Abstract
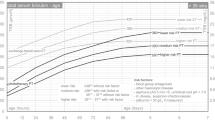
In view of the limitations in the accurate visual assessment of jaundice and its potential role as a predictive vector for serious neurologic sequelae, we propose that a universal screening of bilirubin be considered concurrent to the routine pre-disharge metabolic screening. Universal bilirubin screening in the term and near-term newborns when plotted on “Hour-specific Bilirubin Nomogram” in lieu of the usual “day-specific” value will predict the high-risk and the low-risk groups and facilitate cost-effective and individualized follow-up of those babies at risk. A percentile based bilirubin nomogram for the first week of age was constructed from hour-specific pre-and post-discharge bilirubin values of 2840 healthy term and near-term babies. The accuracy of the pre-discharge bilirubin values was determined as a predictive vector. Pre-discharge (18–72 hours age), 6.1% of the study population had bilirubin values in the high-risk zone (>95th percentile). Of these, 39.5% remained in that zone (likelihood ratio {LR}=14.08). Pre-discharge, 32.1% of the study population had bilirubin values in the intermediate risk zone (40–75th percentiles). In a clinically significant minority of these babies (6.4%), the post-discharge values moved to the high-risk zone (L−R=3.2 for the move from the upper-intermediate zone and 0.48 from the lower-intermediate zone). In the remainder 61.8% of the population who were identified to be at low risk, there was no measurable risk for significant hyperbilirubinemia (L–R =0). The bilirubin nomogram can predict which infant is at high, intermediate, and low risk for subsequent excessive hyperbilirubinemia and allows for the individualized follow-up of these high-risk babies with particular attention to those who may need evaluation and intervention. Whereas, identification of the low risk group allows for a less intense bilirubin follow-up and in whom a visual check by an experienced care-provider may suffice.
Similar content being viewed by others
References
Cashore WJ. Hyperbilirubinemia. Should we adopt a new standard of care?Pediatrics 1992; 89: 824–826.
Gourley GR. Bilirubin metabolism and kernicterus.Ado Pediatr 1997; 44: 173–229.
Brown AK, Seidman DS, Steveson DK. Jaundice in healthy, term neonates: Do we need new action levels or new approaches?Pediatrics 1992; 89 : 827–829.
Johnson L. Yet another expert opinion on bilirubin toxicity!Pediatrics 1992; 89: 829–831.
American Academy of Pediatrics, Committee on Fetus and Newborn. Hospital stay for healthy term newborns.Pediatrics 1995; 96: 788–790.
American Academy of Pediatrics Committee on Fetus and Newborn, and ACOG Committee on Obstetrics : Maternal and Fetal Medicine : Guidelines for Perinatal Care, 3rd edn, 1992; 108–109.
Johnson L, Bhutani VK. Guidelines for the management of jaundice in the term and near-term infant.Clin Perinatol 1998; 25: 555–574.
Maisels MJ, Newman TB. Kernicterus in otherwise healthy, breastfed term newborns.Pediatrics 1995; 96: 730–733.
Stevenson DK. Kernicterus in a full-term infant: the need for increased vigilance.Pediatrics. 1995; 95 : 799 (letter).
Davidson LT, Merritt KK, Weech AA. Hyperbilirubinemia in the newborn.Am J Dis Child 1941; 61: 958–980.
Bhutani VK, Johnson L, Gourley G, Dworanczyk R, Grous M. Non-invasive measurements of total serum bilirubin by multi-wavelength spectral reflectance by bili check in newborn patients.Pediatr Res 1998; 43: 167. (Abstract).
Bhutani VK, Johnson LH. Probability of subsequent hyperbilirubinemia in term healthy newborns with no ABO/Rh disease.Pediatr Res 1996; 39: 197. (Abstract).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bhutani, V.K., Johnson, L.H. Managing the assessment of neonatal jaundice : Importance of timing. Indian J Pediatr 67, 733–737 (2000). https://doi.org/10.1007/BF02723931
Issue Date:
DOI: https://doi.org/10.1007/BF02723931