Abstract
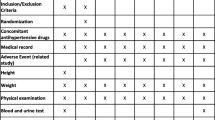
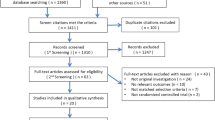
Lowering blood pressure (BP) reduces cardiovascular events, but aggressive BP management may not be advantageous. Optimal BP control (target: < 120/ 80 mm Hg) and conventional BP control (target: < 140/90 mm Hg) were compared in patients with hypertension in terms of target-organ damage and tolerability. A total of 23 patients with hypertension were randomly assigned to optimal versus conventional therapy for 6 months. Therapy was initiated with lercanidipine 10 mg/day. For BP control, the dose could be doubled or other drugs added. Three indices of target-organ damage were studied: left ventricular mass (LVM) index, flow-mediated dilatation (FMD) of the brachial artery, and 24-hour urinary albumin excretion. The BP decreased markedly by 21.3±3.4/13.2±1.7 mm Hg in the conventional therapy group and by 26.6±3.6/17.9±1.5 mm Hg in the optimal therapy group. Diastolic BP was significantly lower, by 4.7±2.3 mm Hg, in the optimal therapy group (P < .05). Ambulatory BP was also decreased in both groups. There was no significant change in LVM or FMD in either group. Baseline LVM index and FMD values were correlated with systolic BP (r=0.51, P=.02; r=0.54, P=.009). In the optimal therapy group, urinary albumin excretion increased significantly (P=.04). Plasma levels of B-type natriuretic peptide (BNP) decreased with antihypertensive therapy (P=.03). Treatment was well tolerated, and none of the patients withdrew from the study. There was no significant difference in adverse events between the 2 groups. Optimization of BP is feasible, safe, and well tolerated; however, a larger study of longer duration may be needed to demonstrate improvements in LVM and endothelial function with conventional versus optimal therapy.
Similar content being viewed by others
References
Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358:1305–1315.
Julius S, Kjelsen SE, Weber M, et al, for the VALUE trial group. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363:2022–2031.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;51:1755–1762.
Chobanian AV, Bakris GL, Black HR, et al, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572.
European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–713.
Lazarus JM, Bourgoignie JJ, Buckalew VM, et al. Achievement and safety of a low blood pressure goal in chronic renal disease: the Modification of Diet in Renal Disease Study Group. Hypertension. 1997;29:641–650.
Cheung BMY, Lau CP, Wu BZ. Efficacy and tolerability of three new dihydropyridine calcium channel blockers: amlodipine, felodipine and isradipine. Clin Ther. 1998;20:1159–1169.
Lau CP, Cheung BMY. Relative efficacy and tolerability of lacidipine and amlodipine in patients with mild-to-moderate hypertension: a randomised double-blind study. J Cardiovasc Pharmacol. 1996;28:328–331.
Cheung BMY, Cheung AHK, Ho SPC, Lau CP, Kumana CR. Utilisation of antihypertensive drugs in a hypertension clinic in 1996 and 1998. J Clin Pharmacol. 1999;39:969.
Cheung BMY, Wong YL, Lau CP. Queen Mary utilisation of antihypertensive drugs study: use of antihypertensive drug classes in the hypertension clinic 1996–2004. Brit J Clin Pharmacol. 2005;30:391–399.
Jebb SA, Cole TJ, Doman D, Murgatroyd PR, Prentice AM. Evaluation of the novel Tanita body-fat analyser to measure body composition by comparison with a four-compartment model. Br J Nutr. 2000;83:115–122.
Oh JK, Seward JB, Tajik AJ. The Echo Manual. 2nd ed. Philadelphia, Pa: Lippincott-Raven; 1999.
Cheung BMY, Lau CP. Fosinopril reduces left ventricular mass in untreated hypertensive patients: a controlled trial. Br J Clin Pharmacol. 1999;47:179–187.
Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115.
Ip MS, Tse HF, Lam B, Tsang KW, Lam WK. Endothelial function in obstructive sleep apnea and response to treatment. Am J Respir Crit Care Med. 2004;169:348–353.
Fleischmann EH, Schmieder RE. Are all antihypertensive drug classes equal in reducing left ventricular hypertrophy? Curr Cardiol Rep. 2002;4:474–478.
Cheung BMY, Kumana CR. Natriuretic peptides: their relevance in cardiovascular diseases. JAMA. 1998;280:1983–1984.
Cheung B, Brown MJ. Plasma brain natriuretic peptide and C-type natriuretic peptide in essential hypertension. J Hypertens. 1994;12:449–454.
Cheung BMY. Plasma concentration of B-type natriuretic peptide is related to diastolic function in hypertension. Clin Exp Pharmacol Physiol. 1997;24:966–968.
Cheung BMY, Law CY, Fung PCW, et al. Randomised trial of candesartan and enalapril (RACE) in the treatment of hypertension. Proceedings of the 6th Congress of the European Association for Clinical Pharmacology and Therapeutics; Istanbul, Turkey, June 24–28, 2003; p 128.
Lewis EJ, Hunsicker LG, Clarke WR, et al, for the Collaborative Study Group. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345:851–860.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cheung, B.M.Y., Man, Y.B., Tse, H.F. et al. Advantages of blood pressure optimization. Adv Therapy 22, 285–296 (2005). https://doi.org/10.1007/BF02850078
Issue Date:
DOI: https://doi.org/10.1007/BF02850078