Abstract
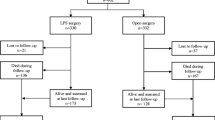
PURPOSE: Laparoscopic colorectal surgery for cancer is currently under discussion. Results of large, randomized studies will not be available for a number of years yet. This study analyses the results of such resections in consecutive patients operated on by unselected surgeons. METHODS: A prospective, observational, multicenter study was initiated on August 1, 1995, in the German-speaking countries of Europe. One year after initiation of the study, findings are presented with respect to the quality of oncologic resections. RESULTS: Of 500 operations, 231 (46 percent) were performed for cancer, 167 (33 percent) with a curative intent. The most common curative resections were as follows: 63 anterior rectum resections (38 percent), 51 sigmoid resections (30 percent), and 27 abdominoperineal resections (16 percent). Segmental resections were performed in 20 patients (12 percent). Intraoperative tumor spillage was reported in 2 percent. Mean number of lymph nodes harvested was 13 (confidence interval, 5–95 percent; range, 11.5–14.6) and positive lymph nodes harvested was 2.2 (confidence interval, 5–95 percent; range, 0.9–3.4). Significant differences were noted between participating centers in terms of number of lymph nodes resected (P<0.0001). Distal and proximal resection margins were tumorfree in every case. Lateral margins were tumor-free when examined. In the case of 63 curative anterior resections, the mean distal resection margin was 39 (confidence interval, 5–95 percent; range, 33–45) mm, and in 8 of these resections, it was less than 20 mm. Mean blood loss was 344 (confidence interval, 5–95 percent; 292–396) ml, and 21 percent of patients received blood transfusions. CONCLUSIONS: These data document that the average quality of laparoscopic colorectal procedures for cancer is satisfactory but differs among surgeons.
Similar content being viewed by others
References
Sobin SH, Wittekind C. TNM: classification of malignant tumours. 5th ed. New York: Wiley and Sons, 1997.
Monihyan BG. The surgical treatment of cancer of the sigmoïd flexure and rectum: with special attention to the principles observed. Surg Gynecol Obstet 1908;6:463–6.
Turnbull RB, Kyle K, Watson FR, Spratt J. Cancer: the influence of the no-touch isolation technique on survival rates. Ann Surg 1967;166:420–5.
Pezim ME, Nicholls RJ. Survival after high or low ligation of the inferior mesenteric artery during curative surgery for rectal cancer. Ann Surg 1984;200:729–33.
Hohenberger W, Hermanek P Jr, Hermanek P, Gall FP. Decision-making in curative rectum carcinoma surgery. Onkologie 1992;15:209–20.
Zirngibl H, Husemann B, Hermanek P. Intra-operative spillage of tumor cells in surgery for rectal cancer. Dis Colon Rectum 1990;33:610–4.
Hermanek P. pTNM and residual tumor classifications: problems of assessment and prognostic significance. World J Surg 1995;19:184–90.
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg 1982;82:613–6.
Hermanek P, Wiebelt H, Staimmer D, Riedel ST, The German Study Group Colo-Rectal Carcinoma (SGCRC). Prognostic factors of rectum carcinoma: experience of the German multicenter study SGCRC. Tumori 1995;81(Suppl 3):60–4.
Gastrointestinal Tumor Study Group. Prolongation of the disease-free interval in surgically treated rectal carcinoma. N Engl J Med 1985;312:1465–72.
Gérard A, Buyse M, Nordlinger B,et al. Preoperative radiotherapy as adjuvant treatment in rectal cancer: final results of a randomized study of the European Organization for Research and Treatment of Cancer (EORTC). Ann Surg 1988;208:606–14.
Hermanek P, Wittekind C. To what extent are laparoscopic procedures defensible in oncologic surgery? Chirurg 1994;65:23–8.
Milsom JW, Bohm B, Decanini C, Fazio VW. Laparoscopic oncologic proctosigmoidectomy with low colorectal anastomosis in a cadaver model. Surg Endosc 1994;8:1117–23.
Bohm B, Milsom JW, Kitago K, Brand M, Stolfi VM, Fazio VW. Use of laparoscopic techniques in oncologic right colectomy in a canine model [see comments]. Ann Surg Oncol 1995;2:6–13.
Decanini C, Milsom JW, Bohm B, Fazio VW. Laparoscopic oncologic abdominoperineal resection. Dis Colon Rectum 1994;37:552–8.
Nelson H, Weeks JC, Wieand HS. Proposed phase III trial comparing laparoscopic-assisted colectomyversus open colectomy. J Natl Cancer Inst Monographs 1995;19:51–6.
Lacy AM, Delgado S, Garcia-Valdecasas JC,et al. Portsite metastases and recurrence after laparoscopic colectomy in malignancy: randomized trial [abstract]. Surg Endosc 1997;11:170.
Stage JG, Schulze S, Møller P,et al. Prospective randomized study of laparoscopicversus open colonic resection for adenocarcinoma. Br J Surg 1997;84:391–6.
Macias JR, Wexner SD. Laparoscopic resection of rectal cancer: short and long term results. In: Søreide O, Norstein J, eds. Rectal cancer surgery: optimization—standardisation—documentation. Berlin: Springer-Verlag, 1997:287.
Köckerkling F, Schneider C, Reymond MA, Wittekind C. Laparoscopic colorectal surgery: indications and concept of a multicenter study. Dig Surg 1995;12:288–92.
Feussner H, Kraemer SM, Siewert JR. Wertigkeit laparoskopischer roskopischer Untersuchungstechniken bei malignen Erkrankungen. Chir Gastroenterol 1995;11:268–73.
Köckerling F, Reymond MA, Schneider C, Hohenberger W. Mistakes and hazards in oncological laparoscopic surgery. Chirurg 1997;68:215–24.
Fingerhut A. Laparoscopic-assisted colonic resection: the French experience. In: Jager RM, Wexner SD, eds. Laparoscopic colorectal surgery. New York: Churchill-Livingstone, 1996:253–8.
Huscher C, Silecchia G, Croce E,et al. Laparoscopic colorectal resection: a multicenter Italian study. Surg Endosc 1996;10:875–9.
Clinical Outcomes of Surgical Therapy (COST) Study Group. Early results of laparoscopic surgery for colorectal cancer: retrospective analysis of 372 patients treated by Clinical Outcomes of Surgical Therapy (COST) Study Group. Dis Colon Rectum 1996;39:S53–8.
Franklin ME, Rosenthal D, Abrego-Medina D,et al. Prospective comparison of openvs. laparoscopic colon surgery for carcinoma: five-year results. Dis Colon Rectum 1996;39(Suppl 10):35–46.
Fleshman JW, Fry RD, Birnbaum EH, Kodner IJ. Laparoscopic-assisted minilaparotomy approaches to colorectal diseases are similar in early outcome. Dis Colon Rectum 1996;39:15–22.
Reymond MA, Wittekind CH, Jung A, Hohenberger W, Kirchner TH, Köckerling F. The incidence of port-site metastases might be reduced. Surg Endosc 1997;11:902–6.
Johnstone PA, Rohde DC, Swartz SE, Fetter JE, Wexner SD. Port site recurrences after laparoscopic and thoracoscopic procedures in malignancy. J Clin Oncol 1996;14:1950–6.
Wexner SD, Cohen SM, Ulrich A, Reissman P. Laparoscopic colorectal surgery—are we being honest with our patients? Dis Colon Rectum 1995;38:723–7.
Köckerling F. Laparoscopic abdominoperineal excision with high transection of the inferior mesenteric artery. Surg Oncol Clin North Am 1994;3:731–43.
Sackier JM, Berci G, Hiatt JR, Hartunian S. Laparoscopic abdominoperineal resection of the rectum. Br J Surg 1992;79:1207–8.
Herrera L, Villarreal JR. Incidence of metastases from rectal adenocarcinoma in small lymph nodes detected by a clearing technique. Dis Colon Rectum 1992;35:783–8.
Cawthorn SJ, Gibbs NM, Marks CG. Clearance technique for the detection of lymph nodes in colorectal cancer. Br J Surg 1986;73:58–60.
Monson JR, Darzi A, Carey PD, Guillou PJ. Prospective evaluation of laparoscopy-assisted colectomy in an unselected group of patients. Lancet 1992;340:831–3.
Tate JJ, Kwok S, Dawson JW, Lau WY, Li AK. Prospective comparison of laparoscopic and conventional anterior resection. Br J Surg 1993;80:1396–8.
Musser DJ, Boorse RC, Madera F, Reed JF. Laparoscopic colectomy: at what cost? Surg Laparosc Endosc 1994;4:1–5.
Miller JI. Limited resections of bronchogenic carcinoma in the patient with impaired pulmonary function. Ann Thorac Surg 1993;56:769–71.
Hohenberger W, Hermanek P. Weite des aboralen Sicherheitsabstand bei anteriorer Rektumresektion. In: Gall FP, Zirngibl H, Hermanek P, eds. Das kolorektale Karzinom. München: Zuckschwerdt Verlag, 1989.
Van Ye TM, Cattey RP, Henry LG. Laparoscopically assisted colon resections compare favorably with open technique. Surg Laparosc Endosc 1994;4:25–31.
Jensen LS, Hokland M, Nielsen HJ. A randomized controlled study of the effect of bedside leucocyte deplation on the immunosuppressive effect of whole blood transfusion in patients undergoing elective colorectal surgery. Br J Surg 1996;83:973–7.
Author information
Authors and Affiliations
Consortia
Additional information
The ongoing multicenter study is supported in part by a grant from Ethicon Endosurgery, Norderstedt, Germany, and Takeda Pharma, Aachen, Germany.
Read at the Annual Congress of the Society of the American Gastrointestinal Endoscopic Surgeons, San Diego, California, March 21 to 23, 1997.
About this article
Cite this article
Köckerling, F., Reymond, M.A., Schneider, C. et al. Prospective multicenter study of the quality of oncologic resections in patients undergoing laparoscopic colorectal surgery for cancer. Dis Colon Rectum 41, 963–970 (1998). https://doi.org/10.1007/BF02237381
Issue Date:
DOI: https://doi.org/10.1007/BF02237381