Abstract
Background
The optimal hematocrit (Hctopt) in hemodialysis (HD) patients has yet to be determined based on the etiology and complications of their endstage renal disease (ESRD). To investigate this problem, we compared regional cerebral oxygen supply (rCOS) in diabetic (DM group) and non-diabetic HD patients (non-DM group) with data from subjects without renal disease or DM (control group)
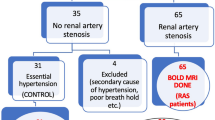
Methods
Regional cerebral blood flow (rCBF) was measured with single-photon emission computed tomography (SPECT) by the N-isopropyl-p-[123I]-iodoamphetamine (123I-IMP)-autoradiographic (ARG) method, and both the O2 content (O2CT) of arterial blood and hematocrit (Hct) were evaluated. Using the regression lines of rCBF vs Hct and O2CT vs Hct, we established a convex curve between rCOS and Hct. The peak of the curve indicates the maximum rCOS (rCOSmax) and Hctopt for rCOSmax
Results
The rCBF in both the DM and non-DM groups was lower than that of the control group at the same Hct level, and the DM group had the lowest values. The rCOSmax values in the DM and non-DM groups were nearly equal, but both were lower than in controls. The Hctopt in the DM group was lower than that in the non-DM group by 6.3%±3.3%
Conclusions
Although the difference in Hctopt values in the DM and non-DM groups was 6.3%, the rCOSmax values in both groups were nearly equal. This suggests that differences in the Hctopt may depend on complications or causes of ESRD. The optimal Hct in the DM group was 22.6%±1.9%, and that for the non-DM group was 29.0%±1.8%
Similar content being viewed by others
References
Besarab A, Bolton WK, Browne JK, Egrie JC, Nissenson AR, Okamoto DM, et al. The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 1998;339:584–90.
Brown WS, Marsh JT, Wolcott D, Takushi R, Carr CR, Higa J, et al. Cognitive function, mood and P3 latency: effects of the amelioration of anemia in dialysis patients. Neuropsychologia 1991;29:35–45.
Hirakata H, Kanai H, Fukuda K, Tsuruya K, Ishida I, Kubo M, et al. Optimal hematocrit for the maximum oxygen delivery to the brain with recombinant human erythropoietin in hemodialysis patients. Clin Nephrol 2000;53:354–61.
Metry G, Wikström B, Valind S, Sandhagen B, Linde T, Beshara S, et al. Effect of normalization of hematocrit on brain circulation and metabolism in hemodialysis patients. J Am Soc Nephrol 1999;10:854–63.
Lasen NA. Normal value of cerebral blood flow in younger adults is 50 ml/100 g/min. J Cereb Blood Flow Metab 1985;5:347–9.
Temple RM, Langan SJ, Deary IJ, Winney RJ. Recombinant erythropoietin improves cognitive function in chronic hemodialysis patients. Nephrol Dial Transplant 1992;7:240–5.
Eschbach JW, Glenny R, Robertson T. Normalizing the hematocrit (HCT) in hemodialysis patients (HDP) with EPO improves quality of life (Q/L) and is safe (abstract). J Am Soc Nephrol 1993;4:425.
Hint H. The pharmacology of dextran and the physiological background for the clinical use of Rheomacrodex and Macrodex. Acta Anaesthesiol Belg 1968;2:119–38.
Paganini EP. In search of an optimal hematocrit level in dialysis patients: rehabilitation and quality-of-life implications. Am J Kidney Dis 1994;24:S10–6.
The Working Group of the Japanese Ministry of Welfare. The guideline for the treatment for anemia due to chronic renal failure with recombinant human erythropoietin (in Japanese). Tokyo: Japanese Ministry of Welfare; 1989 (revised in 1991).
National Kidney Foundation (NKF) Anemia Work Group. NKFDOQI clinical practice guidelines for the treatment of anemia of chronic renal failure. Am J Kidney Dis 1997;30:S192–240.
Eschbach JW, Egrie JC, Downing MR, Browne JK, Adamson JW. Correction of the anemia of end-stage renal disease with recombinant human erythropoietin: results of a combined phase I and II clinical trial. N Engl J Med 1987;316:73–8.
Onoyama K, Kumagai H, Miishima T, Tsuruda H, Tomooka S, Motomura K. Incidence of strokes and its prognosis in patients on maintenance hemodialysis. Jpn Heart J 1986;27:685–91.
Standage BA, Schuman ES, Ackerman D, Gross GF, Ragsdale JW. Does the use of erythropoietin in hemodialysis patients increase dialysis graft thrombosis rates? Am J Surg 1993;165:650–4.
Valderrabano F. Adverse drug effects of recombinant erythropoietin (r-HuEPO) (abstract). Kidney Int 1989;35:265.
Statistical Survey Group of the Japanese Society for Dialysis Therapy. An overview of dialysis treatment in Japan (as of Dec. 31, 1998). J Jpn Soc Dial Ther 2000;33:1–27.
Rostand SG, Gretes JC, Kirk KA. Ischemic heart disease in patients with uremia undergoing maintenance hemo-dialysis. Kidney Int 1979;16:600–11.
Lindner A, Charra B, Sherrard DJ, Scribner BH. Acceleration of arteriosclerosis in prolonged maintenance hemodialysis. N Engl J Med 1974;290:697–701.
Castro L, Hofling B, Hassler R. Progression of coronary and valvular heart disease in patients on dialysis. Trans Am Soc Artif Intern Organs 1985;31:647–50.
Iida H, Itoh H, Nakazawa M, Hatazawa J, Nishimura H, Onishi Y, et al. Quantitative mapping of regional cerebral blood flow using Iodo-123-IMP and SPECT. J Nucl Med 1994;35:2019–30.
Komaba Y, Kitamura S, Terashi A. Effect of prostaglandin E1 on cerebral blood flow in patients with chronic cerebral infarction. Intern Med 1998;37:841–6.
Komaba Y, Osono E, Kitamura S, Katayama Y. Crossed cerebellocerebral diaschisis in patients with cerebellar stroke. Acta Neurol Scand 2000;101:8–12.
Hara S, Arizono K, Ubara Y. Risk factors for renal retardation of renal function in IDDM and NIDDM with nephropathy. J Diabetes Complications 1991;5:131–3.
Yamada N. Increased risk factors for coronary artery disease in Japanese subjects with hyperinsulinemia or glucose intolerance. Diabetes Care 1994;17:107–14.
Kee DB, Wood JH. Rheology of the cerebral circulation. Neurosurgery 1984;15:125–31.
Hirakata H, Yao H, Osato S, Ibayashi S, Onoyama K, Otsuka M. CBF and oxygen metabolism in hemodialysis patients: effects of anemia correction with recombinant human EPO. Am J Physiol 1992;262:F737–43.
Herold S, Brozovic M, Gibbs J, Lammertsma AA, Leenders KL, Carr D. Measurements of regional cerebral blood flow, blood volume and oxygen metabolism in patients with sickle cell disease using positron emission tomography. Stroke 1986;17:692–8.
Ishiwata A, Sakayori O, Kitamura S, Tsuganesawa T, Terashi A. Is brain circulation maintained sufficiently in chronic renal failure patients under hemodialysis treatment? J Cereb Blood Flow Metab 1997;17(suppl 1):S465.
Fan FC, Chen RYZ, Schuessler GB, Chien S. Effects of hematocrit variations on regional hemodynamics and oxygen transport in the dog. Am J Physiol 1980;238:H545–52.
Kusunoki M, Kimura K, Nakamura M, Isaka Y, Yoneda S, Abe H. Effects of hematocrit variations on cerebral blood flow and oxygen transport in ischemic cerebrovascular disease. J Cereb Blood Flow Metab 1981;1:413–7.
Jan KM, Chien S. Effect of hematocrit variation on coronary hemodynamics and oxygen utilization. Am J Physiol 1997;233:H106–13.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Oh, T., Sakayori, O., Kamano, C. et al. Optimal hematocrit based on regional cerebral blood flow in hemodialysis patients with diabetic nephropathy. Clin Exp Nephrol 6, 140–146 (2002). https://doi.org/10.1007/BF03353390
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03353390