Summary
Objective
To determine the effect and side effects of intravitreal rTPA in eyes with submacular hemorrhage.
Method
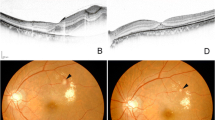
28 eyes with a history of sudden visual loss between 1 day and 4 weeks were included in the study. They received 50μ rTPA and 0.3–0.5cc SF6 intravitreally. Preand postoperatively functional, biomicroscopical, and echographical results were compared. The follow up period was 12 months.
Results
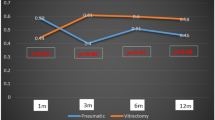
Mean visual acuity was 20/376 preoperatively (range LP to 20/25), 12/28 patients (43%) had quantitative function. One week after surgery mean visual acuity improved to 20/325 (LP to 20/25) and only 4/28 patients (14%) showed quantitative function. At the final examination mean visual acuity decreased to 20/428 and the number of eyes with quantitative vision increased to 9/28 (32%). 12 eyes (43%) showed a final functional benefit after the treatment.
5 eyes (17.8%) developed a severe recurrent hemorrhage. In 3 of those a correlation to partial or total vitreous separation cannot be excluded. One eye showed an inferior retinal detachment 6 weeks postoperatively potentially induced by a complete vitreous separation.
Conclusion
The removal of submacular hemorrhage by intravitreal rTPA is a minimal invasive surgery. The postoperative success rate of 50% visual improvement is statistically significant to preoperative values but the final results are worse than the results immediately after surgery. The effect seems to be temporary especially in cases where the underlying AMD in not treatable.
Zusammenfassung
In der vorliegenden Studie werden die Wirkung und Nebenwirkungen von intravitralen RTPA in Augen mit submakulärer Blutung untersucht.
Methode
28 Augen mit plötzlichem Sehverlust von 1 Tag bis 4 Wochen wurden in die Studie aufgenommen. Sie erhielten eine intravitreale Injektion mit 50μ rTPA und 0,3–0,5 ccSF6 Prä- und postoperativ wurden die funktioneilen, biomikroskopischen und echographischen Ergebnisse verglichen. Die Nachbeobachtungszeit betrug 1 Jahr.
Ergebnisse
Das mittlere Sehvermögen betrug präoperativ 20/376 (von LP bis 20/25), 12 von 28 Patienten (43%) hatten nur ein quantitatives Sehen (LP bis FZ). Eine Woche postoperativ verbesserte sich das durchschnittliche Sehvermögen auf 20/325 (LP bis 20/25) und nur 4 von 28 Patienten (14%) gaben ein quantitatives Sehen an. Bei der letzten Kontrolle sank der Visus im Durchschnitt auf 20/428 und die Zahl der Augen mit quantitativer Funktion stieg auf 9 von 28 (32%).
12 Patienten (43%) hatten zu diesem Zeitpunkt eine bessere Funktion als präoperativ.
In 5 Augen (17,8%) trat eine schwere Nachblutung auf; in 3 Fällen stand diese im zeitlichen Zusammenhang mit einer hinteren Glaskörperabhebung. Ein Patient entwickelte eine Netzhautabhebung in der unteren Hälfte 6 Wochen postoperativ, die möglicherweise auch durch eine Glaskörperabhebung induziert wurde.
Schlussfolgerung
Die Verdrängung von submakulären Blutungen durch intravitreales rTPA und Gas ist ein minimal-invasiver Eingriff. Die postoperative Visusverbesserung in 50% der Fälle ist statistisch signifikant. Die Ergebnisse am Ende der Nachbeobachtungszeit sind jedoch deutlich schlechter als die nach 1 Woche erhobenen. Der Effekt scheint eine vorübergehende Verbesserung zu bewirken besonders in Fällen, in denen die darunterliegende Pathologie nicht behandelbar ist.
Similar content being viewed by others
References
Scupola A, Coscas G, Soubrane G, Balestrazzi E (1999) Natural history of macular subretinal hemorrhage in age-related macular degeneration. Ophthalmologica 213: 97–102
Avery RL, Fekrat S, Hawkins BS, Bressler NM (1996) Natural history of subfoveal hemorrhage in age-related macular degeneration. Retina 16: 183–189
Bennett SR, Blodi CF, Folk JC et al (1990) Prognostic factors of visual outcome in patients with subretinal hemorrhage involving the fovea. Am J Ophthalmol 109: 33–37
Glatt H, Machemer R (1982) Experimental subretinal hemorrhage in rabbits. Am J Ophthalmol 94: 762–772
Benner JD, Hay A, Landers MB 3rd, Hjelmeland LM, Morse LS (1994) Fibrinolytic-assisted removal of experimental subretinal hemorrhage within seven days reduces outer retinal degeneration. Ophthalmology 101: 672–681
Toth CA, Morse LA, Hjelmeland LM, Landers MB 3rd (1991) Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch Ophthalmol 109: 723–729
Berrocal MH, Lewis ML, Flynn HW et al (1996) Variations in the clinical course of submacular hemorrhage. Am J Ophthalmol 122:486–493
El Baba F, Jarrett WH II, Harbin TS et al (1986) Massive hemorrhage complicating age-related macular degeneration. Ophtalmology 93: 1581–1592
Lewis H, Sloan SH, Foos RY (1988) Massive intraocular hemorrhage associated with anticoagulation and age-related macular degeneration. Graefe’s Arch Clin Exp Ophthalmol 226: 59–64
Tani PM, Buettner H, Robertson DM (1980) Massive vitreous hemorrhage and senile macular choroidal degeneration. Am J Ophthalmol 90: 525–533
deJuan E Jr, Machemer R (1988) Vitreous surgery for hemorrhagic and fibrous complications of age-related macular degeneration. Am J Ophthalmol 105: 25–29
Dellaporta AN (1994) Evacuation of subretinal hemorrhage. Int Ophthalmol 18: 25–31
Hanscom TA, Diddie KR (1987) Early surgical drainage of macular subretinal hemorrhage. Arch Ophthalmol 105: 1722–1723
Wade EC, Flynn HW Jr, Olsen KR et al (1990) Subretinal hemorrhage management by pars plana vitrectomy and internal drainage. Arch Ophthalmol 108: 973–978
Vander JF, Federman JL, Greven C (1991) Surgical removal of massive subretinal hemorrhage associated with age-related macular degeneration. Ophthalmology 98: 23–27
Ibanez HE, Williams DF, Thomas MA (1995) Surgical management of submacular hemorrhage. Arch Ophthalmol 113: 62–69
Hesse L, Meitinger D, Schmidt J (1996) Little effect of tissue plasminogen activator in subretinal surgery for acute hemorrhage in age-related macular degeneration. Ger J Ophthalmol 5: 479–483
Heriot W (1996) Intravitreal gas and TPA: an outpatient procedure for subretinal hemorrhage. Vail Vitrectomy Meeting March 10–15, 1996, Vail, Collorado.
Verstraeten TC, Chapman C, Hartzer M, Winkler BS, Trese MT, Williams GA (1993) Pharmacologic induction of posterior vitreous detachment in the rabbit. Arch Ophthalmol 111: 849–854
Hesse L, Kroll P (1999) Enzymatically induced posterior vitreous detachment in proliferative diabetic retinopathy. Klin Monatsbl Augenheilkd 214: 84–89
Johnson MW, Olsen KR, Hernandez E (1991) Tissue plasminogen activator treatment of experimental subretinal hemorrhage. Retina 11: 250–258
Hayasaka S, Uchida M, Setogaure T et al (1990) Subretinal hemorrhages with or without choroidal neovascularization in the maculas of patients with pathologic myopia. Graefe’s Arch Clin Exp Ophthalmol 228: 277–280
Johnson MW, Olsen KR, Hernandez E (1992) Tissue plasminogen activator thrombolysis during surgical evacuation of experimental subretinal hemorrhage. Ophthalmology 99: 515–521
Lewis H, Resnick SC, Flannery JG, Straatsma BR (1991) Tissue plasminogen activator treatment of experimental subretinal hemorrhage. Am J Ophthalmol 111/2: 197–204
Toth CA, Benner JD, Hjelmeland LM, Landers MB 3rd, Morse LS (1992) Ultramicrosurgical removal of subretinal hemorrhage in cats. Am J Ophthalmol 113: 175–182
Boone DE, Boldt HC, Ross RD, Folk JC, Kimura AE (1996) The use of intravitreal tissue plasminogen activator in the treatment of experimental subretinal hemorrhage in the pig model. Retina 16: 518–524
Lewis H (1994) Intraoperative fibrinolysis of submacular hemorrhage with tissue plasminogen activator and surgical drainage. Am J Ophthalmol 118: 559–568
Moriarty AP, McAllister IL, Constable IJ (1995) Initial clinical experience with tissue plasminogen activator (tPA) assisted removal of submacular hemorrhage. Eye 9: 582–588
Kamei M, Tano Y, Maeno T, Ikuno Y, Mitsuda H, Yuasa T (1996) Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol 121:267–275
Lim JI, Drews Botsch C, Sternberg P Jr, Capone A Jr, Aaberg TM (1995) Submacular hemorrhage removal. Ophthalmology 102: 1393–1399
Peyman GA, Nelson NC Jr, Alturki W et al (1991) Tissue plasminogen activating factor assisted removal of subretinal hemorrhage. Ophtalmic Surg 22: 575–582
Saika S, Kawashima A, Minamide A et al (1988) Subretinal administration of t-type plasminogen activator to speed the drainage of subretinal hemorrhage. Graefe’s Arch Clin Exp Ophthalmol 236: 196–201
Humayun M, Lewis H, Flynn HW Jr, Sternberg P Jr, Blumenkranz MS (1998) Management of submacular hemorrhage associated with retinal arterial macroaneurysms. Am J Ophthalmol 126: 358–361
Steinhorst UH, Theischen M, Winter R (1997) Subretinal lavage: a technique of continuous subretinal irrigation for removal of traumatic submacular hemorrhage. Ophthalmologica 211: 399–401
Shariga F, Matsuo T, Yokoe S et al (1999) Surgical treatment of submacular hemorrhage associated with idiopathic polypoidal choroidal vasculopathy. Am J Ophthalmol 128: 147–154
Marmor MF, Negi A, Maurice DM (1985) Kinetics of macro-molecules injected into the subretinal space. Exp Eye Res 40: 687–696
Takeuchi A, Kricorian G, Yao Y, Kenny JW, Marmor MF (1994) The rate and source of albumin entry into saline-filled experimental retinal detachment. Invest Ophthalmol Vis Sci 35: 3792–3798
Jaffe GJ, Green GDJ, McKay BS, Hartz A, Williams GA (1988) Intravitreal clearance of tissue planimogen activator in the rabbit. Arch Ophthalmol 106: 969–972
Raviola G, Bulter JM (1983) Unidirectional vesicular transport mechanism in retinal vessels. Invest Ophthalmol Vis Sci 24: 1465–1474
Heriot WJ (1997) Further experience in management of submacular hemorrhage with intravitreal TPA. Vitreoretinal Update on Macular Surgery, October 24–25, 1997, San Francisco
Hesse L, Schmidt J, Kroll P (1999) Management of acute submacular hemorrhage using recombinant tissue plasminogen activator and gas. Graefe’s Arch Clin Exp Ophthalmol 237: 273–277
Johnson MW, Olsen KR, Hernandez E, Irvine WD, Johnson RN (1990) Retinal toxicity of recombinant tissue plasminogen activator in the rabbit. Arch Ophthalmol 108: 259–263
Irvine WD, Johnson MW, Hernandez E, Olsen KR (1991) Retinal toxicity of human tissue plasminogen activator in vitrectomized rabbit eyes. Arch Ophthalmol 109: 718–722
Lewis H, Resnick SC, Flannery JG, Straatsma BR (1991) Tissue plasminogen activator treatment of experimental subretinal hemorrhage. Am J Ophthalmol 111: 197–204
Ohji M, Saito Y, Hayashi A, Lewis JM, Tano Y (1998) Pneumatic displacement of subretinal hemorrhage without tissue plasminogen activator. Arch Ophthalmol 116: 1326–1332
Coscas G, Soubrane G (1991) Perifoveal laser photocoagulation of subfoveal neovascular lesions in age-related macular degeneration. Results of a randomized clinical trial. Arch Ophthalmol 109: 1115–1121
Macular Photocoagulation Study Group (1991) Laser photocoagulation of subfoveal neovascular lesions in age-related macular degeneration: results of a randomized clinical trial. Arch Ophthalmol 109: 1220–1231
Macular Photocoagulation Study Group (1994) Visual outcome after laser photocoagulation for subfoveal choroidal neovascularization secondary to age-related macular degeneration. Arch Ophthalmol 112:480–488
Arnold J, Algan M, Soubrane G, Coscas G, Barreau E (1997) Indirect scatter laser photocoagulation to subfoveal choroidal neovascularization in age-related macular degeneration. Graefe’s Arch Clin Exp Ophthalmol 235: 208–216
Bressler NM, Maguire MG, Murphy PL et al (1996) Macular scatter („grid“) laser treatment of poorly demarcated subfoveal choroidal neovascularization in age-related macular degeneration. Results of a randomized pilot trial. Arch Ophthalmol 114: 1456–1464
Bressler NM, Frost L, Bressler SB, Fine SL (1988) Natural course of poorly defined choroidal neovascularization in macular degeneration. Arch Ophthalmol 106: 1537–1543
Poliner LS, Olk RJ, Burgess D, Gordon ME (1986) Natural history of retinal pigment epithelial detachments in age-related macular degeneration. Ophthalmology 93: 543–551
Favre M, Goldmann H (1956) Zur Genese der hinteren Glaskörperabhebung. Ophthalmologica 132: 87–90
Lambert HM, Capone A, Aaberg TA, Sternberg P, Mandell BA, Lopez PF (1992) Surgical excision of subfoveal neovascular membranes in age-related macular degeneration. Am J Ophthalmol 113: 257–262
Worst JGF, Los LI (2000) Cisternal anatomy of the vitreous. Kluger Publications, Amsterdam, New York (in press)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Stolba, U., Binder, S., Krebs, I. et al. Short and long term effect of intravitreal tissue plasminogen activator in eyes with submacular hemorrhage. Spektrum Augeheilkd 14, 262–267 (2000). https://doi.org/10.1007/BF03162829
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03162829