Abstract
This study was designed to investigate the reproducibility and clinical relevance of several lung function and exercise test indices in a sample of patients with stable severe chronic obstructive pulmonary disease (COPD).
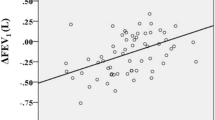
Twenty subjects (ages 67.8±2.0 years, forced expiratory volume in 1s, [FEV1] 39.7±2.8% predicted) receiving conventional medical therapy and pulmonary rehabilitation were tested 4 times at 1 month intervals. Testing procedures included lung function (inspiratory vital capacity [IVC], FEV1, plethysmographic functional residual capacity [FRC], specific conductance of the airways (sGaw), single breath transfer factor divided by the alveolar volume [TL/VA]); incremental, progressive, symptom-limited, cycle exercise (maximum work load [\(\dot V\) max], maximum heart rate [HRmax], maximum ventilation [\(\dot V\) Emax], maximum oxygen uptake [\(\dot V\) O2max]); and 2 modes of submaximum exercise (12 min walking test [12 MWD] and endurance cycle test). The mean of the absolute value of the individual patient, session-to-session, variation was found to be 0.131 for FEV1, 102 ml/min for\(\dot V\) O2max. The within-subject variability was the smallest for HRmax and IVC (mean intrasubject coefficient of variation, [\(\overline {CV} \) intra] 5.0 and 6.5%) and the greatest for TL/VA, the work performed during the endurance cycle test (EW) and sGaw (\(\underline {VA} \) intra 16.5, 19.4, and 22.7%), while it was reasonably low (8.1–10.2%) for all the other variables studied. Calculation of the F ratio of the intersubject variance to the residual (total minus intersubject) variance, interpreted as a signal-to-noise ratio, yielded the following, in decreasing order: TL/VA, EW,\(\dot V\) Emax,\(\dot V\) O2max, IVC, FEV1, HRmax,\(\dot V\) max, sGaw, 12 MWD, FRC. If we assume that a useful variable should combine a low within-subject variability (\(\overline {CV} \) intra ≤10%) with a high signal-to-noise ratio, we conclude that, among all the variables studied, IVC, FEV1,\(\dot V\) Emax, and\(\dot V\) O2max are those with the greatest clinical potential for functional assessment in patients with COPD.
Similar content being viewed by others
References
Becklake MR, Leclerc M, Strobach H, Swift J (1975) The N2 closing volume test in population studies: sources of variation and reproducibility. Am Rev Respir Dis 111:141–147
Belman MJ, Mittman C (1980) Ventilatory muscle training improves exercise capacity in chronic obstructive pulmonary disease patients. Am Rev Respir Dis 121:273–280
Brown SE, Fischer CE, Stansbury DW, Light RW (1985) Reproducibility of VO2max in patients with chronic air-flow obstruction. Am Rev Respir Dis 131:435–438
Cara M (1953) Bases physiques pour un essai de mécanique ventilatoire avec application à la cinésithérapie. Poumon 9:406–411
Carter R, Peavler M, Zinkgraf S, Williams J, Fields S (1987) Predicting maximal exercise ventilation in patients with chronic obstructive pulmonary disease. Chest 92:253–259
Chen HI, Dukes R, Martin BJ (1985) Inspiratory muscle training in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 131:251–255
Cochrane GM, Prieto F, Clark TJH (1977) Intrasubject variability of maximal expiratory flow volume curve. Thorax 32:171–176
Dillard TA, Piantadosi S, Rajagopal KR (1985) Prediction of ventilation at maximal exercise in chronic air-flow obstruction. Am Rev Respir Dis 132:230–235
Dillard TA (1987) Ventilatory limitation of exercise. Prediction in COPD. Chest 92:195–196
Gandevia B, Hugh-Jones P (1957) Terminology for measurements of ventilatory capacity. Thorax 12:290–293
Gayrard P, Orebek J (1984) Mesure d’un effet bronchodilatateur par le VEMS: comment l’exprimer? Rev Mal Respir 1:81–84
Groth S, Dirksen A, Dirksen H, Rossing N (1986) Intraindividual variation and effect of learning in lung function examinations: A population study. Bull Eur Physiopathol Respir 22:35–42
Guyatt GH, Pugsley SO, Sullivan MJ, Thompson PJ, Berman LB, Jones NL, Fallen EL, Taylor DW (1984) Effect of encouragement on walking test performance. Thorax 39:818–822
Jones NL, Makrides L, Hitchcock C, Chypchar T, McCartney N (1985) Normal standards for an incremental progressive cycle ergometer test. Am Rev Respir Dis 131:700–708
Knox AJ, Morrison JFJ, Muers MF (1988) Reproducibility of walking test results in chronic obstructive airways disease. Thorax 43:388–392
McCarthy DS, Craig DB, Cherniack RM (1975) Intraindividual variability in maximal expiratory flow-volume and closing volume in asymptomatic subjects. Am Rev Respir Dis 112:407–411
McDonald JB, Cole TJ (1980) The flow-volume loop: Reproducibility of air and helium-based tests in normal subjects. Thorax 35:64–69
McGavin CR, Gupta SP, McHardy G Jr (1976) Twelve minute walking test for assessing disability in chronic bronchitis. Br Med J 1:822–823
Morgan AD, Peck DF, Buchanan DR, McHardy G Jr (1983) Effect of attitudes and beliefs on exercise tolerance in chronic bronchitis. Br Med J 286:171–173
Mungall IPF, Hainsworth R (1979) Assessment of respiratory function in patients with chronic obstructive airways disease. Thorax 34:254–258
Nicklaus TM, Burgin WW, Taylor Jr (1969) Spirometric tests to diagnose suspected asthma. Am Rev Respir Dis 100:153–159
Noseda A, Carpiaux JP, Vandeput W, Prigogine T, Schmerber J (1987) Resistive inspiratory muscle training and exercise performance in COPD patients: a comparative study with conventional breathing retraining. Bull Eur Physiopathol Respir 23:457–463
Owens MW, Kinasewitz GT, Strain DS (1986) Evaluating the effects of chronic therapy in patients with irreversible air-flow obstruction. Am Rev Respir Dis 134:935–937
Pardy RL, Rivington RN, Despas PJ, Macklem PT (1981) Inspiratory muscle training compared with physiotherapy in patients with chronic airflow limitation. Am Rev Respir Dis 123:421–425
Pennock BE, Rogers RM, McCaffree DR (1981) Changes in measured spirometric indices. What is significant? Chest 80:97–99
Peslin R, Gallina C, Rotger M (1987) Methodological factors in the variability of lung volume and specific airway conductance measured by body plethysmography. Bull Eur Physiopathol Respir 23:323–327
Pham QT, Mur JM, Cavelier C, Meyer-Bisch C, Chau N, Huong ND (1981) Indices fonctionnels respiratoires: variabilité, valeurs de référence et pouvoir discriminant. Bull Eur Physiopathol Respir 17:949–961
Servera E, Gimenez M, Mohan-Kumar T, Candina R, Bonassis JB (1983) Oxygen uptake at maximal exercises in chronic airflow obstruction. Bull Europ Physiopath Resp 19:553–556
Silverman M, Barry J, Hellerstein H, Janos J, Kelsen S (1988) Variability of the perceived sense of effort in breathing during exercise in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 137:206–209
Sonne LJ, Davis JA (1982) Increased exercise performance in patients with severe COPD following inspiratory resistive training. Chest 81:436–439
Spector S, Luparello TJ, Kopetzky MT, Souhrada J, Kinsman RA (1976) Response of asthmatics to metacholine and suggestion. Am Rev Respir Dis 113:43–50
Stebbings JH Jr (1971) Chronic respiratory disease among nonsmokers in Hagerstown, Maryland. II. Problems in the estimation of pulmonary function values in epidemiological surveys. Environ Res 4:163–192
Strain DS, Kinasewitz GT, Franco DP, George RB (1985) Effect of steroid therapy on exercise performance in patients with irreversible chronic obstructive pulmonary disease. Chest 88:718–721
Swinburn CR, Wakefield JM, Jones PW (1985) Performance, ventilation and oxygen consumption in three different types of exercise test in patients with chronic obstructive lung disease. Thorax 40:581–586
Working Party “Standardization of Lung Function Tests”, Ph. H. Quanjer, Scientific Secretary (1983) Standardization lung function testing. Bull Eur Physiopathol Respir 19 (suppl 5)
Yamane T (1973) Statistics. An introductory analysis, 3rd ed. Harper & Row, New York
Yernault JC, Noseda A, Van Muylem A, Estenne M (1983) Variability in lung elasticity measurements in normal humans. Am Rev Respir Dis 128:816–819
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Noseda, A., Carpiaux, JP., Prigogine, T. et al. Lung function, maximum and submaximum exercise testing in COPD patients: Reproducibility over a long interval. Lung 167, 247–257 (1989). https://doi.org/10.1007/BF02714953
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02714953