Abstract
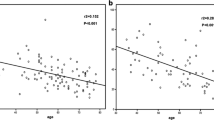
Seventeen patients with progressive systemic sclerosis (PSS) were evaluated with manometry for anorectal function, and an additional 36 age-matched normal subjects were collected as a control group. The study group had a significant decrement of maximum basal pressure (MBP), 42.6±27.0 mm Hg, in PSS as compared with the control group, 71.2±24.9 mm Hg (P=.0004). The difference in the functional length (FL) of the anal canal, PSS∶control=2.4±1.0 cm∶3.7±0.5 cm (P=.0001); the volume of first defecating sensation, PSS∶control=66.3 ±35.2 ml∶125.1±43.8 ml; the voluntary component, the difference between maximum squeeze pressure (MSP) and MBP, PSS∶control=116.6±73.6 mm Hg∶61.8±35.9 mm Hg (P=.0087), were also found to be statistically significant. Nevertheless, the MSP and maximal tolerable capacity (Vmax) showed no difference in these two groups (MSP, PSS∶control=159.3±88.1 mm Hg∶132.9±44.9 mm Hg,P=.259), (Vmax, PSS∶control=193.1±67.7 ml∶230.0±60.9 ml,P=.0526), Twelve (71 percent) of 17 patients did not have rectoanal inhibitory reflex, and paradoxical contraction during rectal balloon inflation was noted in ten patients. Nine patients had different degrees of anal incontinence and abnormal anometric profiles were found in six of eight asymptomatic patients. Therefore, only two patients (12 percent) had neither symptoms nor anometric evidence of anorectal involvement in PSS. Two patients with long-standing disease received posterior anal repair for stool incontinence, the postoperative results were satisfactory both subjectively and objectively. The average MBP increased from 0 to 20 mm Hg, average FL from 0 to 1.5 cm. Patients complained less frequently about stool incontinence or soiling, and their daily life is now more comfortable. The analysis indicates that anorectal function in PSS is affected much more frequently and earlier than thought. Anorectal manometry can be used as an adjuvant in diagnosing controversial cases. Once anal incontinence occurs, posterior anal repair can achieve good results after six months of follow-up.
Similar content being viewed by others
References
Cohen S, Laufer I, Snape WJ, Shiau Y-F, Levine GM, Jiminez S. The gastrointestinal manifestation of scleroderma: pathogenesis and management. Gastroenterology 1980;79:155–66.
Poirier TJ, Rankin GB. Gastrointestinal manifestations of progressive systemic sclerosis based on a review of 364 cases. Am J Gastroenterol 1972;58:30–44.
Jayson MI, Salmon PR, Gough J, Poliness T, Bishton RL. Spontaneous bowel perforation in intestinal scleroderma. Postgrad Med J 1972;48:56–8.
Davis RP, Hines JR, Flinn WR. Scleroderma of the colon with obstruction: report of a case. Dis Colon Rectum 1976;19:256–9.
Edwards DA, Lennard-Jones JE. Diffuse systemic sclerosis presenting as infarction of the colon. Proc R Soc Med 1960;53:877–9.
Scott JT. Copeman's textbook of the rheumatic disease. 6th ed. New York: Churchill Livingstone, 1986:1364–81.
D'Angelo WA, Fries JF, Masi AT, Shulman LE. Pathologic observation in systemic sclerosis (scleroderma). Am J Med 1969;46: 428–40.
Lorentzen M, Hoffman J. Scleroderma of the colon presenting with acute abdominal symptoms. Acta Chir Scand 1984;150: 511–2.
Sacher P, Buchmann P, Burger H. Stenosis of the large intestine complicating scleroderma and mimicking a sigmoid carcinoma. Dis Colon Rectum 1983;26:347–8.
Hamel-Roy T, Devroede G, Arhan P. Comparative esophageal and anorectal motility in scleroderma. Gastroenterology 1985;88:1–7.
Hurwitz AL, Durancean A, Postlewait RW. Esophageal dysfunction and Raynaud's phenomenon in patients with scleroderma. Am J Dig Dis 1976;21:601–6.
Sonnex C, Paice E, White AG. Autonomic neuropathy in systemic sclerosis: a case report and evaluation of six patients. Ann Rheum Dis 1986;45:957–60.
Burleigh DE, D'Mello A, Parks AG. Responses of isolated human internal anal sphincter to drugs and electrical field stimulation. Gastroenterology 1979;77:484–90.
Frenckner B, Ihre T. Influence of antonomic nerves on the internal anal sphincter in man. Gut 1976;17:306–12.
Garry RC. The responses to stimulation of the caudal end of the large bowel in the cat. J Physiol 1933;78:208–24.
Porter NH. Physiological study of the pelvic floor in rectal prolapse. Ann R Coll Surg Engl 1962;31:379–404.
Lane RH, Parks AG. Function of the anal sphincter following colo-anal anastomosis. Br J Surg 1977;64:596–9.
Di Trapani G, Pocchiari M, Masullo C, Albanese A, Tulli A, Peripheral neuropathy in the course of progressive systemic sclerosis: light and ultrastructural study. Ital J Neurol Sci 1982;3:341–8.
Rajapakse CNA, Bancewicz J, Jones CJP, Jayson MI. Pharyngo-oesophageal dysphagia in systemic sclerosis. Ann Rheum Dis 1981;40:612–4.
Author information
Authors and Affiliations
About this article
Cite this article
Chiou, A.WH., Lin, JK. & Wang, FM. Anorectal abnormalities in progressive systemic sclerosis. Dis Colon Rectum 32, 417–421 (1989). https://doi.org/10.1007/BF02563695
Issue Date:
DOI: https://doi.org/10.1007/BF02563695