Abstract
Introduction
Drug therapy for the prevention of migraine attacks is becoming more and attacks is becoming more and more important. The aims of such prophylactic treatment are to reach a lower frequency, shorter duration and milder intensity of migraine attacks, and to reduce the intake of anti-migraine medication, to improve the quality of life and working ability. The question of efficacy and tolerance of established migraine prophylactics [1] has been thoroughly investigated in many studies. So far the question of sustained efficacy after a successful prophylactic treatment completion has not been a research priority, but it is nonetheless of great importance. Researchers at the neurologic scientific research institute of the university of Naples have followed up migraine out-patients after successful prophylactic treatment and observed that prophylactic agents differ not only in their immediate efficacy and safety, but also in long-term efficacy. Therefore, an open pilot study was performed with the prophylactic agents propranolol, flunarizine, pizotifen, DHE retard, methysergide and cyclandelate in the recommended dossages (Tabe 1).
Objective and methods
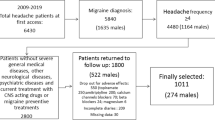
The aim of this study was to determine whether the various prophylactic agents available differ in active and long-term efficacy (at the end of a period after a successful prophylaxis=follow-up) and in the distribution of long-term responders at the end of the follow-up. The side effects of all prophylactic agents during active prophylaxis were also compared. Initially, 387 outpatients who had successfully completed a period of prophylactic treatment were recruited, and 208 were included in the study. At the time of follow-up a further period of prophylactic treatment was recommended if the efficacy rate was lower than 40% of the baseline at the end of the active prophylaxis period. The patients kept migraine headache daries (MHD) during the active prophylaxis and the follow-up, recording the following migraine objectives: number of attacks, pain total index (PTI), frequency of awakening with headache, and use of analgesics.
Results
The results showed that cyclandelate—actually a drug that is not yet officially accepted—had especially good results from the aspects of immediate efficacy, long-term efficacy and tolerance, compared with all other prophylactic agents. Significant differences were found in the duration of active prophylaxis. The mean monthly duration for patients treated with pizotifen (4.2), cyclandelate (3.9), and DHE retard (3.8) was longer than for those treated with flunarizine (2.8), and for patients treated with pizotifen it was longer than for those receiving propranolol (3.4). The mean duration (in months) of the postprophylactic period was distinctly longer for patients treated with cyclandelate (18.2) than for patients treated with DHE retard (12.9), flunarizine (13.1), propranolol (13.3) or pizotifen (13.8), but comparable with that after methysergide (17.2). Among the 208 patients, 85 were long-term responders (with no indication for repeated prophylaxis). No significant differences were found between the various groups, but the group of patients treated with cyclandelate was the only one with more than 50% long-term responders (18 vs 14). In general, the side effects of pizotifen, flunarizine and DHE retard seemed to be most pronounced. For cyclandelate, propranolol and methysergide fewer side effects were reported.
Conclusion
In spite of the uncontrolled pilot design, it can be said in summary that all prophylactic drugs were effective. Cyclandelate had a good safety profile, and in efficacy it was at least comparable to the other prophylactic drugs. Patients treated with cyclandelate had a longer duration of active treatment and likewise a longer period of follow up. In addition, the proportion of patients with “no indication for repeated prophylaxis” at follow up was higher than for any of the other drugs. The results are interesting for medical practice and suggest replication in a randomized blind study. If the results yielded by the present study are confirmed, cyclandelate should be classified as a drug of first choice for migraine prophylaxis.
Zusammenfassung
Der prophylaktischen Therapie der Migräne kommt große Bedeutung zu. Dabei steht neben der Frage nach der Effektivität unterschiedlicher Prophylaktika vor allem auch deren anhaltende Wirksamkeit nach einer erfolgreichen Prophylaxe sowie die Häufigkeit unerwünschter Nebenwirkungen im Vordergrund. Hierzu wurde am Institut für neurologisch wissenschaftliche Forschung der Universität Neapel eine retrospektive Analyse bei 208 mit unterschiedlichen Prophylaktika behandelten Patienten durchgeführt. Es zeigte sich, daß das bisher noch nicht zu den anerkannten Migräneprophylaktika zählende Cyclandelat bezüglich anhaltender Wirksamkeit nach erfolgreicher Prophylaxe und geringer Häufigkeit unerwünschter Nebenwirkungen besonders günstige Ergebnisse erzielte. Sollte sich dies Ergebnis in prospektiven Doppelblindstudien bestätigen, müßte Cyclandelat künftig als ein Migräneprophylaktikum der ersten Wahl empfohlen werden.
Similar content being viewed by others
Literatur
Aschoff JC (1989) Langzeitprophylaxe der Migräne mit Metoprolol. Therapiewoche Neurol Psychiatr (Sonderheft) 2:24
Bono G, Manzoni GC, Martucci N, Baldrati A, Farina S, Cassbogi F, De Carolis P, Carolis P, Nappi G (1985) Flunarizine in common migraine: Italian cooperative trial. II. Long-term follow-up responders’ definition. Cephalalgia 5 [Suppl 2]:155
Headache Classification Commitee of the International Headache Society (1988) Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 8 [Suppl 7]:19
Martinez-Lage JM (1988) Flunarizine (Sibelium) in the prophylaxis of migraine. An open, long-term, multicenter trial. Cephalgia 8 [Suppl 8]:15
Mastrosimone F, Iaccarino C, de Caterina G (1992) Efficacy and tolerance of Cyclandelate versus Pizotifen in the prophylaxis of migraine J Med 23:1
Soyka D, Diener HC, Pfaffenrath V, Gerber WD, Ziegler A (1992) Therapie und Prophylaxe der Migräne. HMMW 134:145
Wöber C, Wöber-Bingöl C, Koch G, Wessely P (1991) Long-term results of migraine prophylaxis with flunarizine and beta-blockers. Cephalalgia 11:251
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Haag, G., Mastrosimone, F., Iaccarino, C. et al. Langzeitwirksamkeit und Nebenwirkungen verschiedener Migräneprophylaktika—eine retrospektive Analyse. Schmerz 8, 162–169 (1994). https://doi.org/10.1007/BF02530393
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02530393