Abstract
Background: The incidence of malignant melanoma is increasing faster than any other cancer, and the state of Florida has one of the highest incidence of melanoma in the United States. This increased incidence is thought to be due to the intense sunlight exposure and ultraviolet radiation exposure in the elderly population. With the increased emphasis on issues of aging, it is appropriate to study the role of age as a prognostic factor for malignant melanoma in the Florida population.
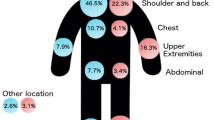
Methods: A retrospective, computer-aided search identified 442 consecutively registered patients with malignant melanoma at the Cutaneous Oncology Program. All patients had stage 1 or 2 disease (cutaneous disease only) at diagnosis. Prognostic variables analyzed included the most powerful factors for stage 1 and 2 melanoma, tumor thickness, ulceration, and Clark level of invasion. Other prognostic variables included in the analysis were the clinical variables of sex and primary site (axial vs. extremity). The population was divided into patients ≤65 and >65 years of age.
Results: Significant disease-free survival differences were encountered in the older population, with only 55% of the elderly population being disease free at 5 years compared with 65% for the younger population (p=0.0073). However, a greater percentage of patients with melanoma who were >65 years of age had ulcerated lesions (17.5% vs. 12.9%) and a greater percentage of thick lesions at diagnosis (67.2% vs. 62.7%). Both of these prognostic factors would bias the older population with a poorer survival. A stepwise regression analysis of the entire population was performed, treating age as a continuous variable. Surprisingly, increasing age along with tumor thickness were the only significant predictors for disease-free survival. After inclusion of these two prognostic variables, none of the other prognostic factors, including Clark level, ulceration, sex, and primary site, added to the prognostic model.
Conclusions: From this analysis, it is apparent that geriatric patients with melanoma have a worse prognosis than a younger control population, even after the correction for the more commonly cited prognostic factors. This information should be used in mathematical modeling to identify high-risk populations who are candidates for perhaps more aggressive primary or adjuvant therapies.
Similar content being viewed by others
References
Rigel DS. Epidemiology and prognostic factors in malignant melanoma.Ann Plast Surg 1992;28:7–8.
Balch CM, Soong SJ, Shaw HM, Milton GW. An analysis of prognostic factors in 4000 patients with cutaneous melanoma.Cutaneous melanoma. Philadelphia, PA: JB Lippincott, 1985.
Cohen HJ, Cox E, Monton K, Woodbury M. Malignant melanomas in the elderly.J Clin Oncol 1987;5:100–6.
Loggie B, Salve GR, Bean J, DasGupta TR. Invasive cutaneous melanoma in elderly patients.Arch Dermatol 1991;127:1188–93.
McHenry PM, Hole DJ, Mackie RM. Melanoma in people aged 65 and over in Scotland, 1979–89.Br Med J 1992;21:746–9.
Meyskens FL, Berdeaux DH, Parks B, et al. Cutaneous malignant melanoma (Arizona Cancer Center Experience): I. The development of stage I disease.Cancer 1988;62:1207–14.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations.J Am Stat Assoc 1958;53:457.
Cox DR. Regression model and life tables.J R Stat Soc Br 1972;34:187.
Crawford JC, Cohen HJ. Aging and neoplasia.Annu Rev Gerentol Geriatr 1984;4:3–32.
Levine J, Kopf AW, Rigel DS, et al. Correlation of thicknesses of superficial spreading malignant melanomas and age of patients.J Dermatol Surg Oncol 1981;7:311–6.
Walford RL. Immunology and aging.Am J Clin Pathol 1980;74:247–53.
Clark WH Jr, Folberg R, Ainsworth AM. Tumor progression in primary human cutaneous malignant melanomas. In: Clark WH, Goldman LI, Mastrengelo MJ, eds.Human malignant melanoma. New York: Grune & Stratton, 1979:15–31.
Reintgen DS, Cruse CW, Wells K, Saba H, Slingluff C. Isolated limb perfusion for recurrent melanoma of the extremity.Ann Plast Surg 1992;28:50–4.
Reintgen DS, Cox C, Slingluff CL, Seigler HF. Treatment of recurrent and metastatic melanoma.Ann Plast Surg 1992;28:45–9.
Balch CM, Urist M, Karakousis C, Smith T, Temple WJ, et al. Efficacy of 2-cm surgical margins for intermediate-thickness melanomas (1 to 4 mm). Results of a multi-institutional randomized surgical trial.Ann Surg 1992;218:262–7.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Austin, P.F., Wayne Cruse, C., Lyman, G. et al. Age as a prognostic factor in the malignant melanoma population. Annals of Surgical Oncology 1, 487–494 (1994). https://doi.org/10.1007/BF02303614
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02303614