Summary
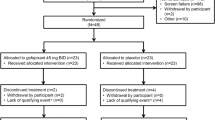
In an evaluator-blind, paralled-group, multicenter study, the efficacy and tolerability of ceftibuten 400 mg capsules once daily were compared with clarithromycin 500 mg twice daily for 7–14 days in the treatment of 309 patients with acute exacerbation of chronic bronchitis (AECB). Clinical (n=262) and microbiological (n=71) assessments were conducted before treatment, during days 4–6 of treatment, and at 0–6 and 7–21 days after treatment. Clinical efficacy success rates (cure/improvement) at the end of treatment (0–6 days) were 91.0% for ceftibuten and 93.0% for clarithromycin. In the intent-to-treat population, the overall clinical assessment showed a success rate of 77.6% (121/156) in the ceftibuten group and 78.4% (120/153) in the clarithromycin group (95% confidence interval, −10.8 to +9.0%). One patient in each of the ceftibuten and clarithromycin groups had a microbiological relapse and became a treatment failure. The overall success rate was 84.3% for ceftibuten and 86.7% for clarithromycin (C.I. −11.7%, +6.9%). Overall eradication of the target pathogens (Haemophilus influenzae, Moraxella catarrhalis, andStreptococcus pneumoniae) was 84.8% for ceftibuten and 89.5% for clarithromycin. Eradication rates for ceftibuten at 0–6 days post treatment were 95.2% (H. influenzae), 87.5% (M. catarrhalis), and 100% (S. pneumoniae), compared with 85.7%, 100% and 100%, respectively, for clarithromycin. Significantly fewer patients in the ceftibuten group experienced treatmentrelated adverse events than in the clarithromycin group (5.3 vs 21.9%; p<0.001). This difference was due to a large number of patients in the clarithromycin group reporting taste perversion (12.6%) or gastrointestinal adverse events (9.9%). Given its tolerability and efficacy profiles, and the advantage of once-daily administration, ceftibuten provides a rational alternative for the treatment of AECB.
Similar content being viewed by others
References
Prager, K., Turczyn, K., Lancashire, J., Smith, S.: National Center for Health Statistics data line. Public Health Report. 1994 vol. 109, issue 5. pp. 713–714.
Reynolds, H. Y.: Chronic bronchitis and acute infectious exacerbations. In:Mandell, G. L., Bennett, J. E., Dolin, R., (eds.): Principles and practice of infectious diseases, 4th ed. Churchill Livingstone, New York 1995, pp. 608–612.
Anthionisen, N. R., Manfreda, J., Warren, C. P. W., Herschfield, E. S., Harding, G. K. M., Nelson, N. A.: Antibiotic therapy in acute exacerbations of chronic obstructive pulmonary disease. Ann. Intern. Med. 106 (1987), 196–204.
Neu, H. C., Chick, T. W.: Efficacy and safety of clarithromycin compared to cefixime as outpatient treatment of lower respiratory tract infections. Chest 104 (1993) 1393–1399.
Elbashier, A. M., Al-Salem, A. H., Al-Jama, A. H., Khogali, A., Abusrair, H., Khot, A. P., Malik, A. G.: Bronchopulmonary infection due toMoraxella (Branhamella) catarrhalis at Qatif Central Hospital. Ann. Saudi Med. 12 (1992) 562–564.
Cazzola, M., Ariano, R., Gioia, V., Mancini, V., Rimoldi, R., Scala, G., Scoccia, S., Girbino, G.: Bacterial isolates and cigarette smoking in patients with chronic bronchitis: results from an Italian multicenter survey. Clin. Ther. 12 (1990) 105–117.
Bensch, G. W., Klaustermeyer, W. B., McCarty, J., Schworer, P. B., Taglietti, M. A.: Efficacy and safety of once-daily ceftibuten vs. twice-daily ciprofloxacin in the treatment of acute exacerbation of chronic bronchitis. Infect. Dis. Clin. Pract. 4 (2 Suppl.) (1995) S80-S87.
Hosie, J., Quinn, P., Smite, P., Sides, G.: A comparison of 5 days of dirithromycin and 7 days of clarithromycin in acute bacterial exacerbation of chronic bronchitis. J. Antimicrob. Chemother. 36 (1995) 173–183.
Verghese, A., Roberson, D., Kalbfleisch, J. H., Sarubbi, F.: Randomized comparative study of cefixime versus cephalexin in acute bacterial exacerbations of chronic bronchitis. Antimicrob. Agents Chemother. 34 (1990) 1041–1044.
Turk, D. C.: Clinical importance ofHaemophilus influenzae-1981. In:Sell, S. H., Wright, P. F. (eds.):Haemophilus influenzae: epidemiology, immunology and prevention of disease. Elsevier Science Publishing Co., New York 1982, pp. 3–9.
Chodosh, S.: Acute bacterial exacerbations in bronchitis and asthma. Am. J. Med. 82 (Suppl. 4A) (1987) 154–163.
Thabaut, A., Meyran, M., Sofer, L., Morand, A., Labia, R.: Interactions of ceftibuten with extended-spectrum beta-lactamases: a bacteriological and enzymatic analysis. Drugs Exp. Clin. Res. 20 (1994 49–54.
Jones, R. N.: Antimicrobial activity and spectrum of ceftibuten (7432-S, SCH 39720): a review of United States and Canadian results. Diagn. Microbiol. Infect. Dis 14 (1991) 37–43.
Friedland, I. R., McCracken, G. H. Jr.: Management of infections caused by antibiotic-resistantStreptococcus pneunoniae. N. Engl. J. Med. 331 (1994) 377–382.
Jones, R. N.: Ceftibuten: a review of antimicrobial activity, spectrum, and other microbiologic features. Pediatr. Infect. Dis. 14 (Suppl.) (1995) S77-S83.
Doern, G. V.:In vitro activity of ceftibuten againstHaemophilus influenzae andBranhamella catarrhalis. Diagn. Microbiol. Infect. Dis. 14 (1991) 75–77.
Jones, R. N., Barry, A. L., andThe Collaborative Antimicrobial Susceptibility Testing Group: Ceftibuten (7432-S, SCH 39720): comparative antimicrobial activity against 4735 clinical isolates, beta-lactamase stability, and broth microdilution quality control guidelines. Eur. J. Clin. Microbiol. Infect. Dis. 7 (1988) 802–807.
Wise, R., Andrews, J. M., Ashby, J. P., Thornber, D.: Ceftibutenin-vitro activity against respiratory pathogens, β-lactamase stability and mechanism of action. J. Antimicrob. Chemother. 26 (1990) 209–213.
Shawar, R., LaRocco, M., Cleary, T. G.: Comparativein vitro activity of ceftibuten (Sch 39720) against bacterial enteropathogens. Antimicrob. Agents Chemother. 33 (1989) 781–784.
Bauernfeind, A.: Ceftibuten and bactericidal kinetics. Comparativein vitro activity againstEnterobacteriaceae producing extended spectrum β-lactamases. Diagn. Microbiol. Infect. Dis. 14 (1991) 89–92.
Hardy, D. J.: Extent and spectrum of the antimicrobial activity of clarithromycin. Pediatr. Infect. Dis. J. 12 (Suppl.) (1993) S99-S105.
Fraschini, F., Scaglione, F., Demartini, G.: Clarithromycin clinical pharmacokinetics. Clin. Pharmacokinet. 25 (1993) 189–204.
Wyngaarden, J. B., Smith, L. H. Jr.,Bennett, J. C.: (eds.): Cecil Textbook of Medicine. 19th ed. W. B. Sauders Company, Philadelphia (1992).
Kamumer, R. B., Ress, R.: Randomized comparative study of ceftibuten versus cefaclor in the treatment of acute lower respiratory tract infections. Diagn. Microbiol. Infect. Dis. 14 (1991) 101–105.
Cockburn, J., Gibberd, R. W., Reid, A. L., Sanson-Fischer, R. W.: Determinants of non-compliance with short term antibiotic regimens. Br. Med. J. 295 (1987) 814–818.
Eraker, S., Kirscht, J. P., Becker, M. H.: Understanding and improving patient compliance. Ann. Intern. Med. 100 (1984) 258–268.
Eisen, S. A., Douglas, K. M., Woodward, R. S., Spitznagel, E., Przybeck, T. R.: The effect of prescribed daily dose frequency on patient medication compliance. Arch. Intern. Med. 150 (1990) 1881–1884.
Wandstrat, T. L., Kaplan, B.: Pharmacoeconomic impact of factors affecting compliance with antibiotic regimens in the treatment of otitis media. Pediatr. Infect. Dis. J. 16 (1997) S27-S29.
Perotta, R., McCabe, R., Rumans, L., Nolen, T.: Comparison of the efficacy and safety of ceftibuten and cefaclor in the treatment of acute bacterial bronchitis. Infect. Dis. Clin. Pract. 3 (1994) 270–276.
Elliott, M., Taglietti, M.: Ceftibuten in the treatment of acute exacerbations of chronic bronchitis (AECB). Poster presented at the 19th International Congress of Chemotherapy, July 16–21, 1995, Montreal, Quebec, Canada.
Bachand, R. T. Jr.: Comparative study of clarithromycin and ampicillin in the treatment of patients with acute bacterial exacerbations of chronic bronchitis. J. Antimicrob. Chemother. 27 (Suppl. A) (1991) 91–100.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ziering, W., McElvaine, P. Randomized comparison of once-daily ceftibuten and twice-daily clarithromycin in the treatment of acute exacerbation of chronic bronchitis. Infection 26, 68–75 (1998). https://doi.org/10.1007/BF02768764
Issue Date:
DOI: https://doi.org/10.1007/BF02768764