Abstract
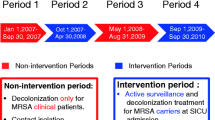
Objectives: Methicillin-resistant Staphylococcus aureus (MRSA) continues to pose a major threat to the lung and cardiovascular surgery patients. We propose evidence-based infection control (EBIC) against MRSA.Methods: We conducted a basic study comparing genotyping to cluster analysis using minimal inhibition concentration on 17 drugs for 21 MRSA strains. With or without EBIC using cluster analysis and global evidence, we compared the incidence of postoperative MRSA infection. Notably, we eliminated tweezers stands and emesis basins.Results: Cluster analysis showed a typing sensitivity of 72%. The use of EBIC decreased MRSA cross-infection in the recovery room. A lung surgery series showed an MRSA incidence of 1/190 before and 0/200 after EBIC was introduced. For a cardiovascular surgery series, the MRSA incidence was 2/169 before and 0/84 after EBIC was introduced. Across wards, MRSA among Staphylococcus aureus in patient fell from 68% in 1999 to 57% in 2000.Conclusions: EBIC consisting of global guidelines and cluster analysis was useful in controlling MRSA in lung and cardiovascular surgery patients.
Similar content being viewed by others
References
Centers for Disease Control and Prevention, US Government. Guidelines for the Prevention of Surgical Site Infection. 1999; 1–32. To download, access http:// www.cdc.gov/ncidod/hip/SSI/SSI.pdf for the original paper and http://www.lamen.or.jp/lib/kansen/saiseikai_ dl3.html for the Japanese translation.)
Yoshida J, Nagata T, Nishioka Y, Nose Y, Tanaka M. Outbreak of multidrug resistant Staphylococcus aureus: a cluster analysis. J Clin Epidemiol 1996; 49: 1447–52.
Yoshida J, Kondo H, Akao M.. Computerized antibiogram for methicillin-resistant Staphylococcus aureus in chest surgery. Jpn J Thorac Cardiovasc Surg 1999; 47: 368–76.
Yoshida J, Ishimaru T, Kawano S, Akao M. An electronic system combining MIC2000 (TM) and antibiogram cluster analysis for surveillance of methicillin-resistant Staphylococcus aureus in hospitals. Jpn J Infect Dis 2000; 53: 79–81.
Yoshida J, Umeda A, Ishimaru T, Akao M. Cluster analysis on multiple drugs susceptibility supplements genotyping of methicillin-resistant Staphylococcus aureus. Int J Infect Dis 2001; 5: 205–208.
Murphy CL, McLaws M. Australian Infection Control Association members’ use of skills and resources that promote evidence-based infection control. Am J Infect Control 2000; 28: 116–22.
Jenner EA, Mackintosh C, Scott GM. Infection control-evidence into practice. J Hosp Infect 1999; 42: 91–104.
Prevost G, Jaulhac B, Piemont Y. DNA fingerprinting by pulsed-field gel electrophoresis is more effective than ribotyping in distinguishing among methicillin-resistant Staphylococcus aureus isolates. J Clin Microbiol 1992; 30: 967–73.
Ichiyama S, Ohta M, Shinokata K, Kato N, Takeuchi J. Genomic DNA figerprintings by pulsed-field gel electrophoresis as an epidemiological marker for study of nosocomial infections caused by methicillin-resistant Staphylococcus aureus. J Clin Microbiol 1991; 29: 2690–5.
Weightman NC, Banfield KR. Protective overshoes are unnecessary in a day surgery unit. J Hosp Infec 1994; 28: 1–3.
Blanc DS, Petignat C, Moreillon P, Wenger A, Bille J, Francioli P. Quantitative antibiogram as a typing method for the prospective epidemiological surveillance and control of MRSA: comparison with molecular typing. Infect Control Hosp Epidemiol 1996; 17: 654–9.
Giacca M, Menzo S, Trojan S, Monti-Bragadin C. Cluster analysis of antibiotic susceptibility patterns of clinical isolates as a tool in nosocomial infection surveillance. Eur J Epidemiol 1987; 3: 155–63.
Author information
Authors and Affiliations
Additional information
Read at the Fifty-fourth Annual Meeting of The Japanese Thoracic Surgery, Panel discussion, Osaka, October 3–5, 2001.
Rights and permissions
About this article
Cite this article
Yoshida, J., Kirikae, T., Yamanaka, N. et al. Evidence-based infection control in thoracic surgery. Jpn J Thorac Caridovasc Surg 50, 273–279 (2002). https://doi.org/10.1007/BF03032294
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03032294