Abstract
From 1983 to 1985, we performed 105 primary hip replacements in 92 osteoarthritic patients, using a non-cemented uncoated RM polyethylene cup. After a follow-up of 8.2 (7.0–9.0) years, 12 patients had died, five sockets had been revised for loosening and three for dislocation, three patients had been lost to follow-up, and three had been excluded due to severe general illnesses.
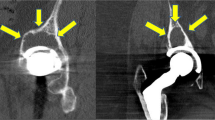
The remaining 66 patients with 79 hip replacements were reviewed clinically and by radiography, which showed osteolytic foci, mean size 13×18 mm, around 17 acetabular sockets mostly around the superior dome of the cup. Osteolytic foci were also seen around 10 femoral stems, and they were significantly more frequent in the 12 cases, where the socket had migrated.
After an exclusion of 11 patients due to a loose stem (one revised) and eight for other illnesses, an excellent or good overall functional outcome was seen in 51% of the remaining 61 hips, a fair outcome in 20% and a poor outcome in 29%. The influence of acetabular pathology on pain and function seemed to be slight.
The non-cemented uncoated polyethylene socket involves over time, a high rate of osteolysis and migration, which also endangers the fixation of the stem. These phenomena do not necessarily give symptoms. Regular radiographic reviews are therefore essential. The socket should be exchanged if the stem is revised.
Résumé
De 1983 à 1985, nous avons réalisé 105 remplacements primaires de hanches chez 92 patients arthritiques, en utilisant une cupule de polyéthylène RM non cimentée et sans revêtement. Après un suivi de 8,2 (7,0–9,0) années, 12 patients étaient décédés, cinq cupules avaient été perdues de vue et trois avaient été exclues à cause d’une sévère maladie.
Les 66 patients restants avec 70 arthroplasties totales de hanche subirent un examen clinique et radiographique. A l’examen radiographique furent découverts des foyers d’ostéolyse d’une taille moyenne de 13 mm sur 18 mm autour 17 cupules acétabulaires, principalement autour de son dôme supérieur. Des foyers d’osteolyse furent aussi vus autour de 10 tiges fémorales et ils étaient significativement plus fréquents dans les 12 cas où la cupule avait migré.
Après exclusion de 11 patients ayant eu un descellement de la tige fémorale (dont l’un a subi un contrôle) et de huit à cause d’une autre maladie, un résultat fonctionel global excellent ou bon fut observé chez 51 % des 61 hanches restantes, un résultat acceptable chez 20 % et un mauvais résultat chez 29 %. L’influence de la pathologie acétabulaire sur la douleur ou la fonction semble être faible.
La cupule en polyéthylène non cimentée sans rêvetement subit avec le temps un haut pourcentage d’ostéolyse et de migration, qui fragilise aussi la fixation de la tige. Ces phénomènes ne sont pas toujours symptomatiques. Des examens radiographiques réguliers sont de ce fait essentiels. La cupule doit être changée si la tige est changée.
Similar content being viewed by others
References
Bloebaum RD, Dupont J A (1993) Osteolysis from a press-fit hydroxyapatite-coated implant. A case study. J Arthroplasty 8: 195–202
Buechel FF, Drucker D, Jasty M, Jiranek W, Harris WH (1994) Osteolysis around uncemented acetabular components of cobalt-chrome surface replacement hip arthroplasty. Clin Orthop 298: 202–211
Buchhorn U, Willert HG, Semlitsch M, Weber H (1984) Dimensionsänderungen der Polyäthylen-Hüftpannen bei Müller-Hüftendoprotesen. Z Orthop 122: 127–135
Carlsson ÅS (1981) 351 Total hip replacements according to Charnley. A review of complications and function. Acta Orthop Scand 52: 339–344
Charnley J, Cupic Z (1973) The nine and ten year results of low friction arthroplasty of the hip. Clin Orthop 95: 9–26
Charnley J, Follacci FM, Hammond BT (1968) The long term reaction of bone to self-curing acrylic cement. J Bone Joint Surg [Br] 50-B: 822–829
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 121: 20–32
Geesink RG (1992) Clinical, radiological and human histological experience with hydroyapatite coatings in orthopaedic surgery. Acta Orthop Belg 59: 160–164
Grigoris P, Roberts P, McMinn DJ (1993) Failure of uncemented polyethylene acetabular components. J Arthroplasty 8: 433–37
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failures” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141: 17–27
Harris WH (1968) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg [Am] 51-A: 737–755
Harris WH (1994) Osteolysis and particle disease in hip replacement. Acta Orthop Scand 65: 113–123
Harris WH, Schiller AL, Scholler JM, Freiberg RA, Scott R (1976) Extensive localized bone resorption in the femur following total hip replacement. J Bone Joint Surg [Am] 58-A: 612–618
Huo MH, Salvati ES, Lieberman JR, Betts F, Bansal M (1992) Metallic debris in femoral endosteolysis in failed cemented total hip arthroplasties. Clin Orthop 276: 157–168
Jacob H, Huggler AH, Dietschi C, Schreiber A (1974) Mechanical function of subchondral bone as experimentally determined on the acetabulum of the human pelvis. J Biomech 9/10: 625–627
Johnston RC, Fitzgerald RH, Harris WH, Poss R, Müller ME, Sledge CB (1990) Clinical and radiographic evaluation of total hip replacement: a standard system of terminology for reporting results. J Bone Joint Surg [Am] 72-A: 161–168
Krismer M, Fischer M, Klestil T, Frischhut B (1991) Uncoated polyethylene RM acetabular component versus Müller cemented acetabular component. A 4- to 8-year follow-up study. Arch Orthop Trauma Surg 110: 195–199
Maloney WJ, Jasty MJ, Harris WH, Galante JO, Callaghan JJ (1990) Endosteal erosion in assosiation with stable uncemented femoral components. J Bone Joint Surg [Am] 72-A: 1025–1034
Morscher EW, Dick W, Kernen V (1982) Cementless fixation of polyethylene acetabular component in total hip arthroplasty. Arch Orthop Trauma Surg 99: 223–230
Niinimäki TJ, Puranen JP, Jalovaara PKA (1994) Total hip arthroplasty using isoelastic femoral stem. J Bone Joint Surg [Br] 76-B: 413–418
Pierson JL, Harris WH (1994) Cemented revision for femoral osteolysis in cemented arthroplasties. Results in 29 hips after a mean 8.5-year follow-up. J Bone Joint Surg [Br] 76-B: 40–44
Remagen W, Morscher EW (1984) Histological results with cement-free implanted hip joint sockets of polyethylene. Arch Orthop Trauma Surg 103: 145–151
Ring PA (1968) Complete replacement arthroplasty of the hip by the Ring prosthesis. J Bone Joint Surg [Br] 50-B: 720–731
Schmalzried TP, Guttmann D, Grecula M, Amstutz HC (1994) The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg [Am] 76-A: 677–688
Schmalzried TP, Jasty M, Harris WH (1992) Periprosthetic bone loss in total hip arthroplasty: the role of polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg [Am] 74-A: 849–863
Stauffer RN (1982) Ten-year follow-up study of total hip replacement with particular reference to roentgenographic loosening of the components. J Bone Joint Surg [Am] 64-A: 983–990
Sutherland CJ, Wilde AH, Borden LS, Marks KE (1982) A ten-year follow-up of one hundred consecutive Müller curved-stem total hip replacement arthroplasties. J Bone Joint Surg [Am] 64-A: 970–982
Willert HG, Bertram H, Buchhorn GH (1990) Osteolysis in alloarthroplasty of the hip. The role of ultra-high molecular weight polyethylene wear particles. Clin Orthop 258: 95–107
Willert HG, Semlitsch M (1977) Reactions of the articular capsule to wear products of artificial joint prostheses. J Biomed Mater Res 11: 157–164
Wilson-MacDonald J, Morscher E, Masar Z (1990) Cementless uncoated polyethylene acetabular components in total hip replacement. J Bone Joint Surg [Br] 72-B: 423–430
Wroblewski BM, Lynch M, Atkinson JR, Dowson D, Isaac GH (1987) External wear of the polyethylene socket in cemented total hip arthroplasty. J Bone Joint Surg [Br] 69-B: 61–63
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Niinimäki, T.J., Ruuskanen, M.M. & Jalovaara, P.K.A. Osteolysis around uncoated polyethylene acetabular cups. Eur J Orthop Surg Traumatol 5, 113–118 (1995). https://doi.org/10.1007/BF02716252
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02716252