Abstract
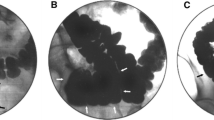
PURPOSE: A study was undertaken to assess the incidence and clinical significance of sigmoidocele as a finding during cinedefecography. METHODS: All patients who underwent cinedefecography between July 1988 and July 1992 were prospectively evaluated. Clinical data were assessed by a standardized questionnaire. Sigmoidocele was classified based on the degree of descent of the lowest portion of the sigmoid: 1° = above the pubococcygeal line; 2° = below the pubococcygeal line and above the ischiococcygeal line; 3° = below the ischiococcygeal line. This classification was then correlated with the patient's symptoms and percentage of redundancy relative to rectal length. RESULTS: Twenty-four sigmoidoceles (5.2 percent) were noted in 463 cinedefecographic studies; 289 of these patients had constipation. These five males and 19 females were of a mean age of 57 (range, 20–77) years. Nine patients had 1° sigmoidocele, seven had 2°, and eight had 3°. Percentage of sigmoid redundancy was 51 percent, 65 percent, and 88 percent for 1°, 2°, and 3°, respectively (P=0.0001). Impaired rectal emptying was present in 16 patients (67 percent). Five of eight patients with 3° sigmoidocele underwent colonic resection with or without rectopexy. The other three patients were conservatively managed. One of seven patients with 2° sigmoidocele underwent colectomy, and the other six were conservatively managed as were all nine patients with 1°. Posttreatment improvement was noted in 100 percent (6 of 6) of patients operated on but in only 33 percent (6 of 18) of patients conservatively treated. Thus, this proposed classification system yielded excellent correlation among the mean of level of the sigmoidocele, percentage of redundancy, and clinical symptoms. Furthermore, clinical significance of 3° sigmoidocele is supported by the fact that all five of 3° patients who underwent colonic resection reported symptomatic improvement at a mean follow-up of 23 (range, 15–39) months. CONCLUSION: Sigmoidocele may account for symptoms of obstructed defecation, and, therefore, it must be considered in the differential diagnosis and evaluation of constipation. Staging of sigmoidocele is useful in determining both clinical significance and optimal treatment.
Similar content being viewed by others
References
Read CD. Enterocele. Am J Obstet Gynecol 1951;62:743–57.
Wilensky AO, Kaufman PA. Vaginal hernia. Am J Surg 1940;49:31–41.
de Garengeot. Mémoire sur plusieurs hernies singulières. Mém Acad Roy Chir 1743;1:699.
Weed JC, Tyrone C. Enterocele. Am J Obstet Gynecol 1950;60:324–32.
Lash AF, Levin B. Roentgenographic diagnosis of vaginal vault hernia. Obstet Gynecol 1962;20:427–33.
Nichols DH. Types of enterocele and principles underlying choice of operation for repair. Obstet Gynecol 1972;40:257–63.
Litschgi M, Käser O. The problem of enterocele. Geburtshilfe Frauenheilkd 1978;38:915–20.
Walldén L. Defecation block in cases of deep rectogenital pouch. Acta Chir Scand 1952;165:1–122.
Ekengren K, Snellman B. Roentgen appearances in mechanical rectal constipation. Acta Radiol 1953;40:447–56.
Mahieu P, Pringot J, Bodart P. Defecography: I. Description of a new procedure and results in normal patients. Gastrointest Radiol 1984;9:247–51.
Mahieu P, Pringot J, Bodart P. Defecography: II. Contribution to the diagnosis of defecation disorders. Gastrointest Radiol 1984;9:253–61.
Bartram CI, Mahieu PH. Radiology of the pelvic floor. In: Henry MM, Swash M, eds. Coloproctology and the pelvic floor. London: Butterworth, 1985:151–86.
Finlay IG. Symposium: Proctography. Int J Colorect Dis 1988;3:67–89.
Wexner SD, Dailey TH. The diagnosis and surgical treatment of chronic constipation. Contemp Surg 1988;32:59–70.
Jorge JM, Wexner SD. A practical guide to basic anorectal physiology. Contemp Surg 1993;43:214–24.
Ekberg O, Nylander G, Fork FT. Defecography. Radiology 1985;155:45–8.
Wexner SD, Jorge JM, Nogueras JJ, Jagelman DG. Physiological assessment of colorectal functional disorders: use or abuse of technology? Eur J Surg 1994;160:167–74.
Jorge JM, Wexner SD, Marchetti F, Rosato GO, Sullivan ML, Jagelman DG. How reliable are currently available methods of measuring the anorectal angle? Dis Colon Rectum 1992;35:332–8.
Lucas JD, Landy LB. The gynecologist's approach to anterior rectoceles. Semin Colon Rectal Surg 1992;3:92–7.
McCall M. Posterior culdeplasty: surgical correction of enterocele during vaginal hysterectomy; a preliminary report. Obstet Gynecol 1952;10:592–602.
Hawksworth W, Roux JP. Vaginal hysterectomy. J Obstet Gynecol 1958;63:214–28.
Nichols DH. Surgery for pelvic floor disorders. Surg Clin North Am 1991;71:927–46.
Selvaggi F, Pesce G, Scotto Di Carlo E, Maffettone V, Canonico S. Evaluation of normal subjects by defecographic technique. Dis Colon Rectum 1990;33:698–702.
Nichols DH, Randall CL. Enterocele. In: Nichols DH, Randall CL, eds. Vaginal surgery. Baltimore: Williams & Wilkins, 1989:313–27.
Author information
Authors and Affiliations
Additional information
Read at the meeting of The American Society of Colon and Rectal Surgeons, Fort Lauderdale, Florida, May 8 to 13, 1994. Dr. Yang was a visiting clinician from the Section of Colon and Rectal Surgery, Department of Surgery, National Defense Medical Center and Tri-Service General Hospital, Taipei, Taiwan.
About this article
Cite this article
Jorge, J.M.N., Yang, YK. & Wexner, S.D. Incidence and clinical significance of sigmoidoceles as determined by a new classification system. Dis Colon Rectum 37, 1112–1117 (1994). https://doi.org/10.1007/BF02049813
Issue Date:
DOI: https://doi.org/10.1007/BF02049813