Abstract
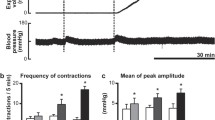
The nervous control of the motility of the human distal bowel was investigated by two physiological studies of electrical stimulation of sacral parasympathetic outflow in patients with high spinal injuries and in patients with intractable constipation following pelvic surgery. Identical and reproducible motility responses of the left colon, rectum, and anal sphincters were obtained by sequential electrical stimulation of anterior sacral roots S2, S3, and S4 in patients with spinal injury. S2 stimulation provoked isolated low-pressure colorectal contractions. S3 stimulation initiated frequency-dependent high-pressure colorectal motor activity which appeared peristaltic and was enhanced with repetitive stimuli. S4 stimulation increased colonic and rectal tone. Quantitative responses were maximal at the splenic flexure and rectum. Pelvic floor activity was stimulated in increasing magnitude from S2 to S4. These results of distal bowel motility were achieved by an implanted Brindley stimulator. A newer generation of externally active stimulators are envisaged for the control of lower bowel in fecal incontinence.
Women with intractable constipation following hysterectomy had significantly increased rectal volume and compliance together with deficits of rectal sensory function. Following stimulation with Prostigmin (neostigmin) a colorectal motility gradient was paradoxically reversed in the patients following hysterectomy, thus constituting a functional obstruction. Denervation supersensitivity was demonstrable in 2 patients tested with carbachol provocation. These findings suggest dysfunction in the autonomic innervation of the hindgut in some patients following hysterectomy.
Résumé
Le contôle nerveux de la motricité de l'intestin terminal a été évalué par deux études physiologiques comprenant une stimulation électrique du nerf parasympathique sacré, d'une part chez le patient ayant une lésion rachidienne haute et d'autre part, chez le patient ayant une constipation rebelle au traitement après chirurgie pelvienne. Par stimulation électrique séquentielle des racines sacrées antérieurs S2, S3 et S4 chez le patient ayant une lésion rachidienne, les réponses obtenues pour le côlon gauche, le rectum, et le sphincter anal étaient identiques et reproducibles. La stimulation S2 provoquait des contractions colorectales de basse pression, isolées. La stimulation S3 provoquait une activité motrice colorectale de haute pression en rapport avec la fréquence de la stimulation. Cette activité apparaissait liée au péristaltisme et elle augmentait lors des stimulations répétées. La stimulation S4 haussait le tonus rectal et colique. Le réponse quantitatives étaient maximales au niveau de l'angle gauche et du rectum. L'activité du plancher pelvien était stimulée de façon croissante de S2 à S4. Ces résultats ont été obtenus en utilisant un stimulateur implantable du type Brindley. La nouvelle génération de stimulateurs, actifs par voie externe, sera appelée à contrôler la continence aux selles du rectum. Chez la femme ayant eu une hystérectomie suivie de constipation rebelle au traitement, le volume et la compliance du rectum sont augmentés, alors que la fonction sensitive du rectum s'avère défectueuse. Après stimulation par la prostigmine (neostigmine, USP), le gradient colorectal est inversé de façon paradoxale chez les femmes hystérectomisées, créant ainsi une obstruction fonctionnelle. L'hypersensibilité de dénnervation a été mise en évidence chez les patientes ayant eu le test de provocation au carachol. Ces données suggèrent une anomalie de fonctionnement du système autonome de l'intestin distal chez certaines patientes hystérectomisées.
Resumen
El control nervioso de la motilidad del tracto intestinal distal fue investigado en dos estudios fisiológicos sobre el estímulo eléctrico de los nervios parasimpáticos sacros en 5 hombres con lesiones altas de la medula espinal y en 14 mujeres con estreñimiento intratable resultante de cirugía pélvica. Se demostraron idénticas respuestas de la motilidad del colon izquierdo, del recto y de los esfínteres anales mediante la estimulación eléctrica secuencial de las raíces sacras anteriores S2, S3 y S4 en los pacientes con lesión de la medula espinal. La estimulación de S2 indujo contracciones colorectales de baja presión. La estimulación de S3 dió origen a una actividad motora de alta presión dependiente de la frecuencia, con apariencia peristáltica, la cual apareció incrementada con estímulos repetidos. La estimulación de S4 resultó en aumento del tono colónico y rectal. Las respuestas cuantitativas aparecieron máximas a nivel del ángulo esplénico y del recto. La actividad del piso pélvico apareció estimulada, con magnitud creciente, entre S2 y S4. Tales resultados sobre la motilidad del tracto intestinal distal fueron logrados por medio de la implantación del denominado estimulador de Brindley. Se presagia una nueva generación de estimuladores de acción externa para el control de la incontinencia fecal.
Las mujeres con estreñimiento intratable consecuente a histerectomía exhibieron significativo aumento de los volumenes y de la compliancia rectales, junto con déficits de la función sensorial rectal. La estimulación con prostigmina (neostigmina, USP) revirtió, paradójicamente, un gradiente de motilidad colorrectal en las pacientes histerectomizadas, lo equivale a una obstrucción funcional. Supersensibilidad de denervación fue demonstrada en dos pacientes estudiadas por medio de la provocación con carbacol. Estos hallazgos sugieren disfunción en la inervación autonómica del intestino distal en algunas pacientes sometidos a histerectomía.
Similar content being viewed by others
References
Brindley, G.S., Polkey, C.E., Rushton, D.N.: Sacral anterior root stimulators for bladder control in paraplegia. Paraplegia20:365, 1982
Cardozo, L., Krishnan, K.R., Polkey, C.E., Rushton, D.N., Brindley, G.S.: Urodynamic observations on patients with sacral anterior root stimulators. Paraplegia22:201, 1984
Brindley, G.S.: An implant to empty the bladder or close the urethra. J. Neurol. Neurosurg. Psychiatry40:358, 1977
Smith, A.N., Varma, J.S.: The latency of the pudendo-anal reflex in man. J. Physiol.360:49P, 1984
Varma, J.S., Smith, A.N., McInnes, A.: Electrophysiological observations on the human pudendo-anal reflex. J. Neurol. Neurosurg. Psychiatry49:1411, 1986
Vereecken, R.L., De Meirsman, J., Puers, B., Van Mulders, J.: Electrophysiological exploration of the sacral conus. J. Neurol. Neurosurg. Psychiatry227:135, 1982
Varma, J.S., Smith, A.N.: Anorectal profilometry with the microtransducer. Br. J. Surg.71:867, 1984
Varma, J.S., Smith, A.N.: Reproducibility of the proctometrogram. Gut27:288, 1986
Connell, A.M.: The motility of the pelvic colon. Part I: Motility in normals and in patients with asymptomatic duodenal ulcer. Gut2:175, 1961
Rudolf, C.R.: Eight letters of Joseph (Lord) Lister to William Sharpey. Br. J. Surg.20:145, 1932
Bayliss, W.M., Starling, E.H.: The movements and innervation of the large intestine. J. Physiol. (Lond.)26:107, 1900
Elliott, T.R., Barclay-Smith, E.: Antiperistalsis and other activities of the colon. J. Physiol. (Lond.)31:272, 1904
Garry, R.C.: Responses to stimulation of caudal end of large bowel in cat. J. Physiol. (Lond.)78:208, 1933
Scott, W.E., Cantrell, J.R.: Colonmetrographic studies of the effects of section of the parasympathetic nerves of the colon. Bulletin of the Johns Hopkins Hospital85:310, 1969
Meshkinpour, H., Harmon, D., Thompson, R., Yu, J.: Effects of thoracic spinal cord transection on the colonic motor activity in rats. Paraplegia23:272, 1985
White, J.C., Verlot, M.G., Ehrentheil, O.: Neurogenic disturbances of the colon and their investigation by the colonmetrogram. Ann. Surg.112:1042, 1940
Connell, A.M., Frankel, H., Guttmann, L.: The motility of the pelvic colon following complete lesions of the spinal cord. Paraplegia1:98, 1963
Weber, J., Denis, P., Mihout, B., Muller, J.M., Blanquart, F., Galmiche, J.P., Simon, P., Pasquis, P.: Effect of brain-stem lesion on colonic and anorectal motility. Dig. Dis. Sci.30:419, 1985
Meshkinpour, H., Nowroozi, F., Glick, M.E.: Colonic compliance in patients with spinal cord injury. Arch. Phys. Med. Rehabil.64:111, 1983
Glick, M.E., Meshkinpour, H., Haldeman, S., Hoehler, F., Downey, N., Bradley, W.E.: Colonic dysfunction in patients with thoracic spinal cord injury. Gastroenterology86:287, 1984
Menardo, G., Fazio, A., Marangi, A., Genta, V., Marenco, G., Corazziari, E.: Large bowel transit in patients with paraplegia. Gut25:A1314, 1984
Haldeman, S., Glick, M., Bhatia, N.N., Bradley, W.E., Johnson, B.R.N.: Colonometry, cystometry and evoked potentials in multiple sclerosis. Arch. Neurol.39:698, 1982
Denny-Brown, D., Robertson, E.G.: An investigation of the nervous control of defaecation. Brain58:256, 1935
Roman, C., Gonella, J.: Extrinsic control of digestive tract motility. In Physiology of the Gastrointestinal Tract, L.R. Johnson, editor, New York, Raven Press, 1981, pp. 289–333
Delbro, D., Fasth, S., Fandriks, L., Hedlund, H.: On the transmission of colonic motility induced by pelvic nerve stimulation. Gut25:A1314, 1984
Devroede, G., Lamarche, J.: Functional importance of extrinsic parasympathetic innervation of the distal colon and rectum in man. Gastroenterology86:287, 1984
Schuster, M.M., Hendrix, T.R., Mendeloff, A.I.: The internal anal sphincter response: Manometric studies on its normal physiology, neural pathways and alteration in bowel disorders. J. Clin. Invest.42:196, 1963
Sherrington, C.S.: Notes on the arrangement of some motor fibres in the lumbosacral plexus. J. Physiol. (Lond.)13:672, 1892
Snooks, S.J., Henry, M.M., Swash, M.: Anorectal incontinence and rectal prolapse: Differential assessment of the innervation to puborectalis and external anal sphincter muscles. Gut26:470, 1985
Percy, J.P., Swash, M., Neill, M.E., Parks, A.G.: Electrophysiological study of motor nerve supply of pelvic floor. Lancet1:16, 1981
Parks, A.G., Porter, N.H., Melzak, J.: Experimental studies of the reflex mechanism controlling the muscles of the pelvic floor. Dis. Colon Rectum5:407, 1962
Ala, J., Mendeloff, A.I., Hendrix, T.R., Schuster, M.M.: Studies of faecal incontinence by combined manometric-electromyographic techniques. Gastroenterology48:863, 1965
Melzak, J., Porter, N.H.: Studies of the reflex activity of the external sphincter ani in spinal man. Paraplegia1:277, 1964
Frenckner, B.: Function of the anal sphincters in spinal man. Gut16:638, 1975
MacDonagh, R.P., Sun, W.M., Smallwood, R., Forster, D., Read, N.W.: Control of defecation in patients with spinal injuries by stimulation of sacral anterior nerve roots. Br. Med. J.300:1494, 1990
Binnie, N.R., Smith, A.N., Creasey, G.H., Edmond, P.: Constipation associated with spinal cord injury: The effect of pelvic parasympathetic stimulation by the Brindley stimulator. Paraplegia (in press)
Binnie, N.R., Smith, A.N., Creasey, G.H., Edmond, P.: Effect of electrical anterior sacral nerve root stimulation on pelvic floor function in paraplegic subjects. Journal of Gastrointestinal Motility3:31, 1991
Smith, P.H., Turnbull, G.A., Currie, D.W., Peel, K.R.: The urological complications of Wertheim's hysterectomy. Br. J. Urol.41:685, 1969
Hamley, H.G.: The late urological complications of total hysterectomy. J. Urol.41:682, 1969
Forney, J.P.: The effect of radical hysterectomy on bladder physiology. Am. J. Obstet. Gynecol.138:374, 1980
Woodside, J.R., McGuire, E.J.: Detrusor hypertonicity as a late complication of Wertheim hysterectomy. J. Urol.127:1143, 1982
Yalla, S.V., Andriole, G.L.: Vesicourethral dysfunction following pelvic visceral ablative surgery. J. Urol.132:503, 1984
Ferghaly, S.A., Hindmarsh, J.R., Worth, P.H.L.: Post-hysterectomy urethral dysfunction: Evaluation and management. Br. J. Urol.58:299, 1986
Parys, B.T., Haylen, B.T., Woolfenden, K.A., Parsons, K.F.: Vesico-urethral dysfunction after simple hysterectomy. Neurology and Urodynamics8:315, 1989
Smith, P.H., Ballantyne, B.: The neuroanatomical basis for denervation of the urinary bladder following major pelvic surgery. Br. J. Surg.55:929, 1968
Chang, P.L., Fan, H.A.: Urodynamic abnormalities before and/or after abdomino-perineal resection of the rectum for carcinoma. J. Urol.130:948, 1983
Long, D.M., Bernstein, W.C.: Sexual dysfunction as a complication of abdomino-perineal resection of the rectum in the male: An anatomic and physiologic study. Dis. Colon Rectum2:540, 1959
Gurnari, M., Mazziotti, F., Corazziari, E., Badiali, D., Alessandrini, A., Carenza, L., Torsoli, A.: Chronic constipation after gynaecological surgery: A retrospective study. Ital. J. Gastroenterol.20:183, 1988
Taylor, T., Smith, A.N., Fulton, P.M.: Effects of hysterectomy on bowel and bladder function. Int. J. Color. Dis.5:228, 1990
Kawimbe, B.W., Binnie, N.R., Smith, A.N.: An electromyographically derived (anismus) index in pelvic floor outlet obstruction during defaecation straining. Gut29:1487, 1988
Varma, J.S., Binnie, N., Smith, A.N., Creasey, G.H., Edmond, P.: Differential effects of sacral anterior root stimulation on anal sphincter and colorectal motility in spinal man. Br. J. Surg.73:478, 1986
Warwick, R., Williams, P.L.: Gray's Anatomy. Edinburgh, Longmans, 1980
Roman, C., Gonella, J.: Extrinsic control of digestive tract motility. In Physiology of the Gastrointestinal Tract, L.R. Johnson, editor, New York, Raven Press, 1981, pp. 89–333
Adamson, W.A.D., Aird, I.: Megacolon: Evidence in favour of a neurogenic origin. Br. J. Surg.20:220, 1932
Cannon, W.B.: Law of denervation. Am. J. Med. Sci.198:737, 1939
Lapides, J., Friend, C.R., Ajemian, E.P., Reus, W.F.: A new test for neurogenic bladder. J. Urol.88:245, 1962
Abdel-Rahman, M., Toppercer, A., Duguay, C., Watier, A., Tetrault, A., Devroede, G., Elhilali, M.: Urorectodynamics in patients with colonic inertia. Urology18:428, 1981
Watier, A., Devroede, G., Duranceau, A., Abdel-Rahman, M., Duguay, D., Forand, M.D., Tetreault, L., Arhan, P., Lamarche, J., Elhilali, M.: Constipation with colonic inertia: A manifestation of systemic disease? Dig. Dis. Sci.28:1025, 1983
Christensen, J., Rick, G.A., Robison, B.A., Stiles, M.J., Wix, M.A.: Arrangement of the myenteric plexus throughout the gastrointestinal tract of the opossum. Gastroenterology85:890, 1983
Fukai, K., Fukuda, H.: The intramural pelvic nerves in the colon of dogs. J. Physiol.354:89, 1984
Christensen, J., Schulze-Delrieu, K.: Nerves in the colon: Discovery and rediscovery. Gastroenterology89:222, 1985
de Groat, W.C., Kawatani, M.: Reorganisation of sympathetic preganglionic connections in cat bladder ganglia following parasympathetic denervation. J. Physiol.409:431, 1989
Ekstrom, J., Motmberg, L.: Functional evidence for sprouting of decentralized parasympathetic neurons in rat urinary bladder. Acta Physiol. Scand.112:7, 1984
Morrison, J.F.B.: The neural control of the bladder. In Systemic Role of Regulatory Peptides, F.K. Schattauer, editor, Stuttgart, New York, Verlag, 1982
Roe, A.M., Bartolo, D.C.C., Mortensen, N.J.Mc.C.: Slow transit constipation: Comparison between patients with and without previous hysterectomy. Dig. Dis. Sci.33:1159, 1988
Howard, E.R., Nixon, H.H.: Internal anal sphincter: Observations on development and mechanism of inhibitory responses in premature infants and children with Hirschprung's disease. Arch. Dis. Child.43:569, 1968
Godec, C.J., Esho, J., Cass, A.S.: Correlation among cystometry, urethral pressure profilometry and pelvic floor electromyography in the evaluation of female patients with voiding dysfunction symptoms. J. Urol.124:678, 1980
Catchpole, B.N.: Motor pattern of left colon before and after surgery for rectal cancer: Possible implications in other disorders. Gut29:624, 1988
Preston, D.M., Hawley, P.R., Lennard-Jones, J.E., Todd, I.P.: Results of colectomy for severe idiopathic constipation in women (Arbuthnot Lane's disease). Br. J. Surg.71:547, 1984
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Varma, J.S. Autonomic influences on colorectal motility and pelvic surgery. World J. Surg. 16, 811–819 (1992). https://doi.org/10.1007/BF02066975
Issue Date:
DOI: https://doi.org/10.1007/BF02066975