Abstract
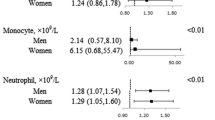
Background and aims: This study retrospectively examined the characteristics of metabolic syndrome in an aged population and assessed the risk factors for these subjects. Methods: A total of 1332 aged subjects (>-65 years; mean age 71.0±5.0 years) were enrolled from 6903 subjects recruited from the Department of Health Management at Chang Gung Medical Center. Of these 6903 subjects, 1665 (814 females and 851 males) were diagnosed with metabolic syndrome. Whole body three-dimensional (3-D) laser scanning was employed for anthropometric measurements. Furthermore, health index (HI) was derived by the following equation: HI = (body weight × 2 × waist area)/[body height2 × (breast area + hip area)]. Results: Among the 6903 subjects, no significant difference in gender was noted between groups with and without metabolic syndrome (p=0.142). For subjects >64 years, the incidence of metabolic syndrome in females is higher than in males. Subjects are categorized into four groups based on age and whether they had metabolic syndrome. Group A (4402 cases) consists of subjects <65 years old without metabolic syndrome. Group B (836 cases) comprises subjects >64 years old and without metabolic syndrome. Group C (1169 cases) contains subjects <65 years old with metabolic syndrome and group D (496 cases) is composed of subjects >64 years old with metabolic syndrome. Of the aged 1332 subjects, 595 were females (mean age, 70.6±4.6 years) and 737 were males (mean age, 71.3±5.3years), 37.2% (496/1332) had metabolic syndrome, 19.9% had DM and 21.8% had hypertension. These subjects had decreased BMI with age. Additionally, WHR peaked at an age range of 75–79 years. Of the aged subjects, also overweight, 42.8% and 33.6% were diagnosed with hypertension and DM, respectively; both ratios higher than those for non-overweight subjects (25.3% and 26.2%, respectively). Of the four groups in this study, the ratios for DM, hypertension, and WHR, HI, and LDL levels progressively increased through groups A to D. WBC count differs statistically significantly between these groups. Statistical analysis of WBC count, RBC and hemoglobin (Hb) with different parameters demonstrates significant elevation of WBC counts with the components of metabolic syndrome in aged subjects. Conclusions: WBC count, RBC count and Hb are associated with metabolic syndrome components in younger and old adults of both genders. The incidence of metabolic syndrome marker increased after menopause onset in the female population in this study.
Similar content being viewed by others
References
Wolk K, Larsson SC, Vessby B, Wolk A, Brismar K. Metabolic, anthropometric, and nutritional factors as predictors of circulating insulin-like growth factor binding protein-1 levels in middle-aged and elderly men. J Clin Endocrinol Metab 2004; 89: 1879–84.
Reaven GM, Lithell H, Landsberg L. Hypertension and associated metabolic abnormalities: the role of insulin resistance and the sympathoadrenal system. N Eng J Med 1996; 334: 374–81.
Garaulet M, Perex-Llamas F, Fuente T, Zamora S, Tebar FJ. Anthropometric, computed tomography and fat cell data in an obese population: relationship with insulin, leptin, tumor necrosis factor-alpha, sex hormone-binding globulin and sex hormones. Eur J Endocrinol 2000; 143: 657–66.
Modan M, Halkin H. Hyperinsulinemia or increased sympathetic drive as links for obesity and hypertension. Diabetes Care 1991; 14: 470–87.
Bao W, Srinivasanm SR, Wattifney WA, Berenson GS. Persistence of multiple cardiovascular risk clustering related to Syndrome X from childhood to young adulthood: The Bogalusa Heart Study. Arch Intern Med 1994; 154: 1842–7.
Chen W, Bao W, Begum S, Elkasabany A, Srinivasan SR, Berenson GS. Age-related patterns of the clustering of cardiovascular risk variables of syndrome X from childhood to young adulthood in population made up of black and white subjects: the Bogalusa Heart Study. Diabetes 2000; 49: 1042–8.
Meigs JB, D’Agostino RB Sr, Wilson PW, Cupples LA, Nathan DM, Singer DE. Risk variable clustering in the insulin resistance syndrome: The Framingham Offspring Study. Diabetes 1997; 46: 1594–600.
Mykkanen L, Haffner SM, Ronnemaa T, Bergman RN, Laakso M. Low insulin sensitivity is associated with clustering of cardiovascular disease risk factors. Am J Epidemiol 1997; 146: 315–21.
Holvoet P, Kritchevsky SB, Tracy RP, et al. The metabolic syndrome, circulating oxidized LDL, and risk of myocardial infarction in well-functioning elderly people in the health, aging, and body composition cohort. Diabetes 2004; 53: 1068–73.
Carantoni M, Zuliani G, Volpato S, et al. Relationships between fasting plasma insulin, anthropometries, and metabolic parameters in a very old healthy population. Associazione Medica Sabin. Metabolism 1998; 47:35–40.
Lin JD, Chiou WK, Weng HF, Tsai YH, Liu TH. Comparison of three-dimensional anthropometric body surface scanning with waist hip ratio and body mass index in correlation of metabolic risk factors. J Clin Epidemiol 2002; 55: 757–66.
Jones PRM, Baker AJ, Hardy CJ, Mowat AP. The Measurement of body surface area in children with liver disease by a novel 3D body scanning device. Eur J Appl Physiol 1994; 68: 514–8.
Lin JD, Chiou WK, Weng HF, Fang JT, Li TH. Application of three dimensional body scanner: Observation of prevalence of metabolic syndrome. Clin Nutr 2004; 23: 1313–23.
Laurier D, Guiguet M, Chau NP, Wells JA, Valleron AJ. Prevalence of obesity: a comparative survey in France, the United Kindom and the United States. Int J Obes Relat Metab Disord 1992; 16: 565–72.
Berenson GS, McMahan CA, Voors AW. Cardiovascular risk factors in children: the early natural history of atherosclerosis and essential hypertension. New York. NY: Oxford University Press. 1980.
Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem 1974; 20: 470–5.
Rawlins ML, Roberts WL. Performance characteristics of six third-generation assays for thyroid-stimulating hormone. Clin Chem 2004; 50: 2338–44.
Fraisse L, Bonnet MC, de Farcy JP, Agut C, Dersigny D, Bayol A. A colorimetric 96-well microtiter plate assay for the determination of urate oxidase activity and its kinetic parameters. Anal Biochem 2002; 309: 173–9.
Nakamura K, Motohashi Y, Kikuchi S, Tanaka M, Nakano S. Liver transferase activity in health Japanese employees aged 18–39 years. Ind Health 1998; 36: 218–22.
Daanen HAM, van de Water GJ. Whole body scanners. Displays 1998; 19:111–20.
SAS Institute. Inc. SAS/STAT user’s guide, version 6.4th ed. Cary, NC: SAS Institute, Inc, 1990.
Lee WY, Park JS, Noh Sy, Rhee EJ, Kim SW, Zimmet PZ. Prevalence of the metabolic syndrome among 40,698 Korean metropolitan. Diabetes Res Clin Pract 2004; 65: 143–9.
Jehn M, Clark JM, Guallar E. Serum ferritin and risk of the metabolic syndrome in U.S. adults. Diabetes Care 2004; 27: 2422–8.
Ilanne-Parikka P, Eriksson JG, Lindstrom J, et al. Finnish Diabetes Prevention Study Group. Prevalence of the metabolic syndrome and its components: findings from a Finnish general population sample and the Diabetes Prevention Study cohort. Diabetes Care 2004; 27: 2135–40.
Fuh JL, Wang SJ, Lu SR, Juang KD, Chiu LM. The Kinmen women-health investigation (KIWI): a menopausal study of a population aged 40–54. Maturitas 2001; 39: 117–24.
Tsai WL, Yang CY, Lin SF, Fang FM. Impact of obesity on medical problems and quality of life in Taiwan. Am J Epidemiol 2004; 160: 557–65.
Aso Y, Wakabayashi S, Yamamoto R, Matsutomo R, Take-bayashi K, Inukai T. Metabolic syndrome accompanied by hypercholesterolemia is strongly associated with proinflammotory state and impairment of fibrinolysis in patients with type 2 diabetes: synergistic effects of plasminogen activator inhibitor-1 and thrombin-activatable fibrinolysis inhibitor. Diabetes Care 2005; 28:2211–6.
Han SH, Quon MJ, Koh KK. Beneficial vascular and metabolic effects of peroxisome proliferators-activated receptor-alpha activators. Hypertension 2005; 46: 1086–92.
Targher G, Scidell JC, Tonoli M, Muggeo M, De Sandre G, Cigolini M. The white blood cell count: its relationship to plasma insulin and other cardiovascular risk factors in healthy male individuals. J Intern Med 1996; 239: 435–41.
Ble A, Palmieri E, Volpato S, Costantini F, Fellin R, Zuliani G. White blood cell count is associated with some features of metabolic syndrome in a very old population. Nutr Metab Cardiovasc Dis 2001; 11: 221–6.
Choi KM, Lee J, Kim YH, et al. Relation between insulin resistance and hematological parameters in elderly Koreans-Southwest Seoul (SWS) Study. Diabetes Res Clin Pract 2003; 60: 205–12.
Ohshita K, Yamane K, Hanafusa M et al. Elevated white blood cell count in subjects with impaired glucose tolerance. Diabetes Care 2004; 27: 491–6.
Choi KM, Lee J, Lee KW, et al. Comparison of serum concentrations of C-reactive protein, TNF-alpha, and interleukin 6 between elderly Korean women with normal and impaired glucose tolerance. Diabetes Res Clin Pract 2004; 64: 99–106.
Perrine SP, Greene MF, Lee PD, Cohen RA, Faller DV. Insulin stimulates cord blood erythroid progenitor growth: evidence for an aetiological role in neonatal polycythaemia. Br J Haematol 1986; 64: 503–11.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Un, JD., Chiou, WK., Chang, HY. et al. Association of hematological factors with components of the metabolic syndrome in older and younger adults. Aging Clin Exp Res 18, 477–484 (2006). https://doi.org/10.1007/BF03324847
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03324847