Abstract
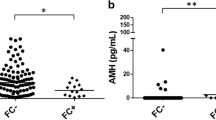
Levonorgestrel serum levels and sex hormone binding globulin (SHBG) were measured in 82 women during different years of use of Norplant implants. The ratio between levonorgestrel and SHBG was calculated as an indicator of the free biologically active fraction of levonorgestrel (free levonorgestrel index, FLI). These parameters were then correlated with the presence of luteal activity, as determined by progesterone levels above 9.6 nmol/L, in a sampling run of 10 samples taken twice a week for five consecutive weeks. Levonorgestrel serum levels remained constant around 1.0 nmol/L during the five-year period. SHBG levels were below normal for the first 18 months of use, returning to normal levels during the last three years of use. The FLI in the first two years was significantly higher than that observed in the later years. The frequency of cycles with luteal activity was 12% during the first 2 years, increasing to 44% in the latter years, when FLI levels were lower.
Our results suggest that the changes in SHBG and consequently in the free biologically active fraction of levonorgestrel may largely account for the differences in degree of ovarian suppression observed between the first two years of use of Norplant implants and the latter three, even in the absence of a significant variation in total levonorgestrel concentrations.
Résumé
Les taux sériques de lévonorgestrel et de globuline liant les hormones sexuelles (SHBG) ont été mesurés chez 82 femmes à différentes périodes des années d'utilisation des implants Norplant. Le ratio entre le lévonorgestrel et la SHBG a été calculé en tant qu'indicateur de la fraction libre biologiquement active du lévonorgestrel (indice de lévonorgestrel libre-FLI). Ces paramètres ont ensuite été corrélés avec la présence d'activité lutéale, telle que déterminée par les niveaux de progestérone dépassant 9.6 nmol/L, sur une série de 10 échantillons prélevés deux fois par semaine pendant cinq semaines consécutives. Les niveaux sériques de lévonorgestrel sont restés constants, aux alentours de 1.0 nmol/L, durant toute la période de cinq ans. Les niveaux de SHBG étaient inférieurs à la normale pendant les 18 premiers mois d'utilisation et sont redevenus normaux au cours des trois dernières années d'utilisation. Quant au FLI, il était significativement plus élevé durant les deux premières années que celui observé dans les années suivantes. La fréquence des cycles comportant une activité lutéale atteignait 12% pendant les deux premières années, augmentant à 44% pour les années suivantes, lorsque le FLI avait baissé.
Nos résultats laissent penser que les modifications de SHBG, et par conséquent de la fraction de lévonorgestrel biologiquement active, détermine sans doute largement les différences dans le degré de suppression ovarienne observé entre les deux premières années de l'utilisation des implants Norplant et les deux années suivantes, même en l'absence d'une variation significative des concentrations totales de lévonorgestrel.
Resumen
Los niveles séricos de levonorgestrel y de globulina de unión con las hormonas sexuales (SHBG) se midieron en 82 mujeres en differentes períodos de años de utilización de implantes Norplant. La proporción entre el levonorgestrel y la SHBG se calculó como indicador de la fracción libre biológicamente activa del levonorgestrel (índice de levonorgestrel libre-FLI). Estos parámetros se correlacionaron luego con la presencia de actividad lútea, según lo determinado por los niveles de progesterona superiores a 9.6 nmol/L, en una serie de 10 muestras sacadas dos veces por semana durante cinco semanas consecutivas. Los niveles séricos de levonorgestrel permanecieron constantes, a alrededor de 1.0 nmol/L durante todo el período de cinco años. Los niveles de SHBG fueron inferiores a lo normal durante los 18 primeros meses de utilización, retornando a niveles normales durante los tres últimos años de utilización. El FLI durante los dos primeros años fue significativamente superior al observado en los años siguientes. La frecuencia de los ciclos con actividad lútea fue del 12% durante los dos primeros años, aumentando al 44% en los años siguientes, cuando el FLI fue inferior.
Nuestros resultados hacen pensar que las modificaciones de la SHBG y, por consiguiente, de la fracción de levonorgestrel biológicamente activa, pueden determinar en gran medida las diferencias en el grado de supresión ovárica observado entre los dos primeros años de utilización de implantes Norplant y los tres últimos, incluso en ausencia de una variación significativa de las concentraciones totales de levonorgestrel.
Similar content being viewed by others
References
SivinI. International experience with Norplant and Norplant-2 contraceptives. Stud Fam Plann. 1988;19:81–94.
KammenEvan, ThijssenJHH, RademakerB, SchwarzF. The influence of hormonal contraceptives on sex hormone binding globulin (SHBG) capacity. Contraception. 1975;11:53–9.
VictorA, JohanssonEDB. Effects of d-norgestrel induced decreases in sex hormone binding globulin capacity on the d-norgestrel levels in plasma. Contraception. 1977;16:115–23.
CekanSZ, JiaM, LandgrenBM, DiczfalusyE. The interaction between sex hormone binding globulin and levonorgestrel released from vaginal rings in women. Contraception. 1985;31:431–39.
AffandiB, CekanSZ, BoonkasemsantiW, SamilRS, DiczfalusyE. The interaction between sex hormone binding globulin and levonorgestrel released from Norplant, an implantable contraceptive. Contraception. 1987;35:135–45.
OlssonSE, OdlindV, JohanssonEDB, NordstromML. Plasma levels of levonorgestrel and free levonorgestrel index in women using Norplant implants or two covered rods (Norplant-2). Contraception. 1987;35:215–28.
WeinerE, JohanssonEDB. Plasma levels of d-norgestrel, estradiol and progesterone during treatment with silastic implants containing d-norgestrel. Contraception. 1976;14:81–91.
MooreDE, RoyS, StanczykFZ, MishellDR. Bleeding and serum d-norgestrel, estradiol and progesterone patterns in women using d-norgestrel subdermal polysiloxane capsules for contraception. Contraception. 1978;17:315–28.
ShaabanMM, El-NasharIM, GhaneimahSA, GomaaAA, SalahM, Abdel-AleemAM. Hormonal changes during the first year of use of subdermal levonorgestrel implants, Norplant. Contraception. 1984;30:391–405.
CroxattoHB, DiazS, PavezM, MirandaP, BrandeisA. Plasma progesterone levels during long-term treatment with levonorgestrel silastic implants. Acta Endocrinol. 1982;101:307–11.
BracheV, FaundesA, JohanssonE, AlvarezF. Anovulation, inadequate luteal phase and poor sperm penetration in cervical mucus during prolonged use of Norplant implants. Contraception. 1985;31:261–73.
BracheV, Alvarez-SanchezF, FaundesA, TejadaAS, CochonL. Ovarian endocrine function through five years of continuous treatment with Norplant subdermal contraceptive implants. Contraception. 1990;41:169–77.
BondA, DavisC. Sex hormone binding globulin in clinical perspective. Acta Obstet Gynecol Scand. 1987;66:255–62.
WeinerE, JohanssonEDB. Plasma levels of d-norgestrel, estradiol and progesterone during treatment with Silastic implants containing d-norgestrel. Contraception. 1976;14:81–92.
RosnerW. A simplified method for the quantitative determination of testosterone-estradiol binding globulin activity in human plasma. J Clin Endocrinol Metab. 1972;34:983–88.
OdlindV, ElamssonK, EnglundD, VictorA, JohanssonEDB. Effects of estradiol on sex hormone binding globulin. Acta Endocrinol. 1982;101:248–53.
CroxattoHB, DiazS, MirandaP. Plasma levels of levonorgestrel in women during longterm use of Norplant. Contraception. 1981;23:197–209.
AlvarezF, BracheV, FaundesA, JohanssonEDB, OdlindV, NashH. Levonorgestrel plasma levels during continuous administration with different models of subdermal implants. Contraception. 1983;27:123–30.
RobertsonDN, SivinI, NashH, BraunJ, DinhJ. Release rates of levonorgestrel from Silastic capsules, homogeneous rods and covered rods in humans. Contraception. 1983;27:483–95.
LandgrenBM, JohannissonE, MasironiB, DiczfalusyE. Pharamacokinetic and pharmacodynamic investigations with vaginal devices releasing levonorgestrel at a constant, near zero order rate. Contraception. 1982;26:567–85.
OlssonSE, BakosO, LindgrenPG, OdlindV, WideL. Ovarian function during use of subdermal implants releasing low doses of levonorgestrel. Br J Fam Plann. 1990;16:88–93.
BarbosaI, BakosO, OlssonSE, OdlindV, JohanssonEDB. Ovarian function during use of a levonorgestrel-releasing IUD. Contraception. 1990;42:51–66.
ShoupeD, HorensteinJ, MishellDR, LacarraM, MedearisA. Characteristics of ovarian follicular development in Norplant users. Fertil Steril. 1991;55:766–70.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Brache, V., Alvarez-Sanchez, F., Faundes, A. et al. Free levonorgestrel index and its relationship with luteal activity during long-term use of Norplant implants. Adv Contracept 8, 319–326 (1992). https://doi.org/10.1007/BF02042590
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02042590