Abstract
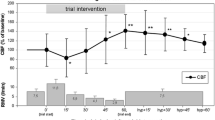
We experimentally evaluated the minimum cerebral bral blood flow required for brain protection during 90 min of selective cerebral perfusion (SCP) at moderate hypothermia ranging from 24° to 28°C, using short-latency somatosensory evoked potentials (SSEPs) as a monitor for cerebral electrical activity. Twenty mongrel dogs were divided into two groups of 10. In group A the brain temperature was lowered to 26°–28°C by core cooling using cardiopulmonary bypass (CPB), and in group B the brain was cooled to 24°C. Each group was subdivided into high-flow (H) and low-flow (L) groups according to the flow rate of SCP. In the high-flow subgroups of group A (group AH,n=5) and group B (group BH,n=5), the flow rate of SCP was maintained at 5 ml/kg/min. In the low-flow subgroups of group A (group AL,n=5) and group B (group BL,n=5), the SCP flow was 3 ml/kg/min. After systemic hypothermia and circulatory arrest, SCP was performed for 90 min via the innominate artery. In the high-flow subgroups (AH + BH), all SSEP wave components from P1 to N2 were completely preserved in 9 of the 10 dogs after 90 min of SCP, with 90% recovery rate of SSEPs. In the low-flow subgroups (AL+BL), the recovery rate of SSEPs was 30%. In four dogs without full recovery of SSEPs in group AL, all components of SSEPs were abolished; however, P1N1 waves, which are regarded as an electrical activity originating from the subcortical pathway, were restored in two of the three in group BL. Therefore, it might be suggested that more than 5 ml/kg/min of SCP is needed as a minimum cerebral blood flow for 90 min at hypothermia of 24° to 28°C, but 3 ml/kg/min is insufficient to protect the whole brain.
Similar content being viewed by others
References
Wilson GJ, Rebeyka IM, Coles JG, Desrosiers AJ, Dasmahaptra HK, Adler S, Feitler DA, Sherret H, Kielmanowicz S, Ikonomidis J, Gatley RAA, Taylor M. Loss of the somatosensory evoked response as an indicator of reversible cerebral ischemia during hypothermic, low-flow cardiopulmonary bypass. Ann Thorac Surg 1988;45:206–209
Kazui T. Surgical results of ascending and aortic arch replacement using selective cerebral perfusion. In: Kawashima Y, Takamoto S (eds) Brain protection in aortic surgery. Amsterdam, Tokyo: Elsevier, 1997;151–156
Bachet J, Guilmet D, Banfi C, Dreyfus G, Goudot B, Brodaty D, Dubois C, Delentdecker P. Surgery of aortic arch aneurysm with cold blood antegrade cerebroplegia. In: Kawshima Y, Takamoto S (eds) Brain protection in aortic surgery. Amsterdam, Tokyo: Elsevier, 1997;139–150
Oumi M. Brain damage following aortic arch repair with regard to techniques of selective cerebral perfusion and preoperative cerebral lesions. Kyobugeka 1998;51:177–182
Kazui T. Antegrade versus retrograde cerebral perfusion during aortic arch surgery. Ann Thorac Cardiovasc Surg 1997;3:158–160
Svensson LG. Brain protection. J Card Surg 1997;12:326–330
Sakurada T, Kazui T, Tanaka H, Komatsu S. Experimental study of limits of retrograde cerebral perfusion. J Jpn Assn Thorac Surg 1996;44:1860–1866
Nakamura S. Determination of the safe limits of the duration of profoundly hypothermic circulatory arrest by analysis of short latency somatosensory evoked potentials. St Marianna Med J 1990;18:846–857
Ropper AH. Evoked potential in cerebral ischemia. Stroke 1986;17:3–5
Endo S, Kawada T, Nishimura K, Funaki S, Takei H, Yamate N, Hoshi T. Usefulness of simultaneous monitoring of transcranial doppler sonography and somatosensory evoked potential during cardiopulmonary bypass. Jpn J Artif Organs 1996;25:52–55
Kawada T, Nakamura S, Nishimura K, Koyama T, Endo S, Kamata S, Takei H, Funaki S, Yamate N. Continuous monitoring of short-latency somatosensory evoked potentials during cardiac and aortic surgery. Jpn J Surg 1998;26:328–332
Rebeyka IM, Coles JG, Wilson GJ, Watanabe T, Taylor MJ, Adler SF, Mickle DAG, Romaschin AD, Ujc H, Burrows FA, Williams WG, Trusler GA, Kielmanowicz S. The effect of low flow cardiopulmonary bypass on cerebral function, an experimental and clinical study. Ann Thorac Surg 1987;43:391–396
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Murakami, H., Kawaka, T., Okada, Y. et al. Minimum cerebral blood flow in selective cerebral perfusion for brain protection within a limited period of time. J Artif Organs 3, 29–33 (2000). https://doi.org/10.1007/BF02479923
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02479923