Abstract
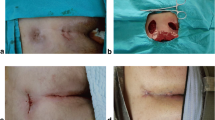
PURPOSE: After excision of the pilonidal sinus, some surgeons leave the wound open, and others close the wound primarily. The aim of this study is to compare length of hospital stay, length of time to return to work, wound infection rate, and recurrence rate in chronic pilonidal sinus patients, after modification of both closed and open techniques. METHODS: One hundred ten patients who had chronic-stage pilonidal sinus were randomly assigned to receive one of two excisional surgical procedures. One-half were treated by surgical excision and primary closure (closed technique, Group A). The other one-half were treated with Obeid's surgical excision (open technique, Group B). RESULTS: Ninety-one (46 in Group A and 45 in Group B) of 110 patients were followed for a period four months to three years. Although patients with primary closure had significantly longer hospital stays (P<0.05) than patients in the open group, they returned to work significantly earlier (P<0.05). In Group A and Group B, infection rates were 3.6 percent and 1.8 percent (P>0.01), and recurrence rates were 4.4 percent and 0 percent (P>0.01), respectively. CONCLUSION: Because both techniques have very low complication rates, treatment of chronic pilonidal sinus should be based on patient preference and characteristics, especially employment status.
Similar content being viewed by others
References
Goligher J. Surgery of the anus, rectum and colon. 5th ed. London: Bailliere Tindall, 1989:221–36.
Corman ML. Colon and rectal surgery. 2nd ed. Philadelphia: JB Lippincott, 1989:297–304.
Raffman R. A re-evaluation of the pathogenesis of pilonidal sinus. Ann Surg 1959;150:895–903.
Page BH. The entry of hair into a pilonidal sinus. Br J Surg 1969;56:32–9.
Heston JT. The aetiology of pilonidal sinuses. Br J Surg 1953;41:307–11.
Buie LA, Curtiss RK. Pilonidal disease. Surg Clin North Am 1952;32:1247–59.
Lamke LO, Larsson J, Nylen B. Results of different types of operation for pilonidal sinus. Acta Chir Scand 1974;140:321–4.
Rains AJ. Treatment of pilonidal sinus by excision and primary closure. BMJ 1959;1:171–3.
Mandel SR, Thomas CG Jr. Management of pilonidal sinus. Surg Gynecol Obstet 1972;134:448–50.
Obeid SA. A new technique for treatment of pilonidal sinus. Dis Colon Rectum 1988;31:879–85.
Bartlett W Jr. Pilonidal cyst and sinus, their management and operative treatment. Surg Gynecol Obstet 1945;80:69–74.
Ferguson LK, Mecray PM Jr. Pilonidal cysts: excision and primary suture in ambulatory patients. Am J Surg 1937;36:270–8.
Holm J, Hulten L. Simple primary closure for pilonidal sinus. Acta Chir Sand 1970;136:537–40.
Gabriel WB. Principles and practice of rectal surgery. 4th ed. London: HK Lewis, 1948.
Block LH, Greene BL. Pilonidal sinus: sclerosing method of treatment. Arch Surg 1938;37:112–22.
Close AS. Pilonidal cysts: an analysis of surgical failures. Ann Surg 1955;141:523–6.
Author information
Authors and Affiliations
About this article
Cite this article
Füzün, M., Bakir, H., Soylu, M. et al. Which technique for treatment of pilonidal sinus—Open or closed?. Dis Colon Rectum 37, 1148–1150 (1994). https://doi.org/10.1007/BF02049819
Issue Date:
DOI: https://doi.org/10.1007/BF02049819