Abstract
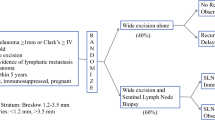
Node dissection for melanoma remains the most important therapeutic decision for the optimal management of the patient with melanoma. In Australia and in some parts of the United States, the majority of patients with intermediate thickness melanoma (1.6–4.00 mm) will undergo elective lymph node dissection. In Europe, the majority of patients with similar lesions are treated with wide local excision only. The development of an agreed policy for node dissection for melanoma awaits the results of 2 current, prospective randomized trials confirming or disproving the efficacy of elective lymph node dissection. Non-randomized studies showing a benefit or not showing a benefit are readily available but the only 2 prospective randomized studies published to date showing a benefit, have been criticized on methodologic grounds. This paper summarizes the evidence and opinions on both sides of this debate. The clinician charged with responsibility for this important decision must, as yet, make the decision to dissect lymph nodes on the basis of a perspective derived from the best available evidence.
Résumé
La lymphadénectomie reste la décision thérapeutique la plus importante dans le traitement optimal d'un patient avec mélanome. En Australie et dans certaines régions des Etats Unis la majorité des patients ayant un mélanome d'épaisseur moyenne (1.6 à 4.0 mm) auront une lymphadénectomie élective. En Europe, la majorité des patients avec le même type de lésions aura seulement une excision locale élargie. L'attitude thérapeutique à adopter dépendra certainement des résultats de deux essais thérapeutiques randomisés et prospectifs pour confirmer ou infirmer la valeur de la lymphadénectomie élective. Il existe à l'heure actuelle beaucoup d'études non randomisées qui ne permettent pas de trancher, et seulement deux études randomisées en faveur de la lymphadénectomie mais qui restent criticables du point de vue méthodologique. Cet article résume les preuves et les opinions qui sont à la base de ce débat. Le clinicien qui a la responsabilité de cette décision thérapeutique importante se doit de la pendre en connaissance des résultats les plus scientifiquement étayés.
Resumen
El papel de la disección ganglionar electiva (DGE) en el manejo del melanoma sigue siendo motivo de controversia; a pesar de múltiples trabajos relacionados con este tópico no se ha logrado un consenso a nivel mundial. Sin embaro, la decisión sobre remoción de los ganglios de drenaje linfático en un paciente con melanoma primario puede significar la vida o la muerte del paciente. En Australia y en algunas partes de los Estados Unidos la mayoría de los pacientes con melanomas de espesor intermedio (1.6–4.0 mm) es sometida a DGE; en Europa la mayoría de los pacientes con lesiones similares es tratada con resección local solamente. El desarrollo de una política unificada sobre disección ganglionar está a la espera de los resultados de dos estudios prospectivos y randomizados que corren en la actualidad para confirmar o negar la eficacia de la DGE. Estudios no randomizados que muestran un beneficio o que niegan tal beneficio están disponibles, pero los dos únicos estudios prospectivos y randomizados publicados hasta la fecha han sido motivo de crítica sobre bases metodológicas. El presente artículo resume la evidencia y las opiniones correspondientes a los dos aspectos del debate.
El médíco responsable de tan importante decisión está sometido, todavía, a emprender o no la DGE con base en una perspectiva que se deriva de la mejor evidencia disponible y teniendo en cuenta las siguientes conclusiones: la DGE no logra mejores resultados que una disección ganglionar pospuesta hasta la aparición de metástasis ganglionares, especialmente en el caso de melanomas de la extremidades; existe correlación evidente entre la incidencia de metástasis ganglionares y el espesor del melanoma, y pacientes con melanomas >2.0 mm de espesor deben ser sometido a vigilancia especial por su alta propensión a las metástasis ganglionares; en los melanomas del tronco persiste la controversia sobre si la disección ganglionar debe hacer parte del tratamiento primario en lo relativo a pacientes masculinos, en quienes se recomienda que aquellos con estado I y melanomas >1.5 mm sean ingresados a estudios randomizados, por cuanto parece existir una pequeña ventaja con la DGE. En resumen, el manejo óptimo de los pacientes con melanoma en estado I debe ser la resección del tumor primario, controles clínicos cada 3 meses por 5 años con especial atención a los ganglios regionales y disección ganglionar en el momento de aparición de ganglios clínicamente afectados; las dos excepciones son los hombres con melanomas de espesor >1.5 mm, que deben ser ingresados a estudios randomizados, y los pacientes con melanomas de espesor >2.0 mm que no puedan ser sometidos a cuidadoso seguimiento, por su alto riesgo de desarrollar metástasis ganglionares inoperables.
Similar content being viewed by others
References
Coit, D., Sauven, P., Brennan, M.: Prognosis of thick cutaneous melanoma of the trunk and extremity. Arch. Surg.125:332, 1990
McCarthy, W.H., Shaw, H.M., Milton, G.W.: Efficacy of elective lymph node dissection in 2,347 patients with clinical stage I malignant melanoma. Surg. Gynecol. Obstet.161:575, 1985
Balch, C.M., Soong, S.J., Shaw, H.M., Milton, G.W.: An analysis of prognostic factors in 4000 patients with cutaneous melanoma. In Cutaneous Melanoma: Clinical Management and Treatment Results Worldwide, C.M. Balch, G.W. Milton, editors, Philadelphia, Lippincott, 1985, p. 321–352
Karakousis, C.P., Hena, M.A., Emrich, L.J., Driscoll, D.L.: Axillary node dissection in malignant melanoma: Results and complications. Surgery108:10, 1990
Cochran, A.J., Lana, A.M.A., Wen, D.R.: Histomorphometry in the assessment of prognosis in stage II malignant melanoma. Am. J. Surg. Pathol.13:600, 1989
Veronesi, U., Adamus, J., Bandiera, D.C., Brennhovd, I.O., Caceres, E., Cascinelli, N., Claudio, F., Ikonopisov, R.L., Jarorskj, V.V., Kirov, S., Kulakowski, A., Lacour, J., Lejeune F., Mechl, Z., Morabito, A., Rode, I., Sergeev, S., Van Slooten, E., Szczygiel, K., Trapeznikov, N., Wagner, R.I.: Inefficacy of immediate node dissection in stage I melanoma of the limbs. N. Engl. J. Med.297:627, 1977
Fortner, J.H., Woodruff, J., Schottenfeld, D., Maclean, B.A.: Biostatistical basis for elective lymph node dissection for malignant melanoma. Ann. Surg.186:101, 1977
Rosenberg, S.A.: Surgical treatment of malignant melanoma. Cancer Treat. Rep.60:159, 1976
McLeod, R., Davis, N.C., Herron, J.J., Caldwell, R.A., Little, J.H., Quinn, R.L.: A retrospective survey of 498 patients with malignant melanoma. Surg. Gynecol. Obstet.126:99, 1968
Das Gupta, T.K.: Current status of surgical tratment of melanoma. Semin. Oncol.15:566, 1988
Cascinelli, N., Preda, F., Vaglini, M., Orefice, S., Morabito, A., Nava, M., Santinami, M.: Metastatic spread of stage I melanoma of the skin. Tumori69:449, 1983
Balch, C.M., Cascinelli, N., Milton, G.W., Sim, F.H.: Elective lymph node dissection: Pros and cons. In Cutaneous Melanoma: Clinical Management and Treatment Results Worldwide, C.M. Balch, G.W. Milton, editors, Philadelphia, Lippincott, 1985, pp. 131–157
Balch, C.M.: The role of elective lymph node dissection in melanoma: Rationale, results, and controversies. J. Clin. Oncol.6:163, 1988
Sim, F.H., Taylor, W.F., Ivins, J.C., Pritchard, D.J., Soule, E.H.: A prospective randomized study of the efficacy of routine elective lymphadenectomy in management of malignant melanoma: Preliminary results. Cancer41:948, 1978
Sim, F.H., Taylor, W.F., Pritchard, D.J., Soule, E.H.: Lymphadenectomy in the management of stage I malignant melanoma: A prospective randomized study. Mayo Clin. Proc.61:697, 1986
Balch, C.M.: Axillary lymph node dissection: Differences in goals and techniques when treating melanoma and breast cancer. Surgery108:118, 1990
Shaw, J.H., Rumball, E.M.: Complications and local recurrence following lymphadenectomy. Br. J. Surg.77:760, 1990
O'Brien, C.J., Gianoutsos, M.P., Morgan, M.J.: Neck dissection for cutaneous malignant melanoma. World J. Surg. (in press)
Ingvar, C., Erichsen, C., Jonsson, P.E.: Morbidity following prophylactic and therapeutic lymph node dissection for melanoma: A comparison. Tumori70:529, 1984
Cochran, A.J., Wen, D.R., Farzad, Z., Stene, M.A., McBride, W., Lana, A.M., Hoon, D.S.B., Morton, D.L.: Immune suppression by melanoma cells as a feature in the growth of metastatic disease. Anticancer Res.9:859, 1989
Goldsmith, H.S., Shah, J.P., Kim, D.H.: Prognostic significance of lymph node dissection in the treatment of malignant melanoma. Cancer26:606, 1970
Cascinelli, N., Santinami, M., Testori, A., Belli, F.: Surgical treatment of cutaneous melanoma. Reg. Cancer Treat.3:57, 1990
Balch, C.M., Soong, S.-J., Murad, T.M., Ingalls, A.L., Maddox, W.A.: A multifactorial analysis of melanoma. II. Prognostic factors in patients with stage I (localized) melanoma. Surgery86:343, 1979
Balch, C.M., Soong, S.-J., Milton, G.W., Shaw, H.M., McGovern, V.J., Murad, T.M., McCarthy, W.H., Maddox, W.A.: A comparison of prognostic factors and surgical results in 1786 patients with localized (stage I) melanoma treated in Alabama, USA, and New South Wales, Australia. Ann. Surg.196:677, 1982
Gumport, S.L., Meyer, H.W.: Treatment of 126 cases of malignant melanoma: Long term results. Ann. Surg.150:989, 1959
McNeer, G., Das Gupta, T.: Prognosis in malignant melanoma. Surgery56:512, 1964
Mundth, E.D., Guralnick, E.A., Raker, J.W.: Malignant melanoma: A clinical study of 427 cases. Ann. Surg.162:15, 1965
Southwick, H.W., Slaughter, D.P., Hinkamp, J.F., Johnson, F.E.: The role of regional node dissection in the treatment of malignant melanoma. Arch. Surg.85:63, 1962
Kirov, St., Lacour, J., Veronesi, U., Cooling, C.I., McNeer G.: Clinic on melanoma. Panel discussion. In Structure and Control of the Melanocyte, G. Della Porta, O. Mühlbock, editors, Berlin, Springer-Verlag, 1966, pp. 359–374.
Veronesi, U., Adamus, J., Bandiera, D.C., Brennhovd, I.O., Caceres, E., Cascinelli, N., Claudio, F., Ikonopisov, R.L., Javorskj, V.V., Kivor, S., Kulakowski, A., Lacour, J., Lejeune, F., Mechl, Z., Morabito, A., Rodé, I., Sergeev, S., Slooten, E. van, Szczygiel, K., Trapeznikov, N.N., Wagner, R.I.: Stage I melanoma of the limbs: Immediate versus delayed node dissection. Tumori66:373, 1980
Veronesi, U., Adamus, J., Bandiera, D.C., Brennhovd, I.O., Caceres, E., Cascinelli, N., Claudio, F., Ikonopisov, R.L., Javorskj, V.V., Kirov, S., Kulakowski, A., Lacour, J., Lejeune, F., Mechl, Z., Morabito, A., Rodé, I., Sergeev, S., Slooten, E. van, Szczygiel, K., Trapeznikov, N.N., Wagner, R.I.: Delayed regional lymph node dissection in stage I melanoma of the skin of the lower extremities. Cancer49:2420, 1982
Balch, C.M., Murad, T.M., Soong, S.-J., Ingalls, A.L., Richards, P.C., Maddox, W.A.: Tumor thickness as a guide to surgical management of clinical stage I melanoma patients. Cancer 43:883, 1979
Buraggi, G.L., Callegaro, L., Turrin, A., Cascinelli, N., Attili, A., Emanuelli, H., Gasparini, M., Deleide, G., Plassio, G., Dovis, M., Mariani, G., Natali, P.G., Scassellati, G.A., Rosa, U., Ferrone, S.: Immunoscintigraphy with 123-I, 99m-TC and 111 In-labelled F (ab')2 fragments of monoclonal antibodies to a human high molecular weight-melanoma associated antigen. J. Nucl. Med. Allied Sci.28:283, 1984
Buraggi, G.L., Callegaro, L., Mariani, G., Turrin, A., Cascinelli, N., Attili, A., Bombardieri, E., Terno, G., Plassio, G., Dovis, M., Mazzucca, N., Natali, P.C., Scassellati, D., Rosa, U., Ferrone S.: Imaging with 131-I-labelled monoclonal antibodies to a high molecular weight-melanoma associated antigen: Efficacy of whole Ig and its F(ab')2 fragments. Cancer Res.45:3378, 1985
Day, C., Sober, A., Lew, R., Mihm, M., Fitzpatrick, T., Kopf, A., Harris, M., Gumport, S., Raker, J., Malt, R., Golomb, F., Cosimi, B., Wood, W., Casson, P., Lopransi, S., Gorstein, F., Postel, A.: Malignant melanoma patients with positive nodes and relatively good prognoses. Cancer47:955, 1981
Balch, C.M., Soong, S.-J., Murad, T., Ingalls, A.L., Maddox, W.A.: A multifactorial analysis of melanoma. Ann. Surg.193:377, 1981
Eilber, F.R., Morton, D.L., Holmes, E.C., Sparks, F.C., Ramming, K.P.: Adjuvant immunotherapy with BCG in the treatment of regional lymph node metastases from malignant melanoma. N. Engl. J. Med.294:237, 1976
Gutterman, J.U., McBride, C., Freireich, E.J., Mavligit, G., Frei, E., Hersh, E.M.: Active immunotherapy with BCG for recurrent malignant melanoma. Lancet1:1208, 1973
Veronesi, U., Adamus, J., Aubert, C., Bajetta, E., Beretta, G., Bonadonna, G., Bufalino, R., Cascinelli, N., Cocconi, G., Durand, J., De Marsillac, J., Ikonopisov, R.L., Kiss, B., Lejeune, F., MacKie, R., Madej, G., Mulder, H., Mechl, Z., Milton, G.W., Morabito, A., Peter, H., Priario, J., Paul, E., Rumke, P., Sertoli, R., Tomin, R.: A randomized trial of adjuvant chemotherapy and immunotherapy in cutaneous melanoma. N. Engl. J. Med.307:913, 1982
Banzet, P., Jaquillat, C., Maral, J.: Adjuvant chemotherapy with or without immunotherapy for malignant melanoma with metastatic nodes. Proc. Am. Assoc. Cancer Res.20:333, 1979
Quagliana, J., Tranum, B., Neidhardt, J., Gagliano, R.: Adjuvant chemotherapy with BCNU, Hydrea and DTIC (BHD) with or without immunotherapy (BCG) in high-risk melanoma patients: A SWOG study. Proc. Am. Assoc. Cancer Res.21:399, 1980
Lacour, J., Lacour, F., Spira, A., Michelson, M., Petit, J.Y., Delage, G., Sarrazin, D., Contesso, G., Viguier, J.: Adjuvant treatment with Polyadenylic-Polyuridylic acid (Poly A-Poly U) in operable breast cancer. Lancet2:161, 1980
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
McCarthy, W.H., Shaw, H.M., Cascinelli, N. et al. Elective lymph node dissection for melanoma: Two perspectives. World J. Surg. 16, 203–213 (1992). https://doi.org/10.1007/BF02071522
Issue Date:
DOI: https://doi.org/10.1007/BF02071522