Summary
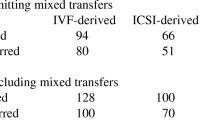
The significance of the performance of conventionalin vitro fertilization and intracytoplasmie sperm injection (IVF/ICSI) using sibling oocytes from couples with subfertile male or unexplained infertility was evaluated. A total of 410 sibling oocyte cumulus-corona complexes (OCCC) from 21 couples with subfertile male (group A) and 11 unexplained infertile couples (group B) were randomly divided, in order of retrieval, into two groups inseminated either by conventional IVF or by ICSI. The treatment outcomes and the influence of infertility factors on fertilization in each group were compared. The results showed that although the two pronuclear (2PN) fertilization rate per injected sibling oocytes was significantly higher after ICSI (group A: 68.2%±28.8%; group B: 66.2% ± 24.9%) than after conventional IVF (group A: 41.8%±32.7%; group B: 40.1% ±22.1%), the other variables studied included: the fertilization rates of per allocated sibling oocytes IVF/ICSI, the fertilization rates of sibling oocytes IVF/ICSI after excluding failed IVF fertilization cycles, as well as the eleavage rates of normal fertilization were not statistically significant (P <0.05). Similarly, though the total fertilization failure rate in the IVF group (group A: 42.9%; group B: 36.4%) was significantly higher than in the ICSI group (group A: 4.8%; group B: 0), we did not cancel cycles due to the normal fertilization of sibling oocytes. Embryo transfer was possible in all 32 couples. There were 10 clinical pregnancies in the two groups. We also discovered a possible association between some semen parameters and sperm functions of group A, and women age and duration of infertility of group B and fertilization. It is suggested that adoption of the split IVF/ICSI technology in the above cases may help eliminate fertilization failures. This is also a useful method to investigate the effect of single factor on the employment of assisted reproductive technology.
Similar content being viewed by others
References
Palermo G D, Cohen J, Rosenwaks Z. Intracytoplasmic sperm injection: a novel treatment to overcome fertilization failure. Fertil Steril, 1996, 65: 899
Li Z L, Lin H, Zhang X Net al. Intracytoplasmic sperm injection in case with a history ofin vitro fertilization failure. Asian J Androl, 2003, 5(1): 69
Martikainen H, Tiitinen A, Tomas Cet al. One versus two embryo transfer after conventional IVF and ICSI: a randomized study. Hum Reprod, 2001, 16(9): 1900
WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. New York: Cambridge University Press, 1999. 51–2
Huang Y F, Xu R J. The diagnosis of male factor infertility. Shanghai: Second Military Medical University Publishing House, 1999, 146–8
Roest J, van Heusden A M, Zeilmaker G Het al. Treatment policy after poor fertilization in the first IVF cycle. J Assist Reprod Genet, 1998, 15: 18
Aboulghar M A, Mansour R A, Serour G Iet al. Intracytoplasmic sperm injection and conventionalin vitro fertilization for sibling oocytes in cases of unexplained infertility and borderline semen. J Assist Reprod Genet, 1996, 13: 38
Hershlag A, Paine T, Kvapil Get al. in vitro fertilization-intracytoplasmic sperm injection split: an insemination method to prevent fertilization failure. Fertil Steril, 2002, 77 (2): 229
Evers J L H, De Hass H W, Land J Aet al. Treatment-independent pregnancy rate in patients with severe reproductive disorders. Hum Reprod, 1998, 13: 1206
Donnelly E T, Lewis S E M, McNally Jet al. In vitro fertilization and pregnancy rates: the influence of sperm motility and morphology on IVF outcome. Fertil Steril, 1998, 70: 305
Hammadeh M E, Zavos P M, Rosenbaum Pet al. Comparison between the quality and function of sperm after semen processing with two different methods. Asian J Androl, 2001, 3: 125
Olds-Clarke P. How does poor motility alter sperm fertilizing ability? J Androl, 1996, 17: 183
Gianaroli L, Magli M C, Ferraretti A Pet al. Reducing the time of sperm-oocyte interaction in human in-vitro fertilization improves the implantation rate. Hum Reprod, 1996, 11: 166
Author information
Authors and Affiliations
Additional information
LI Zhiling, female, born in 1964, Graduate Student, earrently studying on a doctoral program of Tongji Medical. Colleage, Huazhong Universitol Science and Technology. Wuhan 430022, China
Rights and permissions
About this article
Cite this article
Zhiling, L., Hong, L., Wanfen, X. et al. Fertilization of IVF/ICSI using sibling oocytes from couples with subfertile male or unexplained infertility. Current Medical Science 24, 365–368 (2004). https://doi.org/10.1007/BF02861869
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF02861869