Abstract
Besides the coagulation, where the body digests the necrotic tissue and direct evaporation of tissue, the photoablation effect turns out to be very important in tissue removal.
In the case of high tissue absorption the process channels in photoablation can either be photochemical (bond breaking) or fast thermal. In the case of transparent media, a plasma formation due to high irradiances and an optical breakdown is necessary for ablation or photodisruption.
All the process channels lead to a fast microscale explosion and to Shockwaves. For soft tissue the main process channel is the fast thermal explosion.
Assuming that tissue will be disintegrated, if the energy deposited within a single laser pulse is larger than a material specific threshold, the thresholds for the radiant exposure and ablation rates respectively can be calculated.
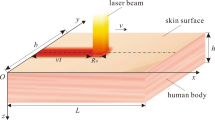
There is a large difference, whether the laser radiation is applied to the tissue surface in noncontact or through a fibre in contact. In contact the ‘fast thermal explosion’ happens in a closed chamber and hence the photohydraulic effect will support the photoablation.
The thermally damaged zone in the surrounding tissue depends on the optical penetration depth mainly in cases that the pulse duration is shorter than a critical time given by the heat conductivity. Pulsed lasers can be used ‘non-thermally’ only if the average power is less than a tenth of a watt. With a higher amount of average power a pulsed laser will act comparable to a cw laser.
Similar content being viewed by others
References
Müller G, Berlien H-P. Lasers in medicine-technical state and prospects. In:Lasers in Cardiovascular Diseases, International Symposium, Baden, Vienna, EBM, 1986:9–13
Boulnois J-L. Photophysical processes in recent medical laser developments: a review.Lasers Med Sci 1986,1:47–64
Srinivasan R. Self-developing photoetching of poly films by far ultraviolet excimer, laser radiation.App Phys Lett 1982,4(6):576–8
Sliney D. Laser-tissue interactions.Clin Chest Med 1985,6:203–8
Berlien HP, Müller G.Angewandte Lasermedizin, Lehr- und Handbuch für Praxis und Klinik. Ecomed, Landsberg, 1989
Star W. Comparing the P3-approximation with diffusion theory and with Monte Carlo calculations of light propagation in a slab geometry. In:Dosimetry of Laser Radiation in Medicine and Biology. SPIE Institutes for Advanced Optical Technologies, 1989,IS5:146–54
Müller G, Schaldach B. Basic laser tissue interaction. In:Safety and Laser Tissue Interaction, Advances in Lasermedicine II. Ecomed, Landsberg, 1989:17–25
Bloembergen N. Laser-induced electric breakdown in solids.J Quant Electr 1974,QF-10(3):375–86
Harnoss B-M, Kar H, Zühlke H et al. A comparative study on the physical aspects of the ablation behavior of short-pulsed laser in arteriosclerotic vessels in vitro.Lasers Surg Med 1990,6(3): 105–10
Walsh J, Deutsch T. Er:YAG laser ablation of tissue: measurement of ablation rates.Lasers Surg Med 1989,9:327–37
Walsh J, Deutsch T. Pulsed CO2 laser tissue ablation: measurement of the ablation rates.Lasers Surg Med 1988,8:264–75
Müller G, Berlien H-P, Biamino B et al. Photoablation threshold of human aorta as a function of wavelength. In:Laser Optoelectronics in Medicine, Proceedings of the 7th Congress of the International Society for Laser Surgery and Medicine, Springer, 1988:38–41
Kar H, Dörschel K, Müller G et al. Optimization of the coupling of excimer laser radiation (308 nm) into Q-Q fibres ranging from 200–600μm core diameter. InOptical Fibers in Medicine IV, Proceedings of SPIE, 1989,1067:223–32
Taylor R. Effect of optical pulse duration on the XeCl laser ablation of polymers and biological tissue.CLEO 1987, 268–9
Yeh J. Laser ablation of polymers.J Vac Sci Technol 1986,A4(3):653–8
Dörschel K, Müller G. Dosimetry for photoablation technique. In:Dosimetry of Laser Radiation in Medicine and Biology, SPIE Institutes for Advanced Optical Technologies, 1989,IS5:146–54
Hibst R, Keller U. Experimental studies of the application of the Er:YAG Laser on dental hard substances: I. Measurement of the ablation rate.Lasers Surg Med 1989,9:338–44
Zweig A, Weber H. Mechanical and thermal parameters in pulsed laser cutting of tissue.IEEE J Quant Electr 1987,QE23(10):1787–93
Rox R, Anderson BS, Parrisch JA. The optics of human skin.J Invest Dermatol 1981,77:13–9
Esterowitz L, Hoffman CA, Tran DC et al. Angioplasty with a laser and fiber optics at 2.94μm. In:Optical and Laser Technology in Medicine, SPIE 1986, 605:32–6
Küper S, Stuke M. Femtosecond uv excimer laser ablation.Appl Phys B 1987,44:199–204
Jaques S. Time resolved propagation of ultrashort laser pulses with turbid tissue.Appl Opt 1989,28:2223–9
Shrinivasan R, Casey K. Sub-nanosecond probing of the ablation of soft plaque from arterial wall by laser pulses delivered through a fiber.IEEE J Quant Electr 1991, to be published
Grothues-Spork M. Vergleich der knochenheilung nach sägeosteomie, CO2-laserosteomie und excimerlaserosteomie am röhrenknochen des kaninchen. Dissertation, Freie Universität, 1990
Walsh J, Flotte T, Deutsch T. Er:YAG laser ablation of tissue: effect of pulse duration and tissue type on thermal damage.Lasers Surg Med 1989,9:314–26
Furzikov N. Different lasers for angioplasty: termooptical comparison.IEEE J Quant Electr 1987,QE-23:1751–5
Müller-Stolzenburg N, Buchwald HJ, Müller G et al. In-vitro Untersuchungen zur refraktiven hornhautchirurgie mit dem excimer-laser über glasfaser.Fortschritte der Ophtalmologie 1989,86:592–6
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Müller, G., Dörschel, K. & Kar, H. Biophysics of the photoablation process. Laser Med Sci 6, 241–254 (1991). https://doi.org/10.1007/BF02030877
Issue Date:
DOI: https://doi.org/10.1007/BF02030877