Abstract
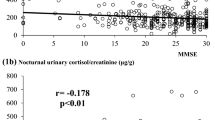
Convincing evidences has linked the hypothalamus-pituitary-adrenal (HPA) axis to aging patterns. F excess is implicated in the development of frailty characteristics whereas DHEAS is positively correlated to successful aging. We compared serum F and DHEAS levels of independent community- living (successful group, 19 M and 28 F, 69 to 87 yr) with those of institutionalized elderly (frail group, 20 M and 30 F, 65 to 95 yr). Serum F was determined at 1) baseline (08:00 h, 16:00 h and 23:00 h), 2) after 2 overnight dexamethasone (DEX) suppression tests (DST, using 0.25 and 1.0 mg doses), and 3) 60 min after ACTH stimulation (250 μg i.v. bolus); serum DHEAS was determined at 08:00 h. Basal serum F at 08:00 h, 16:00 h and 23:00 h and serum DHEAS levels were similar in both groups; however F: DHEAS ratio at 08:00 h was higher in the frail, compared to the successful group (mean±SD: 0.55±0.53 and 0.35±0.41, respectively; p=0.04). In response to DST, F suppression was less effective in frail elderly after either 0.25 or 1.0 mg doses (9.0±6.0 and 2.0±0.9 μg/dl), as compared to the successful group (5.8±4.4 and 1.5±0.5 μg/dl) (p=0.01). In addition, a significant correlation was observed between post- DEX F levels (both doses) and parameters of cognitive and physical frailty. Normal and similar F levels were observed after ACTH stimulation in both groups. Our data suggest a deficient feedback regulation of the HPA axis in frail institutionalized elderly, as demonstrated by a higher set point for F suppression. This augmented HPA tonus enforces the hypothesis that even milder F excess may be related to characteristics of frailty in the elderly.
Similar content being viewed by others
References
Rowe J.W., Kahn R.L. Human aging: usual and successful. Science. 1987, 237: 143–149.
Berkman L.F., Seeman T.E., Albert M., et al. High, usual and impaired functioning in community-dwelling older men and women: findings from the MacArthur Foundation Research Network on Successful Aging. J. Clin. Epidemiol. 1993, 46: 1129–1140.
De Kloet E.R., Vreugdenhil E., Oitzl M.S., Joëls M. Brain corticosteroid receptor balance in health and disease. Endocr. Rev. 1998, 19: 269–301.
Sapolsky R.M., Krey L.C., McEwen B.S. The neuroendocrinology of stress and aging: the glucocorticoid cascade hypothesis. Endocr. Rev. 1986, 7: 284–301.
Lupien S.J., Gaudreau S., Tchiteya B.M, et al. Stress-induced declarative memory impairment in healthy elderly subjects: relationship to cortisol reactivity. J. Clin. Endocrinol. Metab. 1997, 82: 2070–2075.
Lupien S.J., de Leon M., de Santi S., et al. Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat. Neurosci. 1998, 1: 69–73.
Dennison E., Hindmarsh P., Fall C., et al. Profiles of endogenous circulating cortisol and bone mineral density in healthy elderly men. J. Clin. Endocrinol. Metab. 1999, 84: 3058–3063.
Raff H., Raff J.L., Duthie E.H., et al. Elevated salivary cortisol in the evening in healthy elderly men and women: correlation with bone mineral density. J. Gerontol. Biol. Sci. Med. Sci. 1999, 54: M479–M483.
Greendale G.A., Unger J.B., Rowe J.W., Seeman T.E. The relation between cortisol excretion and fractures in healthy older people: results from the MacArthur studies-Mac. J. Am. Geriatr. Soc. 1999, 47: 799–803.
Braden B.J. The relationship between stress and pressure sore formation. Ostomy Wound Manage 1998, 44: 26S–36S.
Watson R.R., Huls A., Araghinikuam M., Chung S. Dehydroepiandrosterone and diseases of aging. Drugs Aging 1996, 9: 274–291.
Berr C., Lafont S., Debuire B., Dartigues J.F., Baulieu E.E. Relationships of dehydroepiandrosterone sulfate in the elderly with functional, psychological, and mental status, and short-term mortality: a French community-based study. Proc. Natl. Acad. Sci. U.S.A. 1996, 93: 13410–13415.
Rudman D., Shetty K.R., Mattson D.E. Plasma dehydroepiandrosterone sulfate in nursing home men. J. Am. Geriatr. Soc. 1990, 38: 421–427.
Ramos L.R., Toniolo J., Cendoroglo M.S., et al. Two-year follow-up study of elderly residents in São Paulo, Brazil: methodology and preliminary results. Rev. Saude Publica 1998, 32: 397–407.
Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12: 189–198.
Tombaugh T.N., McIntyre N.J. The mini-mental state examination: a comprehensive review. J. Am. Geriatr. Soc. 1992, 40: 922–935.
Gruenewald D.A., Matsumoto A.M. Aging of the endocrine system. In: Hazzard W.R., Blass J.P., Ettinger W.H. Jr., Halter J.B., Ouslander J.G. (Eds.), Principles of Geriatric Medicine and Gerontology. McGraw-Hill, New York, 1999, p. 949.
Carlson L.E., Sherwin B.B., Chertkow H.M. Relationships between dehydroepiandrosterone sulfate (DHEAS) and cortisol (CRT) plasma levels and everyday memory in Alzheimer’s disease patients compared to healthy controls. Horm. Behav. 1999, 35: 254–263.
Timiras P.S. Steroid-Secreting Endocrines: Adrenal, Ovary, Testis. In Timiras P.S., Quay W.D., Vernadakis A. (Eds.), Hormones and Aging. CRC Press, New York, 1995, p. 25.
Deuschle M., Gotthardt U., Schweiger U., et al. With aging in humans the activity of the hypothalamus-pituitaryadrenal system increases and its diurnal amplitude flattens. Life Sci. 1997, 61: 2239–2246.
Van Cauter E., Leproult R., Kupfer D.J. Effects of gender and age on the levels and circadian rhythmicity of plasma cortisol. J. Clin. Endocrinol. Metab. 1996, 81: 2468–2473.
Pavlov E.P., Harman S.M., Chrousos G.P., Loriaux D.L., Blackman M.R. Responses of plasma adrenocorticotropin, cortisol, and dehydroepiandrosterone to ovine corticotropin- releasing hormone in healthy aging men. J. Clin. Endocrinol. Metab. 1986, 62: 767–772.
Nicolson N., Storms C., Ponds R., Sulon J. Salivary cortisol levels and stress reactivity in human aging. J. Gerontol. Biol. Sci. Med. Sci. 1997, 52: M68–M75.
Greenspan S.L., Rowe J.W., Maitland L.A., McAloon-Dyke M., Elahi D. The pituitary-adrenal glucocorticoid response is altered by gender and disease. J. Gerontol. 1993, 48: M72–M77.
Uno H., Tarara R., Else J.G., Suleman M.A., Sapolsky R.M. Hippocampal damage associated with prolonged and fatal stress in primates. J. Neurosci. 1989, 9: 1705–1711.
Magarinos A.M., Verdugo J.M., McEwen B.S. Chronic stress alters synaptic terminal structure in hippocampus. Proc. Natl. Acad. Sci. U.S.A. 1997, 94: 14002–14008.
Landfield P.W., Waymire J.C., Lynch G. Hippocampal aging and adrenocorticoids: quantitative correlations. Science 1978, 202: 1098–1102.
Seeman T.E., McEwen B.S., Singer B.H., Albert M.S., Rowe J.W. Increase in urinary cortisol excretion and memory declines: MacArthur studies of successful aging. J. Clin. Endocrinol. Metab. 1997, 82: 2458–2465.
Keenan P.A., Jacobson M.W., Soleymani R.M., Mayes M.D.,Stress M.E., Yaldoo D.T. The effect on memory of chronic prednisone treatment in patients with systemic disease. Neurology 1996, 47: 1396–1402.
Wolkowitz O.M., Reus V.I., Canick J., Levin B., Lupien S. Glucocorticoid medication, memory and steroid psychosis in medical illness. Ann. N. Y. Acad. Sci. 1997, 823: 81–96.
Hatzinger M., Z’Brun A., Hemmeter U., et al. Hypothalamic- pituitary-adrenal system function in patients with Alzheimer’s disease. Neurobiol. Aging 1995, 16: 205–209.
O’Brien J.T., Schweitzer I., Ames D., Tuckwell V., Mastwyk M. Cortisol suppression by dexamethasone in the healthy elderly: effects of age, dexamethasone levels, and cognitive function. Biol. Psychiatry 1994, 36: 389–394.
Swanwick G.R., Kirby M., Bruce I., et al. Hypothalamic-pituitary- adrenal axis dysfunction in Alzheimer’s disease: lack of association between longitudinal and cross-sectional findings. Am. J. Psychiatry 1998, 155: 286–289.
Rosenbaum A.H., Schatzberg A.F., MacLaughlin R.A., et al. The dexamethasone suppression test in normal control subjects: comparison of two assays and effect of age. Am. J. Psychiatry 1984, 141: 1550–1555.
Georgotas A., McCue R.E., Kim O.M., et al. Dexamethasone suppression in dementia, depression, and normal aging. Am. J. Psychiatry 1986, 143: 452–456.
Weiner M.F., Davis B.M., Mohs R.C., Davis K.L. Influence of age and relative weight on cortisol suppression in normal subjects Am. J. Psychiatry 1987, 144: 646–649.
Tourigny-Rivard M.F., Raskind M., Rivard D. The dexamethasone suppression test in an elderly population. Biol. Psychiatry 1981, 16: 1177–1184.
Ansseau M., von Frenckell R., Simon C., Sulon J., Demey-Ponsart E., Franck G. Prediction of cortisol response to dexamethasone from age and basal cortisol in normal volunteers: a negative study. Psychopharmacology (Berl) 1986, 90: 276–277.
Huizenga N.A., Koper J.W., de Lange P. Interperson variability but intraperson stability of baseline plasma cortisol concentrations, and its relation to feedback sensitivity of the hypothalamo-pituitary-adrenal axis to a low dose of dexamethasone in elderly individuals. J. Clin. Endocrinol. Metab. 1998, 83: 47–54.
Weiner M.F. Age and cortisol suppression by dexamethasone in normal subjects. J Psychiatr. Res. 1989, 23: 163–168.
Meikle A.W. Dexamethasone suppression tests: usefulness of simultaneous measurement of plasma cortisol and dexamethasone. Clin. Endocrinol. (Oxf.) 1982, 16: 401–408.
O’Sullivan B.T., Hunt G.E., Johnson G.F., Caterson I.D. The plasma dexamethasone window: evidence supporting its usefulness to validate dexamethasone suppression test results. Biol. Psychiatry 1989, 25: 739–754.
Parmelee P.A., Katz I.R., Lawton M.P. Depression among institutionalized aged: assessment and prevalence estimation. J. Gerontol. 1989, 44: M22–M29.
Lewis D.A., Pfohl B., Schlechte J., Coryell W. Influence of age on the cortisol response to dexamethasone. Psychiatry Res. 1984, 13: 213–220.
Carroll B.J. Feinberg M. Greden J.F., et al. A specific laboratory test for the diagnosis of melancholia. Standardization, validation, and clinical utility. Arch. Gen. Psychiatry 1981, 38: 15–22.
Ohashi M., Kato K., Nawata H., Ibayashi H. Adrenocortical responsiveness to graded ACTH infusions in normal and elderly human subjects. Gerontology 1986, 32: 43–51.
Roberts N.A., Barton R.N., Horan M.A. Ageing and the sensitivity of the adrenal gland to physiological doses of ACTH in man. J. Endocrinol. 1990, 126: 507–513.
Waltman C., Blackman M.R., Chrousos G.P., Riemann C., Harman S.M. Spontaneous and glucocorticoid-inhibited adrenocorticotropic hormone and cortisol secretion are similar in healthy young and old men. J. Clin. Endocrinol. Metab. 1991, 73: 495–502.
Zumoff B., Rosenfeld R.S., Strain G.W., Levin J., Fukushima D.K. Sex differences in the twenty-four-hour plasma concentrations of dehydroisoandrosterone (DHA) and dehydroisoandrosterone sulphate (DHAS) and the DHA to DHAS ratio in normal adults. J. Clin. Endocrinol. Metab. 1980, 51: 330–333.
Orentreich N., Brind J.L., Rizer R.L., Vogelman J.H. Age changes and sex differences in serum dehydroepiandrosterone sulfate concentrations throughout adulthood. J. Clin. Endocrinol. Metab. 1984, 59: 551–555.
Barrett-Connor E., Edelstein S. A prospective study of dehydroepianrosterone sulphate and cognitive function in an older population: The Rancho Bernardo Study. J. Am. Geriatr. Soc. 1994, 42: 420–423.
Kalmijn S., Launer L.J., Stolk R.P., et al. A prospective study on cortisol, dehydroepiandrosterone sulfate and cognitive function in the elderly. J. Clin. Endocrinol. Metab. 1998, 83: 3487–3492.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carvalhaes-Neto, N., Huayllas, M.K., Ramos, L.R. et al. Cortisol, DHEAS and aging: Resistance to cortisol suppression in frail institutionalized elderly. J Endocrinol Invest 26, 17–22 (2003). https://doi.org/10.1007/BF03345117
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03345117