Abstract
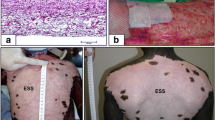
Artificial skin, a bilaminar membrane, is grafted on an excised wound immediately following injury. This bilayer membrane, made of a dermal and epidermal portion, is populated in place on the wound bed by the patient's own fibroblasts and epidermal cells producing a permanent skin replacement with an anatomically functioning dermis and epidermis. The dermal portion is a porous collagen-chondroitin 6-sulfate fibrous matrix arranged in a three dimensional pattern closely resembling the fiber pattern of normal dermis. A thin silastic covering serves as a temporary epidermis immediately after grafting until the patient's epidermal cells, seeded on the “neodermis”, grow into a confluent epidermal replacement. The autogenous “neodermis” is produced as fibroblasts and vessels migrate from the wound bed into the artificial dermal template and, using the artificial fibers as a scaffolding, synthesize new connective tissue in the collagen fiber pattern of normal dermis rather than the pattern of scar while slowly biodegrading the artificial fibers. This replacement dermis functions as normal dermis and not as scar tissue. The patient's epidermal cells seeded on the “neodermis” grow into a confluent normal appearing epidermis and with the neodermis produce a permanent skin composed of normal functioning dermal and epidermal components producedin situ by the patient's own cells. Artificial skin has been successfully used to permanently replace skin destroyed by burn injures ranging form 10 to over 95% BSA. The long term functional results in these patients have been excellent and the long term cosmetic results in preliminary studies tend to be superior to autograft. Artificial skin appears to provide a successful physiologic and cosmetic skin replacement in severe burn injury.
Similar content being viewed by others
References
Burke JF, Bondoc CC, Quinby WC. Primary burn excision and immediate grafting: a method shortening illness. J Trauma 1974; 14: 389–395.
Yannas IV, Burke JF, Huang C, Gordon PL. Correlation ofin vivo collagen degradation rate within vivo measurements. J Biomed Mat Res 1975; 9: 623–628.
Yannas IV, Burke JF. Design of an Artificial Skin I. Basic Design Principals. J Biomed Mat Res 1980; 14: 65–82.
Yannas IV, Burke JF, Jaung C, Gordon PL. Suppresion ofin vivo degradability and of immunogenicity of collagen reaction with glycosaminoglycans. Am Chem Soc Polym Preprints 1975; 16: 209–214.
Yannas IV, Burke JF, Gordon PL, Huang C, Rubenstein RH. Design of an Artificial Skin II. Control of chemical composition. J Biomed Mat Res 1980; 14: 107–132.
Degalakis N, Flink J, Stasikelio P, Burke JF, Yannas IV. Design of an Artificial Skin III. Control of pore structure. J Biomed Mat Res 1980; 14: 511–528.
Burke JF, Quinby WC, Bondoc CC. Primary excision and prompt grafting as routine therapy for the treatment of thermal burns in children. Surg Clin North Am 1976; 56: 477–494.
Burke JF, Yannas IV, Quinby WC, Bondoc CC, Jung WK. Successful use of a physiologically acceptable artificial skin in the treatment of extensive burn injury. Ann Surg 1981; 4: 413–428.
Hegarty MT, Burke JF, Tompkins R, Bondoc C, Quinby W, Behringer G, Ackroyd F. Long term evaluation of the results of treatment of burns 70 per cent or greater of the body at the Massachusetts General Hospital 1974–1985. In preparation.
Tompkins RG, Burke JF, Schoenfeld DA, Bondoc CC, Quinby WC, Behringer GC, Ackroyd FW. Prompt eschar excision: a treatment system contributing to reduced burn mortality. Ann of Surg 1986; 204: 272–281.
Author information
Authors and Affiliations
Additional information
This report is the gist of a paper read by Dr. Naoki Aikawa, a spokesman for Dr. Burke at the 87th Annual Congress of the Japan Surgical Society, Tokyo, Japan, 1987
Rights and permissions
About this article
Cite this article
Burke, J.F. Observations on the development and clinical use of artificial skin —An attempt to employ regeneration rather than scar formation in wound healing—. The Japanese Journal of Surgery 17, 431–438 (1987). https://doi.org/10.1007/BF02470745
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF02470745