — September 5, 2007). Available online at: http://www.cma.ca/index.cfm/ci_id/53612/la_id/1.htm (Accessed June 22, 2008).
Burnett M, Carrière S, Cox LV, Dell CA, Gammon H, Geller B, et al. Consensus report on the screening and recording of alcohol use among women of child bearing age and pregnant women [consensus report on the internet]; n.d. Available online at: http://www.google.ca/search?hl=en&sa=X&oi=spell&resnum=0&ct=result&cd=1&q=margaret+burnett+consensus+report&s pell=1 (Accessed May 22, 2008).
Alvik A, Heyerdahl S, Haldorsen T, Lindemann R. Alcohol use before and during pregnancy: A population-based study. Acta Obstet Gynecol 2006;85(11):1292–98.
Jacobson SW, Jacobson JL, Sokol RJ, Martier SS, Ager JW, Kaplan MG. Maternal recall of alcohol, cocaine, and marijuana use during pregnancy. Neuro-toxicol Teratol 1991;13(5):535–40.
Bradley K, Boyd-Wickizer J, Powell S, Burman M. Alcohol screening questionnaires in women: A critical review. JAMA 1998;280(2):166–71.
Offord DR, Craig DL. Primary Prevention of Fetal Alcohol Syndrome. Canadian Guide to Clinical Preventative Health Care. Ottawa: Health Canada, 1994.
Chang G. Alcohol-screening instruments for pregnant women. Alcohol Res Health 2001;25(3):204–9.
Chang G, Wilkins-Haug L, Berman S, Goetz MA. Brief intervention for alcohol use in pregnancy: A randomized trial. Addiction 1999;94(10):1499–508.
ACOG Committee on Ethics. At-risk drinking and illicit drug use: Ethical issues in obstetric and gynecologic practice. Obstet Gynecol 2004;103(5 Pt 1):1021–31.
May PA. Fetal alcohol effects among North American Indians. Alcohol Health Res World 1991;15(Summer):239–48.
Streissguth AP. Fetal alcohol syndrome: Understanding the problem; Understanding the solution; What Indian communities can do. American Indian Cult Res 1994;18:45–83.
Phelps L, Grabowski JA. Fetal alcohol syndrome: Diagnostic features and psychoeducational risk factors. School Psychology Q 1992;7:112–28.
Phelps L. Psychoeducational outcomes of fetal alcohol syndrome. School Psychology Rev 1995;24:200–12.
Day NL, Richardson GA. An analysis of the effects of prenatal exposure on growth: A teratologic model. Am J Med Genet C Semin Med Genet 2004;127(1):28–34.
Kerr WC, Greenfield TK, Tujague J, Brown SE. A drink is a drink? Variation in the amount of alcohol contained in beer, wine and spirit drinks in a US methodological sample. Alchol Clin Exp Res 2005;29(11):2015–21.
Martinez-Frias ML, Bermejo E, Rodriguez-Pinilla E, Frias JL. Risk for congenital anomalies associated with different sporadic and daily doses of alcohol consumption during pregnancy: A case-control study. Birth Defects Res Part A Clin Mol Teratol 2004;70(4):194–200.
Kaskutas LA, Graves K. Pre-pregnancy drinking: How drink size affects risk assessment. Addiction 2001;96(8):1199–209.
Streissguth AP, Sampson PD, Olson HC, Bookstein FL, Barr HM, Scott M, et al. Maternal drinking during pregnancy: Attention and short-term memory in 14-year-old offspring — A longitudinal prospective study. Alcohol Clin Exp Res 1994;18(1):202–18.
Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: Introducing the 4-digit diagnostic code. Alcohol 2000;35(4):400–10.
Henderson J, Gray R, Brocklehurst P. Systematic review of effects of low-moderate prenatal alcohol exposure on pregnancy outcome. BJOG 2007;114(3):243–52.
Larkby C, Day N. The effects of prenatal alcohol exposure. Alcohol Health Res World 1997;21(3):192–98.
Wilk AI, Jensen NM, Havinghurst TC. Meta-analysis of randomized control trials addressing brief intervention in heavy alcohol drinkers. J Gen Intern Med 1997;12(5):274–83.
Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment seeking populations. Addictions 2002;97(3):279–92.
Chang G, Goetz MA, Wilkins-Haug L, Berman S. A brief intervention for prenatal alcohol use: An in-depth look. J Subst Abuse Treat 2000;18(4):365–69.
Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: Results of a brief intervention trial. Alcohol Clin Exp Res 2000;24(10):1517–24.
O’Connor MJ, Whaley SE. Brief intervention for alcohol use by pregnant women. Am J Public Health 2007;97(2):252–58.
Halmesmaki E. Alcohol counselling of 85 pregnant problem drinkers: Effect on drinking and fetal outcome. Br J Obstet Gynaecol 1988;95(3):243–47.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Premji, S.S., Semenic, S. Do Canadian Prenatal Record Forms Integrate Evidence-based Guidelines for the Diagnosis of a FASD?. Can J Public Health 100, 274–280 (2009). https://doi.org/10.1007/BF03403946
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03403946
Keywords
- Fetal alcohol syndrome
- prenatal care
- evidence-based medicine
- practice guidelines
- prenatal exposure delayed effects