Abstract
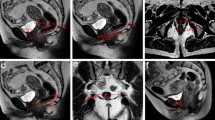
PURPOSE: This study attempts to compare the diagnostic efficacy of dynamic pelvic magnetic resonance imaging with that of videoproctography for the presence of rectocele, sigmoidocele, and intussusception as well as the measurement of anorectal angle and perineal descent in constipated patients. METHODS: Patients volunteering for the study and fulfilling the criteria for videoproctography to evaluate constipation were also scheduled for dynamic pelvic magnetic resonance imaging. Patients undergoing videoproctography were placed in the left lateral decubitus position, after which 50 ml of liquid barium paste was introduced into the rectum. After this, approximately 100 ml of thick barium paste similar to stool in consistency was injected into the rectum, and the patient was instructed to defecate while video images were taken. For dynamic pelvic magnetic resonance imaging, air, to be used as contrast, was allowed to accumulate in the rectumvia examination with the patient in the prone position. A capsule was taped to the perineal skin immediately posterior to the anal orifice for marking. Sagittal and axial T1 images were obtained through the pelvis at 8-mm intervals with dynamic breathhold sagittal images of the anorectal region obtained at rest and during strain and squeeze maneuvers. Total acquisition time per maneuver was approximately 19 seconds. The tests were performed by different examiners blinded to the result of the other evaluation. The investigations were independently interpreted, findings compared, and patients questioned regarding their impression of dynamic pelvic magnetic resonance imaging and videoproctography. RESULTS: From June 1996 to April 1997, 22 patients (15 females) with a mean age of 68 (range, 21–85) years underwent both videoproctography and dynamic pelvic magnetic resonance imaging. Dynamic pelvic magnetic resonance imaging was only able to detect 1 of 12 (8.3 percent) anterior rectoceles and one of two (50 percent) posterior rectoceles identified by videoproctography. It failed to recognize any of the rectoanal intussusception (zero of four) but did show 9 of 12 (75 percent) sigmoidoceles. Significant discrepancy of measurement of the anorectal angle and perineal descent exists between the two studies, and dynamic pelvic magnetic resonance imaging was not able to detect any (0 of 11) of the patients with increased fixed perineal descent and only half (one of two) of the patients with increased dynamic perineal descent noted on videoproctography. All 22 patients preferred dynamic pelvic magnetic resonance imaging over videoproctography because of greater comfort. CONCLUSION: Occasionally, the increased cost of new technology can be justified by the enhanced diagnostic yield. The ability to avoid unnecessary surgery or, conversely, to continue to search for otherwise occult pathology that can be surgically corrected justifies routine application of these new tools. However, this study has shown that, despite a cost of approximately ten times more for dynamic pelvic magnetic resonance imaging than for videoproctography, no clinical changes were made. Thus, on the basis of this study, we cannot endorse the routine application of dynamic pelvic magnetic resonance imaging for the evaluation of constipated patients. In certain selected individuals, it may play a role, but further study is necessary to clarify its exact role.
Similar content being viewed by others
References
Sonnenberg A, Koch TR. Epidemiology of constipation in the United States. Dis Colon Rectum 1989;32:1–8.
Whitehead WE, Drinkwater D, Cheskin L, Heller BR, Shuster MM. Constipation in the elderly living at home: definition, prevalence and relationship to lifestyle and health status. J Am Geriatr Soc 1989;37:423–9.
Talley NJ, Fleming KC, Evans JM,et al. Constipation in an elderly community: a study of prevalence and potential risk factors. Am J Gastroenterol 1996;91:19–25.
Jensen JE. Medical treatment of constipation. In: Wexner SD, Bartolo DC, eds. Constipation. Etiology, evaluation and management. Oxford: Butterworth-Heinemann, 1995:137–52.
Vaccaro CA, Cheong DM, Wexner SD, Salanga VD, Phillips RC, Hanson MR. Role of pudendal nerve terminal motor latency assessment in constipated patients. Dis Colon Rectum 1994;37:1250–4.
Pfeifer J, Agachan F, Wexner SD. Surgery for constipation: a review. Dis Colon Rectum 1996;39:444–60.
Jorge JM, Wexner SD. Anorectal manometry: techniques and clinical applications. South Med J 1993;86:924–31.
Yang YK, Wexner SD, Nogueras JJ, Jagelman DG. The role of anal ultrasound in the assessment of benign anorectal diseases. Coloproctology 1993;5:260–4.
Jorge JM, Wexner SD, Marchetti F, Rosato GO, Sullivan ML, Jagelman DG. How reliable are currently available methods of measuring the anorectal angle? Dis Colon Rectum 1992;35:332–8.
Mahieu P, Pringot J, Bodar P. Defecography: II. Contribution to the diagnosis of defecation disorders. Gastrointest Radiol 1984;9:253–61.
Brodén B, Snellman B. Procidentia of the rectum studied with cineradiography: a contribution to the discussion of causative mechanism. Dis Colon Rectum 1968;11:330–47.
Janssen LWM, van Dijke CF. Selection criteria for anterior rectal wall repair in symptomatic rectocele and anterior rectal wall prolapse. Dis Colon Rectum 1994;37:1100–7.
Yang X-M, Partanen K, Farin P, Soimakallio S. A review article. Defecography. Acta Radiol 1995;36:460–8.
Piccirillo MF, Teoh TA, Yoon KS, Patino Paul RA, Lucas J, Wexner SD. Rectoceles: the incidence and clinical significance. Techniques Coloproctol 1996;2:75–9.
Mansfield P, Grannel PK. NMR “diffraction” in solids [abstract]. J Phys (Lond) 1973;C6, L422.
Lauterbur PC. Image formation by induced local interactions: examples employing nuclear magnetic resonance. Clin Orthop 1989;244:3–6.
Stehling MK, Turner R, Mansfield P. Echo-planar imaging: magnetic resonance imaging in a fraction of a second. Science 1991;254:43–50.
Mezzacappa PM, Price AP, Haller JO, Kassner G, Hansbrough F. MRI and CT demonstration of levator sling in congenital anorectal anomalies. J Comput Assist Tomogr 1987;11:273–5.
Healy JC, Halligan S, Reznek RH,et al. Dynamic MR imaging compared with evacuation proctography when evaluating anorectal configuration and pelvic floor movement. AJR Am J Roentgenol 1997;169:775–9.
Jorge JM, Yang YK, Wexner SD. Incidence and clinical significance of sigmoidoceles as determined by a new classification system. Dis Colon Rectum 1994;37:1112–7.
Jorge JM, Ger GC, Gonzalez L, Wexner SD. Patient position during cinedefecography: influence on perineal descent and other measurements. Dis Colon Rectum 1994;37:927–31.
Kelvin FM, Maglinte DD, Hornback JA, Benson JT. Pelvic prolapse. Assessment with evacuation proctography (defecography). Radiology 1992;184:547–51.
Delemarre JB, Kruyt RH, Doornbos J,et al. Anterior rectocele: assessment with radiographic defecography, dynamic magnetic resonance imaging, and physical examination. Dis Colon Rectum 1994;37:249–59.
Ferrante SL, Perry RE, Schreiman JS, Cheng SC, Frick MP. The reproducibility of measuring the anorectal angle in defecography. Dis Colon Rectum 1991;34:51–5.
Kruyt RH, Delemarre JB, Doornbos J. Normal anorectum: dynamic MR imaging anatomy. Radiology 1991;179:159–63.
Author information
Authors and Affiliations
Additional information
Supported in part by a generous educational grant from the Caporella family.
About this article
Cite this article
Matsuoka, H., Wexner, S.D., Desai, M.B. et al. A comparison between dynamic pelvic magnetic resonance imaging and videoproctography in patients with constipation. Dis Colon Rectum 44, 571–576 (2001). https://doi.org/10.1007/BF02234331
Issue Date:
DOI: https://doi.org/10.1007/BF02234331