Abstract
Objectives
This study sought to determine the effects of grafting the internal thoracic artery (ITA) to the left anterior descending coronary artery (LAD) on long-term (10-year) survival, the cardiac death-free rate, and on the cardiac event-free rate in Japanese patients.
Background
The use of ITA grafts has been reported to enhance postoperative survival and to decrease the occurrence of cardiac events in the Western literature. However, the survival benefits in Japanese patients, who may have different prognoses with coronary artery disease and a different fate of a saphenous vein graft, have not yet been determined.
Subjects and Methods
A total of 954 consecutive patients who underwent coronary artery bypass graft operations (CABG) during the last 12 years at the Nara Medical University were followed and evaluated. Of these, 713 patients underwent ITA-CABG to at least the LAD (ITA group), and 241 patients received a saphenous vein graft (SVG) to the LAD (SVG group). At the time of operation, no significant difference was found between these two groups in age, sex ratio, left ventricular ejection fraction, left ventricular end-diastolic pressure, cardiac index, incidence of unstable angina, or in the necessity for an emergency operation. However, those patients who received ITA-CABG had significantly higher incidences of diabetes mellitus, hyperlipidemia, and left main coronary artery disease.
Results
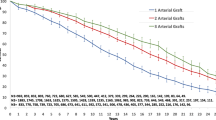
The 10-year cumulative graft patency rate for the LAD was 23% higher in the ITA group (90.3%) compared to the SVG group (67.0%), (p<.0001). Despite increased preoperative risk factors, patients in the ITA group showed significant improvements in their 5- and 10-year cumulative survival rates as well as in their cardiac death-free and event-free rates. Furthermore, this study demonstrated that ITA grafts improved the prognoses of patients with diabetes mellitus or left ventricular dysfunction and lowered both the long-term postoperative cardiac-death rate and the cardiac-event rate.
Conclusions
The use of ITA grafts was effective in improving both the postoperative survival and cardiac event-free rates, and should be recommended in patients with diabetes mellitus or left ventricular dysfunction. ITA grafting to the LAD should be a routine operation in almost all categories of such patients.
Similar content being viewed by others
References
Grondin CM, Campeau L, Lesperance J, Enjalbert M, Bourassa MG. Comparison of late changes in internal mammary artery and saphenous vein grafts in two consecutive series of patients 10 years after operation. Circulation 1984; 70 (Suppl I) 208–12.
Lytle BW, Loop FD, Cosgrove DM, Ratiff NB, Easley K, Taylor PC, et al. Long-term (5 to 12 years) serial studies of internal mammary artery and saphenous vein coronary bypass grafts. J Thorac Cardiovasc Surg 1985; 89: 248–58.
Loop FD, Lytle BM, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, et al. Influence of the internal mammary artery grafts on 10-year-survival and other cardiac events. N Engl J Med 1986; 314: 1–6.
Okies JE, Page US, Bigelow JC, Krause AH, Salomon NW. The internal mammary artery: the graft of choice. Circulation 1984; 70 (Suppl I):213–21.
Zeff RH, Kongtahworn C, Iannon LA, Gordon DF, Brown TM, Phillips SJ, et al. Internal mammary artery versus saphenous vein graft to the left anterior descending coronary artery: prospective randomized study with 10-year follow-up. Ann Thorac Surg 1988; 45: 533–6.
Lytle BW, Loop FD, Taylor PC, Simpferdorfer C, Kramer JR, Batliff NB, et al. Vein graft disease: the clinical impact of stenoses in saphenous vein bypass grafts to coronary arteries. J Thorac Cardiovasc Surg 1992; 103: 831–40.
Cameron AAC, Green GE, Brongo DA, Thornton J. Internal thoracic artery grafts: 20-year clinical follow-up. J Am Coll Cardiol 1995; 25:188–92.
Nakamura Y, Kinoshita M, Kawai C, the Multicenter Study of Myocardial Ischemia Research Group. Coronary artery disease in Japan as compared with that in North America, clinical characteristics, medical treatment and program (in Japanese). J Jpn Coll Angiol 1995; 35: 999–1002.
Horii T, Suma H, Wanibuchi Y, Fukuda S, Kigawa I. The long-term patency rate of saphenous vein grafts and vein graft disease in Japanese patients (in Japanese). J Jpn Ass Thorac Surg 1993; 41: 1447–51.
Hosoda Y, Nukariya M, Watanabe M, Sasaguri S, Kazui M, Watanabe T, et al. Late results of coronary artery bypass surgery with maximal follow-up of 7 years. Analysis of determinants affecting late survival. Cardiovasc Surg 1993; 1:403–9.
Lowry PJ, Glover DR, Mace PJE, Littler WA. Coronary artery disease in Asians in Birmingham. Brit Heart J 1984; 52:610–3.
Boylan MJ, Lytle BW, Loop FD, Taylor PC, Borsh JA, Goormastic M, et al. Surgical treatment of isolated left anterior stenosis. J Thorac Cardiovasc Surg 1994; 107:657–62.
Kobayashi H, Kitamura S, Kawachi K, Morita R, Konishi Y, Tsutsumi M. A pathohistological and biochemical study of arteriosclerosis in the internal thoracic artery, a vessel commonly used as a graft in coronary artery bypass surgery. Surg Today 1993; 23:697–703.
Sims FH. A comparison of coronary and internal mammary arteries and implications of the results in the etiology of arteriosclerosis. Am Heart J 1983; 105: 560–6.
Pearson PJ, Evora PR, Schaff HV. Bioassay of EDRF from internal mammary arteries. Implications for early and late bypass graft patency. Ann Thorac Surg 1992; 54:1078–84.
Singh RN, Beg RA, Kay EB. Physiological adaptability: the secret of success of the internal mammary artery graft. Ann Thorac Surg 1986; 41:247–50.
Kitamura S, Seki T, Kawachi K, Morita R, Kawata T, Mizuguchi K, et al. Excellent patency and growth potential of internal mammary artery grafts in pediatric coronary artery bypass surgery. New evidence for a “live” conduit. Circulation 1988; 78 (Suppl 1) 129–39.
Morita R, Kitamura S, Kawachi K, Kawata T, Mizuguchi K, Kameda Y, et al. Exercise coronary flow reserve of bilateral internal thoracic artery bypass grafts. Ann Thorac Surg 1993; 55:883–7.
Seki T, Kitamura S, Kawachi K, Morita R, Kawata T, Mizuguchi K, et al. A quantitative study of postoperative luminal narrowing of the internal thoracic artery graft in coronary artery bypass surgery. J Thorac Cardiovasc Surg 1992; 104:1532–8.
Jones EL, Lutz JF, King SB, Powelson S, Knopf W. Extended use of the internal mammary artery graft. Important anatomic and physiological considerations. Circulation 1986; 74 (Suppl III): 42–7.
Chesebro JH, Fuster V. Drug trials in prevention of occlusion of aortocoronary artery vein grafts. J Thorac Cardiovasc Surg 1982; 83:90–3.
Blankenhorn DH, Nessim SA, Johnson RL, Sanmarco ME, Azen SP, Cashin-Hemphill L. Beneficial effects of combined colestipolniacin therapy on coronary atherosclerosis and venous bypass grafts. JAMA 1987; 257:3233–40.
Engblom E, Ronnemaa T, Hamalainen H, Kallio V, Vanttinen E, Knuts LR. Coronary heart disease risk factors before and after bypass surgery. Results of a controlled trial on multifactorial rehabilitation. Eur Heart J 1992; 13:232–7.
Solymoss BC, Nadeau P, Millette D, Campeau L. Late thrombosis of saphenous vein coronary bypass grafts related to risk factors. Circulation 1988; 78 (Suppl I): 140–3.
Mock MB, Ringovist I, Fisher LD, Davis KB, Chaitman BR, Kouchoukos NT, et al. Survival of medically treated patients in the coronary artery surgery study (CASS) registry. Circulation 1982; 66: 562–8.
Elefteriades JA, Tolis G Jr, Levi E, Mills LK, Zaret BL. Coronary artery bypass grafting in severe left ventricular dysfunction and functional state. J Am Coll Cardiol 1993; 22: 1411–7.
Pigott JD, Kouchoukos NT, Oberman A, Cutter GR. Late results of surgical and medical therapy for patients with coronary artery disease and depressed left ventricular function. J Am Coll Cardiol 1985; 5:1036–45.
Smith LR, Harrell FE Jr, Rankin JS, Califf RM, Pryor DB, Muhlbaier LH, et al. Determinants of early versus late cardiac death in patients undergoing coronary artery bypass graft surgery. Circulation 1991; 84(Suppl III): 245–53.
Edwards FH, Clark RE, Schwartz M. Impact of internal mammary artery conduit on operative mortality in coronary revascularization. Ann Thorac Surg 1994; 57: 27–32.
Barzilay JI, Kronmal RA, Bittner V, Eaker E, Evans C, Foster ED. Coronary artery disease and coronary artery bypass grafting in diabetic patients aged ≧65 years (Report from the CASS Registry) 1994;74:334–9.
Aronson D, Bloomgarden Z, Rayfield EJ. Potential mechanisms promoting restenosis in diabetic patients. J Am Coll Cardiol 1996; 27: 528–35.
Cosgrove DM, Lytle BW, Loop FD, Taylor PC, Stewart RW, Gill CC, et al. Does bilateral internal mammary artery grafting increase surgical risk? J Thorac Cardiovasc Surg 1988; 95:850–6.
Berreklouw E, Schonberger JP, Ercan H, Koldewijn EL, de Bock M, Verwaal VJ, et al. Does it make sense to use two internal thoracic arteries? Ann Thorac Surg 1995; 59:1456–63.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kitamura, S., Kawachi, K., Taniguchi, S. et al. Long-term benefits of internal thoracic artery-coronary artery bypass in Japanese patients. Jpn J Thorac Caridovasc Surg 46, 1–10 (1998). https://doi.org/10.1007/BF03217715
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03217715