Abstract
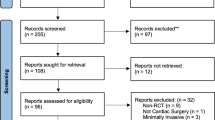
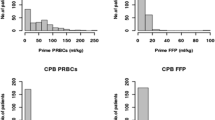
Objectives: Open heart surgery without homologous blood transfusion remains difficult in children. The introduction of vacuum-assisted cardiopulmonary bypass circuits to reduce priming volume for pediatric patients has improved the percentage of transfusion-free operations. We retrospectively analyzed blood transfusion risk factors to further reduce blood transfusion requirements after vacuum-assisted circuit introduction.Methods: From March 1995 to June 1996, 49 patients weighing between 5 and 20 kg underwent cardiac surgery with cardiopulmonary bypass at our institution, excluding hospital deaths. We retrospectively analyzed risk factors influencing blood use in 37 patients with no blood priming in cardiopulmonary bypass after introducing a vacuum-assisted system. Factors selected for univariate analysis were age, body weight, cyanosis, preoperative Hb, operation time, cardiopulmonary bypass time, aortic cross-clamping time, and intraoperative and postoperative bleeding volume. Correlation between total bleeding volume/body weight and cardiopulmonary bypass time was studied by regression analysis.Results: As risk factors, univariate analysis identified cyanotic disease, longer operation time (>210 minutes), longer cardiopulmonary bypass time (>90 minutes), longer aortic cross-clamping time (>45 minutes), greater intraoperative bleeding volume/body weight (>4 ml/kg), and greater postoperative bleeding volume/body weight (>15 ml/kg). Regression analysis showed a significant positive correlation between total bleeding volume/body weight and cardiopulmonary bypass time.Conclusions: Cyanotic disease and long bypass time are risk factors in reducing blood transfusion requirements in pediatric open heart surgery after introduction of vacuum-assisted circuits. Further efforts are needed, however, to reduce blood transfusion requirements, particularly in these children.
Similar content being viewed by others
References
Chambers LA, Cohen DM, Davis JT. Transfusion patterns in pediatric open heart surgery. Transfusion 1996; 36: 150–4.
Hatzopoulos FK, Stile CI, Rodvold KA, Sullivan BJ, Del NP, Levitsky S. Vacuum-assisted venous drainage (VAVD). Perfusion 1999; 14: 419–23.
Maeda M, Koyama T, Murase M, Teranishi K, Sakurai H, Nishizawa T. The indications and limitations of open heart surgery without homologous blood transfusion in children and infants (Eng abstr). Jpn Assn Thorac Surg 1994; 42: 1–7.
Berryessa R, Wiencek R, Jacobson J, Hollingshead D, Farmer K, Cahill G. Vacuum-assisted venous return in pediatric cardiopulmonary bypass. Perfusion 2000; 15: 63–7.
Kawashima Y, Yamamoto Z, Manabe H. Safe limits of hemodilution in cardiopulmonary bypass. Surgery 1974; 76: 391–7.
Henling CE, Carmichael MJ, Keats AS, Cooley DA. Cardiac operation for congenital heart disease in children of Jehovah’s Witnesses. J Thorac Cardiovasc Surg 1985; 89: 914–20.
Ekert H, Gilchrist GS, Stanton R, Hammond D. Hemostasis in cyanotic congenital heart disease. J Pediatric 1970; 76: 221–30.
Miller BE, Mochizuki T, Levy JH, Bailey JM, Tosone SR, Tam VKH, et al. Predicting and treating coagulapathies after cardiopulmonary bypass in children. Anesth Analg. 1997; 85: 1196–202.
Chan AKC, Leaker M, Burrows FA, Williams WG, Gruenwald CE, Whyte L, et al. Coagulation and fibrinolytic profile of paediatric patients undergoing cardiopulmonary bypass. Thromb Haemost 1997; 77: 270–7.
Williams GD, Bratton SL, Ramamoorthy C. Factors associated with blood loss and blood product transfusion: a multivariate analysis in children after open-heart surgery. Anesth Analg 1999; 89: 57–64.
Williams GD, Bratton SL, Riley EC, Ramamoorthy C. Coagulation tests during cardiopulmonary bypass correlate with blood loss in children undergoing cardiac surgery. J Cardiothorac Vasc Anesth 1999; 13: 398–404.
Hardy JF, Belisle S, Janvier G, Samama M. Reduction in requirements for allogeneic blood products: nonpharmacologic methods. Ann Thorac Surg 1996; 62: 1935–43.
Takahashi Y, Tatsuno K, Kikuchi T. Open heart surgery with bloodless priming for cyanotic congenital heart diseases—the role of autologous blood donation after induction of anesthesia. J Jap Thorac Surg 1996; 44: 1075–81.
Fukahara K, Murakami A, Ueda T, Doki Y, Tsubata S, Ichida F, et al. Scheduled autologous blood donation at the time of cardiac catheterization in infants and children. J Thorac Cardiovasc Surg 1997; 114: 504–5.
Dietrich W, Barankay A, Dilthey G, Richter JA. Autotransfusion and hemoseparation in cardiac surgery. What can be saved in cardiac reoperations and operations of thoracic aortic aneurysms? Thorac Cardiovasc Surg 1989; 37: 84–8.
Zonis Z, Seear M, Reichert C, Sett S, Allen C. The effect of preoperative tranexamic acid on blood loss after cardiac operations in children. J Thorac Cardiovasc Surg 1996; 111: 982–7.
Herynkopt F, Lucchese F, Pereira E, Kalil R, Prates P, Nesralla IA. Aprotinin in children undergoing correction of congenital heart defects. A double-blind pilot study. J Thorac Cardiovasc Surg 1994; 108: 517–21.
Davies MJ, Allen A, Kort H, Weerasena NA, Rocco D, Paul CL, et al. Prospective, randomized, double-blind study of high-dose aprotinin in pediatric cardiac operations. Ann Thorac Surg 1997; 63: 497–503.
Carrel TP, Schwanda M, Vogt PR, Turina MI. Aprotinin in pediatric cardiac operations: a benefit in complex malformations and with high-dose regimen only. Ann Thorac Surg 1998; 66: 153–8.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Nakanishi, K., Shichijo, T., Kato, G. et al. Risk factors reducing blood transfusion requirements in pediatric open heart surgery after introduction of vacuum assisted circuits. Jpn J Thorac Cardiovasc Surg 49, 564–569 (2001). https://doi.org/10.1007/BF02913533
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF02913533